Published online Aug 14, 2005. doi: 10.3748/wjg.v11.i30.4634
Revised: December 18, 2004
Accepted: December 21, 2004
Published online: August 14, 2005
AIM: To characterize the histochemical type and pattern of intestinal metaplasia (IM) adjacent to gastric cardia adenocarcinoma (GCA) and distal gastric cancer (GC) in Linzhou, Henan Province, China.
METHODS: Alcian-blue-periodic acid Schiff and high iron diamine-Alcian blue histochemical methods were performed on 142 cases of IM, including 49 cases of GCA and 93 cases of GC. All the patients were from Linzhou, Henan Province, China, the highest incidence area for both GCA and squamous cell carcinoma. Radio- or chemotherapy was not applied to these patients before surgery.
RESULTS: The detection rate of IM in tissues adjacent to GCA tissues was 44.9%, which was significantly lower than that in GC tissues (80.64%, P < 0.01). The rates of both incomplete small intestinal and colonic IM types identified by histochemistry in GCA tissues (31.82% and 63.64%, respectively) were significantly higher than those in GC (5.33% and 21.33%, respectively, P < 0.01).
CONCLUSION: IM in GCA and GC should be considered as a separate entity. Further research is needed to evaluate whether neoplastic progression of IM is related to its mucin profile in GCA.
- Citation: Gao SG, Wang LD, Fan ZM, Li JL, He X, Guo RF, Xie DL, He XW, Gao SS, Guo HQ, Wang JK, Feng XS, Ma BG. Histochemical studies on intestinal metaplasia adjacent to gastric cardia adenocarcinoma in subjects at high-incidence area in Henan, north China. World J Gastroenterol 2005; 11(30): 4634-4637
- URL: https://www.wjgnet.com/1007-9327/full/v11/i30/4634.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i30.4634
In China, epidemiologically, gastric cardia adenocarcinoma (GCA) shares a very similar geographic distribution with esophageal squamous cell carcinoma (SCC), especially in Linzhou (formerly Linxian County), Henan Province, north China, the highest incidence area of SCC in the world[1,2]. However, the incidence of adenocarcinoma arising from the distal stomach is very low in this area[3,4]. In the last two decades, the incidence of primary adenocarcinoma of the lower esophagus, esophagogastric junction and GCA has increased dramatically in North America and Western European countries[5-6]. In contrast, the incidence of gastric cancer (GC) has decreased steadily in recent years.
In Linzhou, China, GCA has been classified as esophageal cancer by the local registry for the past several decades, because of their similar clinical symptoms, such as dysphagia[1]. Approximately 60% of patients with dysphagia are found to have a diagnosis of SCC, the remaining 40% are found to have adenocarcinomas of the lower esophagus or gastric cardia[8]. A case-control study performed on patients with presumed distal esophageal or gastric cardia cancer in Linzhou found that one-third of all these tumors are adenocarcinomas of the gastric cardia[9].
The histogenesis and carcinogenesis for malignant transformation of GCA, however, are still not clear. Intestinal metaplasia (IM) is documented in the gastro-esophageal junction and cardia, but the etiology remains unclear[10,11]. It has been believed that IM is closely related with the distal stomach cancer[12]. However, whether IM is a premalignant lesion for GCA is still not clear. Studies on the histochemical features of IM arising from gastric cardia and distal stomach and their relationship are very limited. Thus, the present study was undertaken to characterize the histological and histochemical types of IM in tissues adjacent to GCA and GC from patients in Linzhou, a high-incidence area of SCC and GCA in north China with Alcian-blue-periodic acid Schiff (AB-PAS) and High Iron Diamine-Alcian blue (HID-AB) staining methods.
One hundred and forty-two surgically resected GCA and AC specimens were collected from Linzhou People’s Hospital, Linzhou Center Hospital and Yaocun Esophageal Cancer Hospital in Henan Province from 2000 to 2001. All the patients were from Linzhou, Henan Province, the highest incidence area of both GCA and SCC. There were 49 patients with GCA, including 26 males and 23 females with an average age of 59.96 ± 10.29 years (range 36-80 years) and 93 patients with GC, including 49 males and 44 females with an average age of 58.96 ± 9.38 years (range 33-82 years). None of the cases received chemotherapy or radiotherapy before surgery. The surgically resected specimens were immediately fixed in 85% ethanol, and embedded with paraffin. Ten to fifteen pieces of tissue adjacent to cancer foci were obtained from each sample, dehydrated routinely with graded ethanol, embedded with paraffin, and cut into 5-μm-thick sections. For each block, three slides were prepared, one slide was stained with hematoxylin and eosin (HE) for pathological diagnosis and another two slides were histochemically stained for histochemical analysis.
The protocols for AB-PAS and HID-AB staining established previously in our laboratory were used[11]. Briefly, for AB-PAS staining, the paraffin slides were deparaffinized with xylene. One hundred microliters of AB staining solution (Fluka Company) was added to the slides for staining in wet boxes for 20-30 min, washed with distilled water for 3-5 min; 100 mL 0.5% periodic acid solution was applied for oxidation for 10 min, washed with distilled water for 3-5 min; Schiff solution staining for 10 min, washed with distilled water for 5-10 min. Finally, the slides were sealed with neutral gum. For HID-AB staining (Sigma Company, USA), the paraffin slides were deparaffinized with xylene. The slides reacted with high iron diamine solution at room temperature for 24 h and then were washed with distilled water. One hundred microliters of AB solution was applied for staining in wet boxes for 20-30 min and washed with distilled water, 0.5% neutral red solution (No. 3 Reagent Factory, Shanghai) was stained for 1-2 min and then washed with distilled water for 3-5 min. Finally, the slides were sealed with neutral gum.
Based on the morphology and histochemistry findings, IM was classified as five types: complete intestinal IM, incomplete intestinal IM, complete colonic IM, incomplete colonic IM, and incomplete gastric IM (Table 1). In complete IM, the epithelial cells were composed of goblet cells, Paneth cells, mucous columnar cells, and absorptive cells; in incomplete IM, the epithelial cells were composed of goblet and mucous columnar cells.
| Types of IM | Histology | Histochemical staining | ||||
| Structure of glands | Columnar cell | Paneth cell | AB | PAS | HID | |
| Complete | Regular | - | + | + | - | - |
| Incomplete | Irregular | + | - | + | + | - |
| Complete colonic | Regular | - | - | + | - | + |
| Incomplete colonic | Irregular | + | - | + | + | + |
| Incomplete gastric | Irregular | + | - | - | + | - |
The data were processed with SPSS 8.0 and χ2 test was used for the difference among different IM types. P < 0.05 was considered statistically significant.
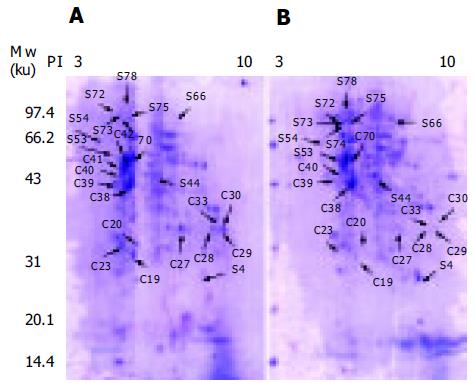
The histological analysis showed that the detection rate in both complete and incomplete IM adjacent to GCA (44.9%) was lower than that in both complete and incomplete IM adjacent to GC (80.64%, P < 0.01, Table 2). IM could be identified in a single acinus, or in several acini (Figure 1A).
| Incomplete IM | |||
| Type | Complete IM | Small intestinal | Colonic |
| n (%) | n (%) | n (%) | |
| GCA | |||
| (44.90%, 22/49) | 1/22 (4.55) | 7/22 (31.82) | 14/22 (63.64) |
| GC | |||
| (80.64%, 75/93) | 55/75 (73.33) | 4/75 (5.33) | 16/75 (21.33) |
By AB-PAS staining, complete type of IM was stained blue (Figure 1B), the incomplete type of IM was stained blue and red (Figure 1C), the gastric type of IM was stained red, the intestinal type of IM was stained blue. But, by HID-AB staining, the intestinal type of IM was stained blue (Figure 1D), the colonic type of IM was stained brown or black (Figure 1E).
The histochemical pattern and type of IM were different between GCA and GC and most types of IM in GCA were incomplete type (95.45%), especially in the incomplete colonic type (63.64%); In contrast, complete IM occurred more frequently in GC (73.33%, P < 0.01, Table 2). Incomplete colonic and small intestinal IM could be observed in the same microscopic field or different fields on the same sample. In other words, blue acid mucous and brown-black sulfuric acid mucous co-existed in one acinus in some cases. The detection rate of co-existence for both colonic and small intestinal types on the same slide was 22.73% (n = 5). IM mostly occurred in the deep glands of gastric cardia.
The present study showed that IM was a frequent event in gastric cardia non-cancerous tissue adjacent to GCA (44.9%) in Linzhou, Henan Province, the highest incidence area of SCC and GCA. Goblet cells were invariably identified on HE-stained specimens. Only 0.7% symptom-free subjects in Linzhou are identified with IM in gastric cardia biopsies[4]. These results suggest that IM may be a precancerous lesion of GCA in this area.
Another interesting observation in the present study is that incomplete type of IM, especially the colonic type, is the predominant form of IM found in the gastric cardia. In contrast, the complete type of IM is the major form of IM found in GC. These results suggest that IM in GCA and GC should be considered as a separate entity. In stomach, IM frequently forms at the antrum (22.9%) but rarely at the fundus (2.8%)[13]. Likewise, most GCs arise from the distal part of the stomach and infrequently from the near part. It is believed that GC correlates with IM closely, particularly with the intestinal type of GC based on the fact that the risk for GC and IM shares the same epidemiological characteristics[14]. It was reported that the incomplete IM in which columnar cells secrete sulfuric acid mucous relates with GC[12,15,16]. The present study indicated that the detection rate of IM adjacent to GCA was lower than that adjacent to GC. But the IM adjacent to GCA belonged to the incomplete IM, and the percentage of incomplete IM is much higher, suggesting that GCA correlates with incomplete IM closely and incomplete IM may be precancerous lesions of GCA. Reports with respect to the relationship between IM and GCA are inconsistent[17]. Further characterization of molecular changes of IM in nearby cancer foci and cancer tissue will shed light on the relationship of IM and GCA.
The prevalence of IM in gastric cardia is an under-studied subject, especially in symptom-free subjects at the high-risk area of GCA. Only 0.7% symptom-free subjects in Linzhou, Henan Province, the high incidence area for GCA are identified with IM in gastric cardia biopsy, which is much lower than that in gastric cardia tissue adjacent to GCA (64-folds lower, 44.9% vs 0.7%)[4]. The possibility for this difference may be that the prevalence of IM in symptom-free subjects is lower than that in GCA patients. Recent studies in Western countries indicate that IM in Barrett’s esophagus and at the gastroesophageal junction seems to occur more apparently in old subjects. GCA patients are usually 5-10 years older at the time of diagnosis than symptom-free subjects in the same area. Another reason may be due to the sampling procedure. IM occurs with a patchy, irregular distribution in flat mucosa that is usually invisible at endoscopy. Presently, we lack methods to target biopsy for IM lesions, the chance to identify IM lesions in small biopsy is much less than that in surgically resected GCA specimen. Methylene blue selectively stains specialized columnar epithelia in Barrett’s esophagus with a high accuracy. Chromoendoscopy with methylene blue stain may help to direct biopsies in subjects with IM in gastric cardia[17-19].
IM has been recognized as a key point in Barrett’s esophagus. Goblet cells are invariably identified on HE-stained Barrett’s esophagus. It has been hypothesized that Barrett’s adenocarcinoma follows the metaplasia-dysplasia-adenocarcinoma sequence[10]. At present, however, the importance of IM at gastric cardia remains unclear. Apparently, reflux esophagitis is not correlated with IM at gastric cardia in Chinese population. Chronic carditis may contribute to the development of IM at gastric cardia. Further research in large scale and long-term follow-up are needed to evaluate whether neoplastic progression of GCA is related to IM and its mucin profile.
The present study showed that incomplete IM and colonic IM coexisted in the same area or different areas of one sample. Some stomach glands presented blue acid mucous of intestinal IM and brown-black sulfuric acid mucous of colonic IM. The possible explanation is the multi-potent stem cells in the neck of gastric glands are to differentiate different types of epithelium due to the irritation of various initial agents, leading to different mucous reaction.
We would like to thank Dr. Zhe Sun and Dr. Xiao-Dong Lv for helpful discussions and preparation of this manuscript.
Science Editor Wang XL and Guo SY Language Editor Elsevier HK
| 1. | Wang LD, Zhou Q, Yang CS. Esophageal and gastric cardia epithelial cell proliferation in northern Chinese subjects living in a high-incidence area. J Cell Biochem Suppl. 1997;28-29:159-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 2. | Wang LD, Shi ST, Zhou Q, Goldstein S, Hong JY, Shao P, Qiu SL, Yang CS. Changes in p53 and cyclin D1 protein levels and cell proliferation in different stages of human esophageal and gastric-cardia carcinogenesis. Int J Cancer. 1994;59:514-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 76] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Wang LD, Zheng S. Mechanisms of human esophageal and gastric cardia cancer on the subjects in Henan,the high inci-dence area for esophageal canceer. Zhengzhou Daxue Xuebao. 2002;37:717-729. |
| 4. | Wang LD, Feng CW, Zhou Q, Chen YL, Li YX, Zhuang Y, Xie BH, Qiu SL, Liu BC, Zhao YZ. Analysis of the screening result of esophageal disease in high risk urban and rural areas of esophageal carcinoma. Henan Yike Daxue Xuebao. 1997;32:6-8. |
| 5. | Powell J, McConkey CC. Increasing incidence of adenocarcinoma of the gastric cardia and adjacent sites. Br J Cancer. 1990;62:440-443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 264] [Cited by in RCA: 279] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 6. | Blot WJ, Devesa SS, Kneller RW, Fraumeni JF. Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA. 1991;265:1287-1289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1287] [Cited by in RCA: 1149] [Article Influence: 33.8] [Reference Citation Analysis (0)] |
| 7. | Blot WJ, Devesa SS, Fraumeni JF. Continuing climb in rates of esophageal adenocarcinoma: an update. JAMA. 1993;270:1320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 198] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 8. | Wang LD, Gao WJ, Yang WC, Li XF, Li J, Zou JX, Wang DC, Guo RX. Preliminary analysis of the statistics on 3,933 cases with esophageal cancer and gastric cardia cancer from the subjects in people's Hospital of Linzhou in 9 years. Henan Yike Daxue Xuebao. 1997;32:9-11. |
| 9. | Li JY, Ershow AG, Chen ZJ, Wacholder S, Li GY, Guo W, Li B, Blot WJ. A case-control study of cancer of the esophagus and gastric cardia in Linxian. Int J Cancer. 1989;43:755-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 130] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Clouston AD. Timely topic: Premalignant lesions associated with adenocarcinoma of the upper gastrointestinal tract. Pathology. 2001;33:271-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Chen H, Wang LD, Fan ZM, Gao SG, Guo HQ, Guo M. The comparison study of the three histochemical staining meth-ods in gastric cardia intestinal metaplasia staining. Henan Yixue Yanjiu. 2003;12:10-13. |
| 12. | Conio M, Lapertosa G, Blanchi S, Filiberti R. Barrett's esophagus: an update. Crit Rev Oncol Hematol. 2003;46:187-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Eidt S, Stolte M. Prevalence of intestinal metaplasia in Helicobacter pylori gastritis. Scand J Gastroenterol. 1994;29:607-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Ruol A, Parenti A, Zaninotto G, Merigliano S, Costantini M, Cagol M, Alfieri R, Bonavina L, Peracchia A, Ancona E. Intestinal metaplasia is the probable common precursor of adenocarcinoma in barrett esophagus and adenocarcinoma of the gastric cardia. Cancer. 2000;88:2520-2528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 15. | El-Serag HB, Sonnenberg A, Jamal MM, Kunkel D, Crooks L, Feddersen RM. Characteristics of intestinal metaplasia in the gastric cardia. Am J Gastroenterol. 1999;94:622-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 47] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Morales CP, Spechler SJ. Intestinal metaplasia at the gastroesophageal junction: Barrett's, bacteria, and biomarkers. Am J Gastroenterol. 2003;98:759-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Sharma P, Weston AP, Morales T, Topalovski M, Mayo MS, Sampliner RE. Relative risk of dysplasia for patients with intestinal metaplasia in the distal oesophagus and in the gastric cardia. Gut. 2000;46:9-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 127] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 18. | Canto MI, Setrakian S, Willis JE, Chak A, Petras RE, Sivak MV. Methylene blue staining of dysplastic and nondysplastic Barrett's esophagus: an in vivo and ex vivo study. Endoscopy. 2001;33:391-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 93] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 19. | Olliver JR, Wild CP, Sahay P, Dexter S, Hardie LJ. Chromoendoscopy with methylene blue and associated DNA damage in Barrett's oesophagus. Lancet. 2003;362:373-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 184] [Article Influence: 8.4] [Reference Citation Analysis (0)] |