Published online Aug 7, 2005. doi: 10.3748/wjg.v11.i29.4607
Revised: November 23, 2004
Accepted: December 1, 2004
Published online: August 7, 2005
Symptomatic hepato-diaphragmatic interposition of a bowel loop or Chilaiditi’s syndrome is a peculiar anatomical condition most often found by chance. Its described symptoms range from intermittent, mild abdominal pain and dyspepsia to acute intestinal obstruction. We report a case of hepato-diaphragmatic migration of the hepatic flexure of the colon associated to an unusual, heretofore unreported, angina-like pain exclusively evoked by the left lateral decubitus. To maximize the chance of observing anatomical changes in different postures, computed tomography of the chest and abdomen was performed after air insufflation into the colon. While frank herniation into the chest was excluded, the scan showed that the hepatic flexure-with the interposition of the diaphragm-came in contact with the right side of the heart in the left lateral, but not in the supine, decubitus. This finding was reproduced by echocardiography which also showed virtually unaltered hemodynamics after the change of posture. ECG, left and right ventricular global and regional function as well as cardiac injury markers also remained unchanged during the maneuver, indicating that the pain evoked by the latter was unlikely due to myocardial ischemia. This case suggests that Chilaiditi’s syndrome should be included among the possible, although rare, causes of unexplained angina-like symptoms.
- Citation: Sorrentino D, Bazzocchi M, Badano L, Toso F, Giagu P. Heart-touching Chilaiditi’s syndrome. World J Gastroenterol 2005; 11(29): 4607-4609
- URL: https://www.wjgnet.com/1007-9327/full/v11/i29/4607.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i29.4607
The radiological finding of hepato-diaphragmatic interposition of a bowel segment, also known as Chilaiditi’s sign, defines an uncommon and typically asymptomatic anatomical abnormality. When associated with symptoms, it is termed as Chilaiditi’s syndrome[1]. Although a number of different symptoms have been attributed to this condition they are almost always related to the digestive tract itself such as, most commonly, abdominal pain, dyspepsia and intestinal obstruction due to volvulus.
In the case described in this paper, the hepato-diaphragmatic migration of the hepatic flexure of the colon was associated with an angina-like pain, exclusively evoked by the left lateral decubitus. The investigations conducted in our patient clearly showed that the symptom was associated to the contact between the heart and the intestine. Although the precise mechanism at the basis of this phenomenon remains unknown it is, to our knowledge, the first time that precordial pain has been attributed to such a peculiar anatomical condition.
A 69-year-old white male was admitted to the hospital with a history of retrosternal oppressive pain radiating to the left arm, mild dyspnea, and a state of prostration for the past 2 years.
These symptoms were present with the patient lying on his left side, and subsided in the supine position and in orthostatism.
For this reason, he had been previously referred to a cardiologist. However, an ECG failed to show overt signs of ischemia; a stress test and a Holter monitoring were within limits and a trial with calcium antagonists proved ineffective. At this point, a diagnosis of anxiety/depression syndrome was considered likely but a therapeutic trial with benzodiazepines was without effect.
The only relevant episodes in his past medical history were an apparent pleural effusion at the age of 18 which spontaneously resolved; and an NSAID-related gastric ulcer at the age of 46 which was treated with H2-antagonists with complete healing.
On admittance, the patient was in good general condition. He was overweight (BMI 27.5 kg/m2) but physical examination was otherwise unremarkable. The pulse rate was 72, and the blood pressure was 130/70 mmHg. Laboratory tests showed increased values of ferritin (635 ng/dL), γ-GT (75 U/L) and total cholesterol (295 mg/dL). The ECG tracing at rest was normal. During the hospital stay, the symptoms mentioned above took place on two separate episodes: in each occasion they immediately subsided by changing decubitus. The physical examination during the crisis was unremarkable; the ECG and cardiac injury markers remained unchanged. Cardiac involvement at this point seemed unlikely. Since he reported, during his symptoms, the subjective feeling of a mass moving from the abdomen toward the chest, subsequent studies focused on the gastrointestinal tract.
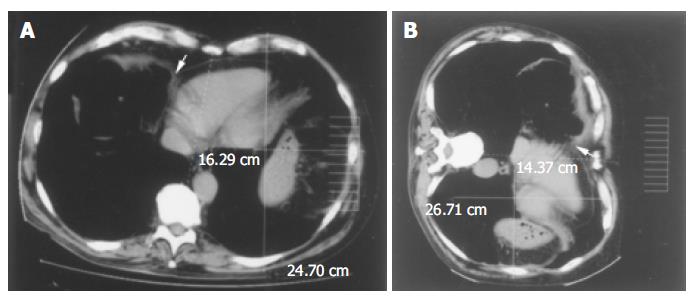
An abdominal ultrasound showed a severe hypotrophism of the liver with marked stretching of the intrahepatic vessels, while the portal hilum and the gallbladder were not identifiable at all. The general picture was not incompatible with chronic liver disease, even in the absence of parenchymal and focal lesions. However, liver disease became unlikely once the diagnosis of Chilaiditi’s sign was established by a double contrast barium enema (not shown) and a CT scan of the abdomen which showed the interposition of the hepatic flexure of the colon between the right liver lobe and the homolateral rib cage (Figure 1) while excluding frank herniation into the chest.
Subsequently, we sought a correlation between this anatomic finding and the patient’s symptoms. To maximize the chances of observing anatomical changes in different postures, a CT scan of the abdomen and chest was performed with a Toshiba Aquilion 16 Multi-Slice CT (Toshiba AMS, Tustin, CA, USA) after air insufflation into the colon. The latter involved an amount of air (approximately 800 cm3) that caused mild discomfort to the patient, roughly equivalent to the sensation provoked by naturally occurring meteorism. The scan demonstrated the close vicinity of the colon to the right side of the heart in the supine position (Figure 2A, arrow). When the same scan was taken with the patient lying on his left side (Figure 2B) it showed that the colon had moved forward and medially, coming into contact with the vena cava and the right side of the heart. In this position, the patient complained of his typical precordial pain. The change of posture also caused migration of the diaphragm and its attached organs (i.e., the heart) toward the left side of the chest (Figures 2A and B). At the same time, the left hemithorax anteroposterior diameter increased, while the transverse diameter decreased (Figures 2A and B).
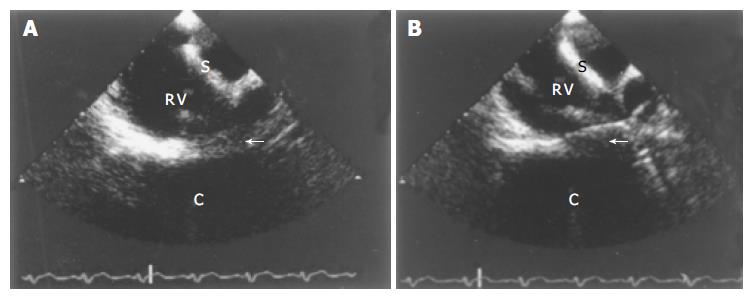
Finally, the patient was subjected to multiplane trans-esophageal echocardiography (SONOS 5500, Philips, Best, Holland) before and after air insufflation into the colon as above. The latter did not produce echos different from the exam conducted under basic conditions. However, the change of posture from the supine (Figure 3A) to the left lateral decubitus (Figure 3B) resulted again in frank contact between the heart and the colon with blurring of each other’s contours. Blood pressure, heart rate, right and left ventricular global and regional function and oxygen saturation remained unchanged indicating no alteration in cardiac hemodynamics.
Thus, the mechanism provoking pain, as well as being reversible, did not appear to involve true ischemia. In addition, the patient refused to take surgery into consideration. Therefore, we opted for careful observation recommending the patient to lose weight. After 8 mo he did lose 8 kg of body weight and his symptoms have now become much less frequent and intense.
Hepato-diaphragmatic interposition of a bowel loop, usually the hepatic flexure of the colon, described by Chilaiditi[2] in 1910, is a peculiar anatomical condition most often found by chance. When associated with symptoms-usually from mild abdominal pain and dyspepsia to acute intestinal obstruction-it is termed Chilaiditi’s syndrome[1].
Congenital anatomical abnormalities such as colonic elongation and laxity of colonic and hepatic suspensory ligaments have been postulated as the principal predisposing factors[3]. Other predisposing situations can be acquired such as an enlarged lower thoracic outlet (e.g., in pregnancy, emphysema, and cirrhosis with ascites), or organ shrinkage (e.g., atrophic cirrhosis of the liver)[4]. Fat deposition between the liver and the colon, in obese individuals, widens the space between the two organs and can also favor the migration of the colon[5].
The case of Chilaiditi’s syndrome reported in this paper is peculiar with regard to its symptoms angina of like pain with left arm irradiation and their likely origin, i.e., the motion of the colon into the chest. Although a case of right rib cage pain has been attributed to Chilaiditi’s syndrome[6] the latter has never been causally associated to precordial pain.
Our patient had a few known predisposing factors for the migration of the hepatic flexure, i.e., he was overweight and, likely, had an abnormally thin and lax diaphragm. In addition, he had a hypotrophic liver even though the latter could have been a consequence rather than the cause of his bowel displacement.
Guided by the absence of cardiologic abnormalities and by the patient’s subjective feeling of a moving abdominal mass, we made an initial diagnosis of Chilaiditi’s sign by barium enema and CT scan. We then elected to perform both CT scan and cardiac ultrasound after air insufflation into the colon to study in detail the expected anatomical changes associated with the patient’s symptom. It should be emphasized that the amount of insufflated air was small and only produced a typical subjective feeling of meteorism. Although the colon (with the interposition of the diaphragm) was very close to the heart in the supine position (Figures 2A and 3A) it was in the left lateral decubitus, that the two organs clearly touched each other and the heart moved to the left of the chest (Figures 2B and 3B). Since the ECG, the cardiac function and the cardiac enzymes remained within limits during the maneuver, it is unlikely that the pain originated from true cardiac ischemia. Blood pressure, heart rate, and oxygen saturation also did not change. Indeed, cardiac hemodynamics were not expected to be affected since the pressure inside the heart chambers far exceeds that inside the colon. Thus, it is possible that the pain felt by the patient, concomitant to the migration of the hepatic flexure, was simply due to the transient stimulation of cardiac nervous fibers or to the internal compression of the chest or to overstretching of the major vessels-including the aorta and vena cava, or to a combination of these last two factors[7]. Indeed, the CT scan showed a movement of the heart with the diaphragm toward the left side of the chest upon changing position (Figures 2A and B). This partial migration might have caused the hypothetical stretching of the vessels as well as (at least in part) the change in the anteroposterior and transverse diameters of the left hemithorax.
Based on patient’s choices and given the apparent absence of a life threatening situation, we did not recommend surgery but only careful observation and weight loss. Indeed, losing weight has gradually decreased the frequency and intensity of the patient’s symptoms.
In conclusion, we have shown a case of Chilaiditi’s syndrome presenting with an unusual symptom-precordial pain-associated to the unusual contact between the colon and the heart and the movement of the heart to the left of the chest. Hence, Chilaiditi’s syndrome should be included among the possible, although rare, causes of unexplained angina-like symptoms.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Lekkas CN, Lentino W. Symptom-producing interposition of the colon. Clinical syndrome in mentally deficient adults. JAMA. 1978;240:747-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 48] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Chilaiditi D. Zur frage der hepatoptose und ptose im allgemeinen im Anschluss an drei Falle von temporarer, partieller Leberverlagerung. Fortcshr Geb Rontgenstr Nuklearmed Erganzongsband. 1910;16:173-208. |
| 3. | Walsh SD, Cruikshank JG. Chilaiditi syndrome. Age Ageing. 1977;6:51-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Pritchard GA, Price-Thomas JM. Internal hernia of the transverse colon. A new syndrome. Dis Colon Rectum. 1986;29:657-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Murphy JM, Maibaum A, Alexander G, Dixon AK. Chilaiditi's syndrome and obesity. Clin Anat. 2000;13:181-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Schubert SR. Chilaiditi's syndrome: an unusual cause of chest or abdominal pain. Geriatrics. 1998;53:85-88. [PubMed] |
| 7. | Braunwald E. The History. ed: Heart Disease, Philadelphia, PA WB Saunders 2000; 1-13. |