Published online Aug 21, 2005. doi: 10.3748/wjg.v11.i31.4800
Revised: October 5, 2004
Accepted: October 11, 2004
Published online: August 21, 2005
AIM: To observe different histomorphologic changes of ulcerative colitis (UC) rats that were treated with four regulating-intestine prescriptions (FRIP), to investigate the curative effects of FRIP and to analyze their treatment mechanism.
METHODS: The UC rat model was made by the method of 2,4-dinitro chloro benzene (DNCB) immunity and acetic acid local enema. Ninety-eight SD rats were randomly divided into seven groups, namely, the normal control group, model group, salicylazosulfapyridine (SASP) group, Wumeiwan (WMW) group, Baitouwengtang (BTWT) group, Senglingbaishusan (SLBSS) group, and Tongxieyaofang (TXYF) group. Each group had 14 rats (with equal ratio of male and female). The six animal model groups of UC -SASP, TXYF, WMW, BTWT, SLBSS, TXYF-were treated by distilled water except the normal control group. Changes of the rat’s general conditions after treatment were respectively observed, the colon tissue damage scores were given out, the pathology of colonic mucosa and changes of ultrastructure were analyzed.
RESULTS: Different pathological changes on histology were shown after treatment by FRIP. The colon tissue damage score in model group was higher than that of FRIP groups and SASP group (q = 4.59, 4.77, P<0.05 or q = 5.48, 6.25, 5.97, P<0.01). The scores of WMW group, BTWT group and SLBSS group were lower than that of SASP (q = 4.13, P<0.05 or q = 5.31, 5.12, P<0.01). There was no remarkable difference between the damage score of TXYF group and SASP group (q = 3.75, P>0.05). In addition, some apoptosis cells were found in the pathologic control group.
CONCLUSION: The model made with DNCB and acetic acid was successful, and FRIP had better curative effect and WMW was the best curative effect, BTW, SLBSS and TXYF were similar to SASP, and we discovered that apoptosis was possibly related to UC.
- Citation: Fan H, Qiu MY, Mei JJ, Shen GX, Liu SL, Chen R. Effects of four regulating-intestine prescriptions on pathology and ultrastructure of colon tissue in rats with ulcerative colitis. World J Gastroenterol 2005; 11(31): 4800-4806
- URL: https://www.wjgnet.com/1007-9327/full/v11/i31/4800.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i31.4800
Ulcerative colitis (UC) is a non-specific inflammatory intestinal disease. The pathogenesis of UC is affected by a variety of factors, but its pathogenesis is still unknown at present[1]. A rat model of UC was established by the methods of DNCB immunity and acetic acid local enema. This subject is about the treatment effect of four regulating-intestine prescriptions (FRIP) by making rat model of UC, especially they were observed by scoring the gross morphologic damage and the change on the pathological section of colon tissue under light and electron microscope by treating with traditional Chinese medicine (TCM), and compared the different curative effect of Wumeiwan (WMW) group, Baitouwengtang (BTWT) group, Senglingbaishusan (SLBSS) group and Tongxieyaofang (TXYF) group.
Herbs in FRIP (WMW, BTWT, SLBSS, TXYF) and their quantity are as follows: WMW: 16 g dark plum, 6 g asarum herb, 10 g dried ginger, 16 g Chinese goldthread, 4 g Chinese angelica root, 6 g aconite root, 4 g pricklyash peel, 6 g cassia twig, 6 g sun-dried ginseng, 6 g bark of cork tree; BTWT: 30 g Chinese pulsatilla root, 24 g bark of amur corktree, 10 g Chinese goldthread, 24 g ash bark; SLBSS: 10 g pulp of lotus seed, 10 g coix seed, 10 g dried amomum fruit, 10 g balloon flower root, 15 g bean of white hyacinth, 20 g white Tuckahoe, 20 g sun-dried ginseng, 20 g licorice root, 20 g big head atractylodes rhizome, 20 g Chinese yam; TXYF: 30 g parched white atractylodes rhizome, 20 g white peony root, 15 g dried old orange peel, 20 g ledebouriella root.
Salicylazosulfapyridine (SASP) with batch no. 200111002 is produced by Shanghai Sanwei Pharmaceutical Company (250 mg/tablet).
TNF-α ISH detection kit, ISH special cover glass, DBA chromogenic kit, poly-L-lysine, DEPC and 20% glycerin were supplied by Wuhan Boster Biological Technology Co., Ltd.
Transmission electron microscope (Hitachi H-600), photomicroscope (Japan), ultramicrotome (LKB-V), magnifier and microscope, etc., were used.
Ninety-eight SD rats (male rats and female rats separately account for 50% and a rat weighed 30050 g) were supplied by Test Animal Center of Tongji Medical School, Huazhong University of Science and Technology. They were raised in the SPF environment (constant temperature, humidity and sterilized water, food and padding) and acclimatized to the surrounding for 7 d before the experiments.
Animal groups Ninety-eight SD rats (male rats and female rats separately account for 50%) were randomly divided into seven groups as males and females, and each group contained 14 rats (male rats and female rats separately account for 50%), of which group 7 was normal group. Groups 1-6 were modeled, which were respectively WMW group, BTWT group, SLBSS group, TXYF group, SASP group, and model group. Body weight of rats in each group showed no significant difference on statistics (P>0.05).
Preparation of the animal model Model of UC rat was established with 2,4-dinitro chloro benzene (DNCB) immunity and acetic acid local enema[1-5]. After hair on the rats nape was removed with Na2S of 100 g/L, 0.25 mL acetone solution with DNCB content of 20 g/L (five drops) was dripped on the rats back once a day and continuously dripped for 14 d. On the 15th d, a Φ 3-mm urinary catheter was put into at 8 mm of a rat’s colon via its anus to fill 0.25 mL ethanol containing 0.1% DNCB. On the 16th d, 2 mL 8% acetate solution was filled in the same position. After accurately timing for 10 s, this position was flushed with 5 mL physiological saline. After that, they were fed for 2 wk, to continue observing the rats stool characters, dietetics, hair and activity conditions, etc., every day. It could be seen from observation that the rats gradually produced typical symptom of UC active period. After 30 d, the modeling was finished. After modeling was finished (after the 30th d), two rats were randomly taken in each group and their colons were examined after they were killed to pathologically confirm a series of changes occurring in their colons such as hyperemia, hydrops, inflamed cellular infiltration, crypt abscess, fewer goblet cells, body of gland destroyed and aphthous formed.
Means for drugs For each rat in WMW group, BTWT group, SLBSS group, TXYF group, gastric lavage was conducted respectively with 3 mL prepared WMW liquid (0.515 g/mL), BTWT liquid (0.562 g/mL), SLBSS liquid (0.987 g/mL) and TXYF liquid (0.216 g/mL) once a day. For each rat in SASP group, gastric lavage was conducted with 3 mL SASP suspension (0.026 g/mL) liquid once a week. For each rat in model control group and normal group, gastric lavage was conducted with 3 mL distilled water. The drug feeding period was 15 d.
Collection and treatment of specimens After the feeding of drugs in all groups of rats ended, they were weighed and killed by the mode of cutting off their heads. After that, they were immediately dissected to take 6-8 mm colons upward at 2 mm of the anus. The intestine cavities were opened along the longitudinal axis of the intestinal mucosa and cleaned thoroughly with 0.9% saline and pure water, and assigned a code number. Then they were spread on the wax plate with the intestinal mucosa pointing upward. After they were fastened with the pins, occurring conditions of inflammation and ulcer were observed with a dissecting microscope. The colon was immediately examined under a stereomicroscope and any visible damage was scored on a 0-5 scale (Table 1).
| Score | Gross morphology |
| 0 | No damage |
| 1 | Localized hyperemia with no ulcers |
| 2 | Linear ulcers with no significant inflammation |
| 3 | Linear ulcers with inflammation at one site |
| 4 | More site of ulcers and inflammation, the size of ulcers <1 cm |
| 5 | Multiple inflammation and ulcers, the size of ulcers≥1 cm |
After modeling was finished (30 d), two rats were randomly selected from each group and killed by the mode of cutting off their heads to take part of the intestine tissues, which were immobilized with 40 g/L formaldehyde, embedded with paraffin, pathological section was taken and HE staining was performed. And then, colon conditions after modeling were observed and investigated.
After ending of the above tests (45 d), a small piece of colon tissue (3 mm) was taken from the colon of each rat. They were immobilized with 40 g/L formaldehyde (grouped and numbered with the penicillin bottles), embedded with paraffin, pathological section was taken and HE staining was performed. And then, pathological changes in each group of colons were observed (the above work was finished with the help of Pathology Department of Hubei Hospital of Traditional Chinese Medicine).
A rat was randomly selected in each group and the above procedures were executed until cleaning procedure. The colonic mucosa with ulcer was taken immediately and cut into 1-mm bits, which was immobilized with 2.5% glutaraldehyde, washed with 1% paraformaldehyde and immobilized after it was put in 1% osmic acid. Then, they were dehydrated in steps with ethanol and acetone, embedded with vegetable wax, cut into super-thin sections and doubly stained with uranium acetate and lead nitrate. After that, they were observed with a transmission electron microscope (finished with the help of Electron Microscope Department of Medical School of Wuhan University).
The weights of rats and tissue damage scores were expressed as mean盨D, and analyzed with the Student’s t-test or F test (q test).
The study of the rats in the model had symptoms of mucous thin stool after about 2 wk and worsened gradually. After about 4 wk, the symptoms were more serious and some symptoms such as pus and blood stool, thinner, less weight, hair having no gloss, significantly less appetite, intolerance of cold and action and less movement occurred. After gastric lavage was conducted with FRIP and SASP, their symptoms were improved differently (no statistical analysis except for weights). Weight changes are shown in Table 2.
The degree of colonic mucosal damage in rats of FRIP was scored according to the criteria in Table 1. The colon tissue damage score in model group was higher than that of FRIP groups and SASP group (P<0.05 or P<0.01). The scores of WMW group, BTWT group, and SLBSS group was lower than that of SASP (P<0.05 or P<0.01). There was no remarkable difference between the damage score of TXYF group and SASP group (P>0.05). The scores were roughly given out according to the inflammation and injury level, observation results of which are shown in Table 3.
| Group | Case (n) | Scoring the grossmorphologic damage |
| Normal control group | 12 | 0b |
| Model group | 10 | 5.5±0.45 |
| SASP group | 9 | 3.8±0.39a |
| WMW group | 11 | 1.8±0.34b,d |
| BTWT group | 10 | 2.5±0.38b,d |
| SLBSS group | 9 | 1.9±0.35b,c |
| TXYF group | 10 | 3.7±0.47a |
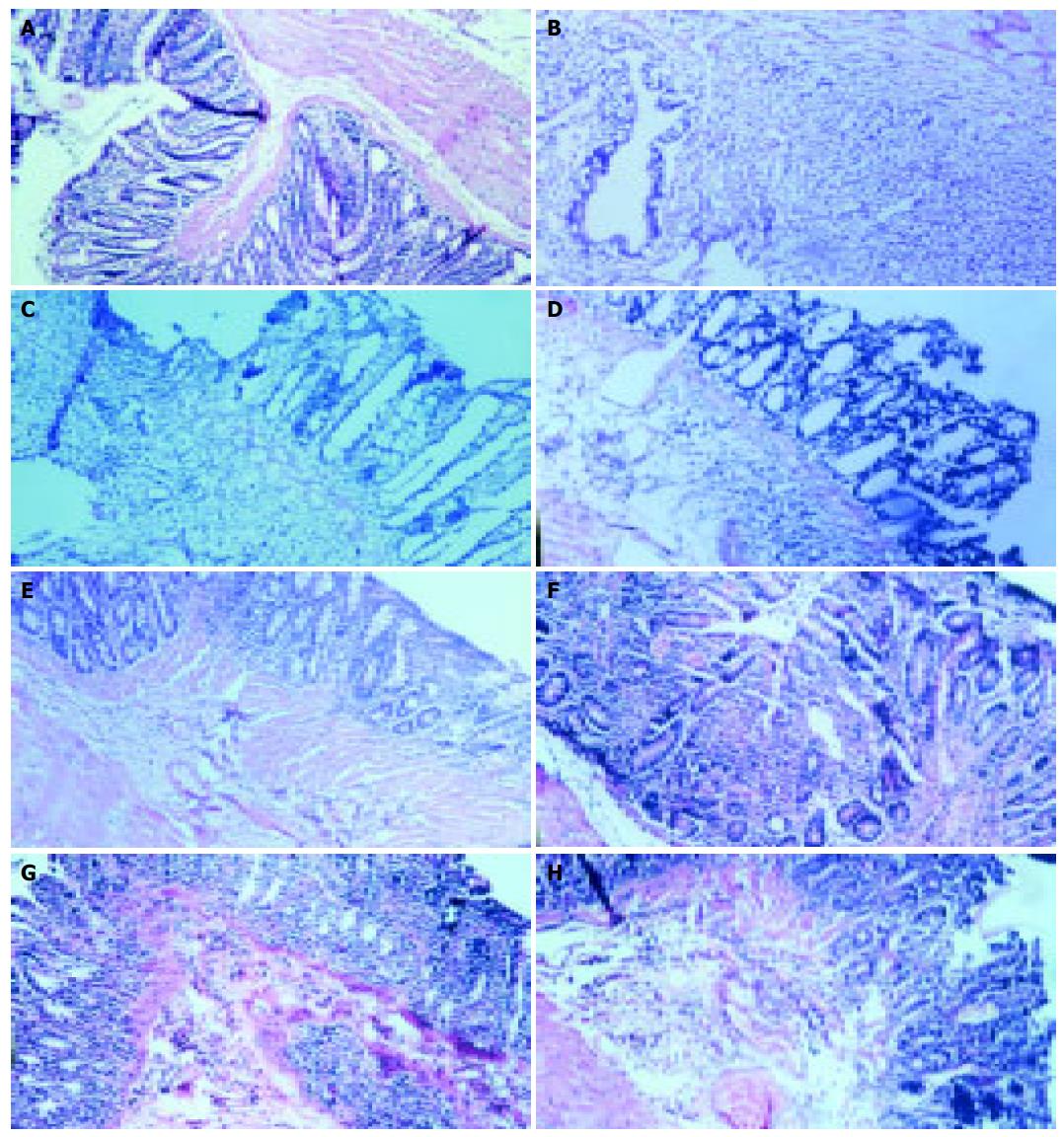
Normal control group: The colonic mucosa of rats was in good condition without inflammatory cell infiltration or ulceration of mucosa; the epithelial mucosae was intact and continuous; the bodies of gland arranged regularly with clear structure and active secreting function; the epithelial mucosae, the blood vessel in the membrana propria and fibers were normal; muscularis had no abnormal conditions. Model group: The colonic mucosa of the rats showed erosion and ulcers; the most of mucosa produced coloboma and some produced deep and large erosions, mucous gland bodies were destroyed; remaining mucosa was hyperemic and dropsical and formed polyp-like appearance (false polyp) due to hyperplasia; a lot of inflammatory cells (lymphocytes, plasma cells, and macrophages) infiltrated; some cells were scattered and were in multiplication conditions (more plasma, large nucleus, and sparse chromatin); mucous layer became thinner and the lamina propria beneath the mucosa showed local hyperemia, dropsy, and fiber hyperplasia. SASP group: The epithelial mucosae of the rat colon produced the local defects; the bodies of gland arranged less regularly with slight hyperemia beneath the mucosa and more inflammatory cells infiltrated. WMW group: The epithelial mucosae of the rat was basically sound; the bodies of gland arranged more regularly without significant hyperemia beneath the mucosa; a few inflammatory cells infiltrated. BTWT group: The epithelial mucosae of the rat was basically sound; the bodies of gland arranged more regularly without significant hyperemia beneath the mucosa; and inflammatory cell infiltration could be seen. SLBSS group: The epithelial mucosae of the rat was basically sound; the bodies of gland arranged more regularly without significant hyperemia beneath the mucosa; and a few inflammatory cell infiltration could be seen. TXYF group: The epithelial mucosae of the rat was less sound; the bodies of gland arranged less regularly with significant hyperemia beneath the mucosa; and inflammatory cell infiltration could be seen (Figures 1A-H).
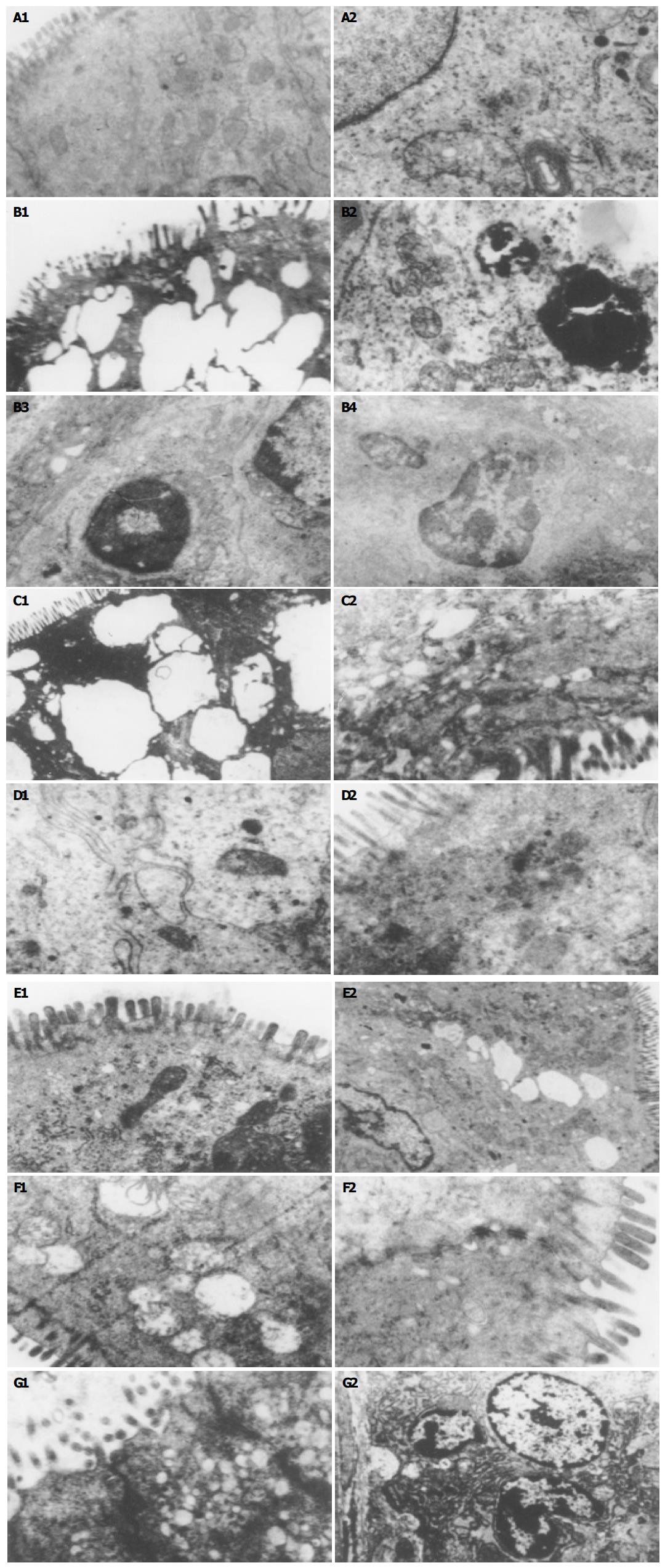
Normal control group: The microvilli on the surface of the mucosal epithelium of the rat colon was integral with neat arrangement, identical sizes, and regular mitochondrion shape and showed approximate roundness and ellipse, inner matrixes of which were of medium density; endoplasmic reticulum and nucleus were all up to snuff; epithelia linked tightly; space between cells was found to be wider (normal linking); the intestine gland was composed of the goblet cells. Model group: The microvilli on the surface of the mucosal epithelium of the rat colon were sparse, became shorter and irregularly curled with visible vacuoles, even epithelium cell membrane produced defects; organelles became fewer; cytoplasm liquefied and dissolved; inner matrixes in the mitochondria were clear with fewer inner cristae and significant swelling; endoplasmic reticulum expanded; chromatic agglutination and pyknosis could be seen; nucleoplasm proportion became less, some congregated beneath karyolemma and showed gobbet with clear boundaries, even apoptosis corpusculum, karyo-pyknosis, and lymphocyte infiltration could be seen. SASP group: The microvilli on the surface of the mucosal epithelium of the rat colon partly dropped off and became less regular; mitochondria shape became less regular and some were with slight swelling with destroyed cytoarchitecture; fat particles and endoplasmic reticulum expanding could be seen. WMW group: The microvilli on the surface of the mucosal epithelium of the rat colon were basically intact with normal cytoarchitecture; after observing under the electron microscope (12 000), it could be found that their endoplasmic reticulum and mitochondria were clearer, and the organelles such as mitochondria and elder with cytoryctes could be seen with clear cytoarchitecture as well as dropping-off of the microvilli could be seen. BTWT group: The microvilli on the surface of the mucosal epithelium of the rat colon was basically regular and intact; mitochondria in the cytoplasm was abundant with regular mitochondria and showed approximate roundness or ellipse; the matrixes were basically even. SLBSS group: The microvilli on the surface of the mucosal epithelium of the rat colon were less irregular and a few microvilli dropped off; mitochondria were swelling with normal cytoarchitecture. TXYF group: More microvilli on the surface of the mucosal epithelium of the rat colon dropped off or they were sparse and expanding; staining of nucleus was a little dark; destroyed cytoarchitecture and wider chromatin margin could be seen; cellular nucleus became smaller (Figures 2A-G).
The results of pathological sections under electron microscope showed that UC was related to apoptosis and the curative effect of WMW was better than that of the other groups and SASP groups.
Normal colonic tissue consists of mucous membrane layer (including epidermis layer, lamina propria, muscular layer of mucous membrane), mucous membrane substrate layer, muscular layer (inner ring and outer race), chorion layer and so on. Pathological changes of UC affects mucous membrane and substrate layer. The best characteristic changes of histology included diffuse and severe inflammatory cell infiltration in all layers of inhesion membrane, serious and comprehensive mucous configuration abnormity, crypt lymph in recess (namely crypt abscess), inhesion membrane with a great number of plasma cells, lymphocyte, mononuclear cells, neutrophils and eosinophils infiltration. Because of inflammatory irritation, there were epithelial hyperplasia of gland, which were shown as goblet cells and mucilage in the body of the gland reduced but nucleus expanded and nuclear fusion increased in various extents. Cytoplast had a liking for alkalescence; epithelial hyperplasia of gland sometime became false compound. Further observation showed that the capillary vessel dilatation caused congestion and blood vessel swelling further. In a serious case, the inflammation could develop into the mucous membrane substrate layer, even perforation, which broke to form the pilosity granular light ulcer or merged into various sizes and shapes to become irregular ulcer. Serious cases had large range of mucous membrane peeling. More normal mucous membrane between the ulcer turn into prowling form (there are boundary between sick mucous membrane and normal mucous membrane), taking on hydronics and polyp (false polyp), so the mucous membrane took the form of particle coarsely, the blood vessels were so fuzzy and fragile that they were apt to bleed with purulence secretion when touched. But there was seldom involvement of the deep layer of intestine wall, so the incrassation and fibrosis intestine wall were not remarkable, but few breaking out types and poisoning type colon cases come out of a hole because of piercing through intestine wall.
In recent years, many studies to the change of colonic mucus were carried out. It was suggested that it might be the prodromal change of carcinoma of large intestine. As we all know, UC is a pre-cancerous lesion of colon carcinoma. The mucosa in this region also showed certain histologic characteristics: the goblet cells in the glandular body decreased remarkably or disappeared with appearance of simple columnar cells, which lack mucin secretion. The lumen of some mucosal glands became dilated, branched or irregularly arranged. We found that the important characteristic of UC was inflammation in this experiment and cell apoptosis under electron microscope. We also found that the presentation was hyperemia and edema with a great number of plasma cells, lymphocytes, mononuclear cells, neutrophils, and eosinophils infiltration[10-12], the characteristic that pathology changes and ultrastructure was different in all groups was associated with the treatment.
This model made with DNCB and acetic acid was successful by the changes of symptoms and signs, damage scores of the colonic mucosa and the pathology sections and ultrastructure of colon tissue. At the same time, their symptoms and signs and pathology differently improved after treatment (not statistically significant, P>0.05). In this study, we discovered that FRIP had better curative effect on UC and WMWs was the best, BTWs and SLBSSs were the second of best. TXYFs were worst (they were as same as SASPs). At the same time, this implies, that we must have BianzhengLunzhi in the treatment of UC[13]. According to TCM, UC belongs to the category of 揦iouxili (diarrhea), the mucosal inflammatory lesions result from not only deficiency and hypofunction of spleen and stomach, but also accumulation of damp heat, the pathogenesis of UC is similar with the prescription characteristic of WMW. Therefore, in this study, the best curative effect was achieved by the treatment of the WMW. The results showed that this WMW had the function of strengthening the spleen and reinforcing Qi and eliminating damp-heat pathogen, promoting flow of Qi and blood, improving luminal blood circulation, and was helpful for hemostasis and the absorption of inflammatory products, eventually attained the goal of the neogenesis of granulated tissue in the region of ulceration, and the repair of mucosal epithelium. But BTW concentrated on eliminating damp-heat pathogen, SLBSS was good at strengthening the spleen and reinforcing Qi, the former had the function of reducing the excess, the latter had the function of reinforcing the deficiency, so two formulae of BTW and SLBSS had some therapeutic effects, and they were the second curative effect; the prescription characteristic of TXYF, which had the function of smoothing the liver-Qi to normalize the stomach, was different with the pathogenesis of UC and it had the worst curative effect.
In addition, we discovered that apoptosis was possibly related to UC[13] and FRIP could decrease apoptosis, block inflammation and induce remission.
Science Editor Zhu LH and Guo SY Language Editor Elsevier HK
| 1. | Bicks RO, Rosenberg EW. A chronic delayed hypersensitivity reaction in the guinea pig colon. Gastroenterology. 1964;46:543-549. [PubMed] |
| 2. | Li Y. Methods on making rat experiment model of ulcerative colitis. New Drugs TCM Clinical Pharmacol. 1999;10:120-122. |
| 3. | Jiang XL, Quan QZ, Wang D, Sun ZQ, Wang YJ. A new ulcerative colitis model induced by compound method and the change of immunity and ultrastructures. Shijie Huaren Xiaohua Zazhi. 1999;7:381. |
| 4. | Jiang XL, Quan QZ, Wang D, Sun ZQ, Wang YJ, Qi F. Effect of heartleaf houttuynia herb on colonic pressure in rats with ulcerative colitis. Shijie Huaren Xiaohua Zazhi. 1999;7:786. |
| 5. | Fan H, Qiu MY. Evaluating on making rat experiment model of ulcerative colitis. Chinese Archives Traditional Chinese Med. 2004;22:865-866. |
| 6. | Wallace JL, Keenan CM. An orally active inhibitor of leukotriene synthesis accelerates healing in a rat model of colitis. Am J Physiol. 1990;258:G527-G534. [PubMed] |
| 7. | Zheng HB, Hu HY, Lu X, Ma GT. Morpholgical observation of intestine-clearing suppository in preventing and treating rats, ulcerative colitis. J Zhejiang College TCM. 2001;25:47-51. |
| 8. | Morris GP, Beck PL, Herridge MS, Depew WT, Szewczuk MR, Wallace JL. Hapten-induced model of chronic inflammation and ulceration in the rat colon. Gastroenterology. 1989;96:795-803. [PubMed] |
| 9. | Padol I, Huang JQ, Hogaboam CM, Hunt RH. Therapeutic effects of the endothelin receptor antagonist Ro 48-5695 in the TNBS/DNBS rat model of colitis. Eur J Gastroenterol Hepatol. 2000;12:257-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Tjandra K, Le T, Swain MG. Experimental colitis attenuates development of toxin-induced cholangitis in rats. Dig Dis Sci. 2002;47:1216-1223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Ji XL, Shen MS, Yin W. Key of Pathological Diagnosis on ulcerative colitis and colon desease. J Diag Pathol. 2002;9:245-247. |
| 12. | Nosalova V, Cerna S, Schunack W, Grandi D, Coruzzi G. Effects of (R)alpha-methylhistamine on experimental colitis. Inflamm Res. 2001;50 Suppl 2:S108-S109. [PubMed] |
| 13. | Fan H, Qiu MY, Mei JJ, Shen GX, Liu SL. Effect of Lichangsifang on cellular apoptosis and expression of the related regulatory genes in rats with ulcerative colitis. Shijie Huaren Xiaohua Zazhi. 2004;12:1119-1124. |