Published online Aug 14, 2005. doi: 10.3748/wjg.v11.i30.4764
Revised: June 13, 2004
Accepted: June 18, 2004
Published online: August 14, 2005
Biloma is an encapsulated bile collection outside the biliary tree due to a bile leak. It is occasionally found following traumatic liver injury or iatrogenic injury to the biliary tract, induced either during an endoscopic or surgical procedure. It is a rare complication of transcatheter arterial embolization (TAE). Although biloma can be shrunk by appropriate aspiration or drainage in majority of cases, we report a case of intrahepatic biloma following repeated TAE for hepatocellular carcinoma (HCC) and complicated by infection and intrahepatic stones. This particular constellation of problems has not been reported before and the intrahepatic stones need to be removed by percutaneous procedure.
- Citation: Chen MJ, Lin CC, Chang WH, Yang FS. Biloma following repeated transcatheter arterial embolization and complicated by intrahepatic duct stones: A case report. World J Gastroenterol 2005; 11(30): 4764-4765
- URL: https://www.wjgnet.com/1007-9327/full/v11/i30/4764.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i30.4764
A 69-year-old woman was diagnosed with cryptogenic liver cirrhosis 15 years ago, but had well-compensated liver function. In October 2000, she was found to have a 8-cm tumor in the left lobe of the liver. HCC was diagnosed on pathological examination. Surgical resection was not attempted because of the large size of the tumor and atrophy of the right lobe. Therefore, she was treated with transcatheter arterial embolization (TAE) and percutaneous ethanol injection (PEI). TAE was performed with 6 cm3 of iodized oil (lipiodol) injected through the catheter and embolization with gelfoam sponge. Four weeks after TAE, enhanced CT was used to access the effects. If the response was not satisfactory, pure ethanol was injected under ultrasound guidance. By May 2003, the patient received five courses of combined TAE and PEI. Her cirrhosis was assessed as Child-Pugh class A, and HCC was maintained at 7 cm in diameter. No major complications were noted till that point.
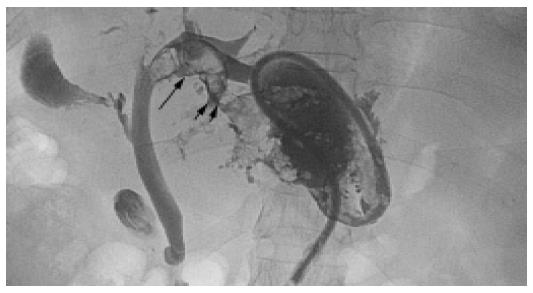
Three weeks after the sixth TAE procedure, the patient complained of nausea, epigastric pain, and poor appetite. She denied fever or chills. A tender mass was palpable in the epigastric area. Her bilirubin was elevated at 2.8 mg/dL. An abdominal CT disclosed an encapsulated fluid collection in the left lobe of the liver. Echo-guided aspiration of bile from the lesion confirmed the diagnosis of biloma. Several days later, the culture of the aspirated bile culture was reported as growing K. pneumoniae. On the same day, the patient developed fever and leukocytosis. She was treated with intravenous antibiotics, and a 10 F pig-tail catheter was placed percutaneously to drain the biloma. Two days later, contrast media was injected through the catheter for a fluoroscopic evaluation. A communication was found between the biloma and the left biliary tree (Figure 1). Small filling defects were seen in one dilated branch of the IHD, consistent with stones. Some of these fell into the biloma. The biloma drain continued to put out a large volume of bile along with sandy stones for 5 d, without any shrinkage the size of the cavity. However, the fever did subside. Concerned that the stones were preventing collapse of the biloma, we decided to remove the stones percutaneously. The fistula track was gradually dilated to 16 F by changing the drainage catheter. The IHD stones were removed with a basket over several sessions. Two months later, the biloma shrunk.
Biloma is occasionally found following traumatic liver injury or iatrogenic injury to the biliary tract, induced either during an endoscopic[1] or surgical procedure. Peripheral bile duct necrosis caused by microvascular damage and ductal stenosis after TAE might lead to a bile leak[2,3]. Our patient has already undergone five courses of TAE and PEI before, and the biloma developed 3 wk after the sixth TAE. We do not think that the PEI could directly influence this biloma, although there is one case report in the literature of a biloma after PEI[4]. The incidence of biloma after TAE in several series has been reported to be around 0.8-1.1%[5-7]. These often occurred only after more than five courses of TAE[5,6]. Recent reports indicate the advantage of the usage of embolization materials which have a suitable size only for the feeding artery, but largely for occlusion of bile duct microplexus. It is in terms of effective tumor embolization as well as prevention of possible complications.
Biloma is usually a simple cyst without septum. Percutaneous needle aspiration with chemical analysis could confirm the diagnosis. It may be asymptomatic or present with a variety of manifestations, such as gastric outlet obstruction, jaundice, or fever. The presentation depends on the size and location of the lesion and the presence or absence of infection. Asymptomatic patients may be treated conservatively. In a series reported by Kohno et al.[4], in 15 of 20 patients, the biloma shrank spontaneously during a 6-mo follow-up period. A biloma that fails to decrease in size should be drained, as infection is a common complication if the condition persists. If there is no communication with the biliary tree, and the proximal biliary tree has neither stricture nor stones, percutaneous drainage and intravenous antibiotics may achieve resolution. Intra-hepatic duct strictures may require insertion of a stent in order to relieve pressure that might reopen a tract to the biloma. However, IHD stones are often difficult to be removed. A biloma connected to a biliary tree containing stones has not been previously reported. It appeared in our patient that peripheral bile outflow was blocked by the IHD stones, causing a high pressure in biliary system and thus, led to a persistent bile leak. Given the difficulty of reaching IHD stones endoscopically, percutaneous removal of the stones seemed advisable, and ultimately, the biloma did shrink.
The proposed therapies for HCC, beyond TAE and PEI are increasing and include hepatic artery infusion of chemotherapy agents[8], microwave coagulation[9], and high frequency radioablation. Any of these may cause peripheral bile duct damage, so that it is conceivable that the incidence of biloma will increase. Clinicians must be aware of this possible complication. The prophylactic administration of antibiotics may be employed in these procedures, since biloma can be a result of focal infection. But the real necessity of prophylactic antibiotics remains to be identified.
Science Editor Wang XL Language Editor Elsevier HK
| 1. | Ranjeev P, Goh KL, Rosmawati M, Tan YM. Intrahepatic biloma: an unusual complication of cholangiocarcinoma treated endoscopically. Gastrointest Endosc. 1999;50:711-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Kobayashi S, Nakanuma Y, Terada T, Matsui O. Postmortem survey of bile duct necrosis and biloma in hepatocellular carcinoma after transcatheter arterial chemoembolization therapy: relevance to microvascular damages of peribiliary capillary plexus. Am J Gastroenterol. 1993;88:1410-1415. [PubMed] |
| 3. | Koda M, Murawaki Y, Mitsuda A, Oyama K, Okamoto K, Idobe Y, Suou T, Kawasaki H. Combination therapy with transcatheter arterial chemoembolization and percutaneous ethanol injection compared with percutaneous ethanol injection alone for patients with small hepatocellular carcinoma: a randomized control study. Cancer. 2001;92:1516-1524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 4. | Kohno E, Chen S, Numata K, Nakamura S, Tanaka K, Endo O, Inoue S, Takamura Y. [A case of biloma: complication of percutaneous ethanol injection therapy for hepatocellular carcinoma]. Nihon Shokakibyo Gakkai Zasshi. 1992;89:2719-2724. [PubMed] |
| 5. | Chen C, Tsang YM, Hsueh PR, Huang GT, Yang PM, Sheu JC, Lai MY, Chen PJ, Chen DS. Bacterial infections associated with hepatic arteriography and transarterial embolization for hepatocellular carcinoma: a prospective study. Clin Infect Dis. 1999;29:161-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Chung JW, Park JH, Han JK, Choi BI, Han MC, Lee HS, Kim CY. Hepatic tumors: predisposing factors for complications of transcatheter oily chemoembolization. Radiology. 1996;198:33-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 259] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 7. | Sakamoto I, Aso N, Nagaoki K, Matsuoka Y, Uetani M, Ashizawa K, Iwanaga S, Mori M, Morikawa M, Fukuda T. Complications associated with transcatheter arterial embolization for hepatic tumors. Radiographics. 1998;18:605-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 168] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 8. | Seno H, Ito K, Kojima K, Nakajima N, Chiba T. Efficacy of an implanted drug delivery system for advanced hepatocellular carcinoma using 5-fluorouracil, epirubicin and mitomycin C. J Gastroenterol Hepatol. 1999;14:811-816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Shimada S, Hirota M, Beppu T, Matsuda T, Hayashi N, Tashima S, Takai E, Yamaguchi K, Inoue K, Ogawa M. Complications and management of microwave coagulation therapy for primary and metastatic liver tumors. Surg Today. 1998;28:1130-1137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 48] [Article Influence: 1.8] [Reference Citation Analysis (0)] |