Published online May 28, 2005. doi: 10.3748/wjg.v11.i20.3165
Revised: September 22, 2004
Accepted: September 30, 2004
Published online: May 28, 2005
A 42-year-old man presented with a two-year history of progressive dysphagia and hoarseness. Esophagogram and endoscopy revealed submucosal mass effect on the upper esophagus. Computed tomography and magnetic resonance imaging revealed an elongated mass in the retrotracheal region of the lower neck with extension to the posterior mediastinum. Partial tumor resection and histopathological evaluation revealed a WHO type B2 thymoma. Adjuvant radiation and chemotherapy were subsequently administered resulting in complete tumor regression. To our knowledge, this is the first report of ectopic retrotracheal thymoma with clinical and imaging manifestations mimicking those for esophageal submucosal tumor.
- Citation: Ko SF, Tsai YH, Huang HY, Ng SH, Fang FM, Tang Y, Sung MT, Hsieh MJ. Retrotracheal thymoma masquerading as esophageal submucosal tumor. World J Gastroenterol 2005; 11(20): 3165-3166
- URL: https://www.wjgnet.com/1007-9327/full/v11/i20/3165.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i20.3165
Thymoma is an epithelial neoplasm of the thymus, which usually lies in the anterior mediastinum[1-4]. Uncommonly, thymomas can also be found in other locations including the neck, the middle or posterior mediastinum, and the lung[4-9]. These ectopic thymomas are considered to arise from aberrantly distributed thymic tissues due to failure of normal caudal migration into the anterosuperior mediastinum[4-10]. Herein, we described a rare case of retrotracheal thymoma presenting with progressive dysphagia due to compression of the esophagus. To our knowledge, a thymoma developing in such an unusual location and mimicking an esophageal submucosal tumor on endoscopy and imaging studies has not been previously described.
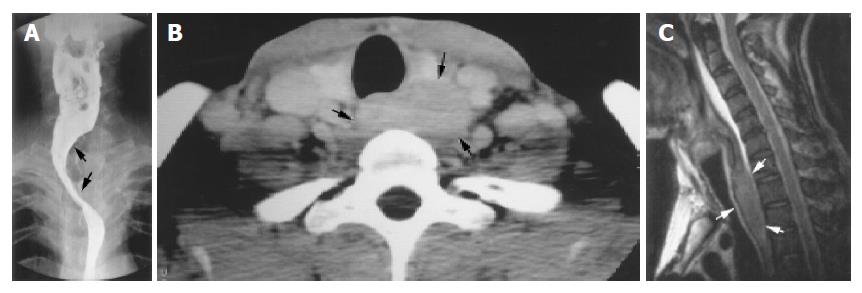
A 42-year-old male presented with a 2-year history of progressive dysphagia and hoarseness. A mass with elastic consistency was palpable in the left lower neck. Otherwise, physical examination was normal. Laboratory work-up was also unremarkable. Endoscopy revealed an intact esophageal mucosa and a submucosal mass compressing the anterior wall of the upper esophagus. Esophagogram confirmed extraluminal compression and right-side deviation of the upper esophagus in the lower neck and upper mediastinum (Figure 1A). Extrinsic compression of the upper posterior tracheal wall was demonstrated from bronchoscopy. Computed tomography (CT) of the neck and thorax demonstrated a well-defined, homogeneously enhanced mass measuring 6 cm×3 cm×2 cm posterior to the trachea in the lower neck and upper posterior mediastinum, while the esophageal lumen was markedly compressed (Figure 1B). Magnetic resonance imaging (MRI) revealed a slightly elongated inhomogeneous mass posterior to the upper tracheal wall, highly suggestive of the presence of an esophageal submucosal mass (Figure 1C). The patient underwent surgical treatment under the initial impression of esophageal submucosal tumor. During the operation, instead of the expected esophageal growth, an elongated mass in the lower neck with extension to the mediastinum lying between the posterior wall of the trachea and anterior wall of the esophagus was found. Only partial resection of the mass via the low-neck approach was possible. Histopathological examination revealed a tumor composed of neoplastic epithelial component cells appearing as scattered plump cells with vesicular nuclei and distinct nucleoli among a heavy population of lymphocytes, compatible with the type B2 WHO classification. The patient refused further thoracotomy for complete tumor resection. Adjuvant chemotherapy and radiotherapy (60 Gy) were performed postoperatively and recovery was unremarkable. Complete resolution of the tumor was noted on 1-year CT follow-up. At the time of writing, there had been no evidence of recurrence in the intervening 5 years.
Embryologically, the thymic epithelium originates bilaterally from the ventral portions of the third pharyngeal pouches and descends caudally with the third parathyroid to a level lower than the thyroid tissue, eventually migrating to the anteriosuperior mediastinum by the fifth or sixth week of gestation[4,10]. Aberrant migration may occur anywhere along this pathway, especially adjacent to the thyroid glands or in the anterior neck[4-10]. Rarely, aberrant thymic tissues identified in the skull base, preaortic and retrocarinal fat during autopsies have also been reported.
Thymoma is the most common anterior mediastinal neoplasm, usually occurring at 30-40 and 60-70 years of age in patients with and without myasthenia gravis, respectively[1-4]. Corresponding to the frequencies for thymus location, 75% of thymomas are in the anterior mediastinum, 15% involve both the anterior and superior mediastinum, and 6% are within the superior mediastinum[4]. The remaining 4% of thymomas occur ectopically, affecting the neck, middle and posterior mediastinum, and the lung[4-9]. To our knowledge, however, isolated ectopic thymoma occurring in the retrotracheal region masquerading as an esophageal submucosal mass has not previously been documented.
Approximately one-third of patients with a thymic tumor are asymptomatic[1,2]. In symptomatic patients, 30% present with myasthenia gravis, and the remainder usually present with chest pain, cough, and dyspnea. Superior vena cava syndrome, weight loss, fever and night sweats can also be found in patients with more aggressive tumors [1,2]. On the other hand, although extremely unusual, our case illustrated that thymoma may be present with progressive dysphagia, which could be related to the unusual anatomic location, leading to initial endoscopic and esophagographic evaluations and a tentative diagnosis of esophageal submucosal tumor.
On CT, thymomas usually appear as homogeneous soft-tissue density oval or lobulated masses, which are usually sharply demarcated and project to one side of the anterior mediastinum[3,6-8]. On MRI, thymomas typically have a low signal intensity on T1-weighted images, which increases with T2-weighted images, and may be homogeneous or inhomogeneous in intensity[3,5]. In retrospect, we found that the tumor morphology on CT and MRI in this particular case was compatible with thymoma. However, owing to the rarity of its location, an accurate preoperative diagnosis was, indeed, difficult and the differential diagnosis included leiomyoma or leimyosarcoma, gastrointestinal stromal tumor, and lymphoma.
Surgical resection is the mainstay of treatment for thymoma[1,2]. Recently, multimodality therapy has been stressed for thymoma, especially for subtotally resected tumors[1,2]. Significant reduction of the rate of thymoma metastasis has also been reported in chemotherapy patients. Adjuvant radiotherapy and chemotherapy were successful in our patient. CT follow-up revealed total tumor regression 1 year after surgery, and the patient remained disease-free 5 years after treatment.
In summary, this report documents a rare occurrence of retrotracheal thymoma presenting with progressive dysphagia. In light of this case, retrotracheal thymoma may be included as one of the unusual differential considerations when submucosal mass effect on the esophagus is encountered.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Detterbeck FC, Parsons AM. Thymic tumors. Ann Thorac Surg. 2004;77:1860-1869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 260] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 2. | Moore KH, McKenzie PR, Kennedy CW, McCaughan BC. Thymoma: trends over time. Ann Thorac Surg. 2001;72:203-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Naidich DP, Webb WR, Muller NL, Krinsky GA, Zerhouni EA, Siegelman SS. Computed tomography and magnetic resonance of the thorax. 3rd ed. Philadelphia: Lippincott Raven 1999; 58-76. |
| 4. | Rosai J, Levine GD. Tumors of the thymus. Atlas of tumor pathology. Fascicle 13, 2nd series. Washington: Armed Forces Institute Pathol 1976; 34-161. |
| 5. | Nagasawa K, Takahashi K, Hayashi T, Aburano T. Ectopic cervical thymoma: MRI findings. AJR Am J Roentgenol. 2004;182:262-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Kanzaki M, Oyama K, Ikeda T, Yoshida T, Murasugi M, Onuki T. Noninvasive thymoma in the middle mediastinum. Ann Thorac Surg. 2004;77:2209-2210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Kojima K, Yokoi K, Matsuguma H, Kondo T, Kamiyama Y, Mori K, Igarashi S. Middle mediastinal thymoma. J Thorac Cardiovasc Surg. 2002;124:639-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Tan A, Holdener GP, Hecht A, Gelfand C, Baker B. Malignant thymoma in an ectopic thymus: CT appearance. J Comput Assist Tomogr. 1991;15:842-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Moran CA, Suster S, Fishback NF, Koss MN. Primary intrapulmonary thymoma. A clinicopathologic and immunohistochemical study of eight cases. Am J Surg Pathol. 1995;19:304-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 56] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Richardson MA, Sie KYC. The neck: embryology and anatomy. Pediatric Otolaryngology. 3rd ed. Philadelphia: WB Saunders Company 1996; 1464-1479. |