INTRODUCTION
Gastric emphysema or pneumatosis is a rare finding. It was first described by Brouardel in 1895 and only 42 cases have been described in the literature[1]. Although uncommon, the radiologic[2], endoscopic[3], histologic[3], and percutaneous ultrasound[4,5] findings of this condition are well described. Since its development in the 1980s, endoscopic ultrasound[6-8] has been used for evaluating various esophageal, gastric and pancreatic-biliary diseases[9]. Here, we present the first description of the endoscopic ultrasonographic appearance of gastric emphysema.
CASE REPORT
An 87-year-old man presented to our gastroenterology ward with jaundice, fever, and abdominal pain in January 2002. He had been diagnosed with periampullary adenocarcinoma in June 2001. The tumor was not resected due to his advanced age and comorbid conditions; obstructive jaundice was treated with repeated sessions of palliative endoscopic biliary stenting. On admission, the patient appeared cachectic and complained of some abdominal pain. Physical examination was remarkable for scleral icterus, abdominal distension and epigastric tenderness. His hemogram showed mild anemia with a mildly elevated white cell count of 11300/mm3 (84% neutrophils). Total serum bilirubin level was 1.54 mg/dL.
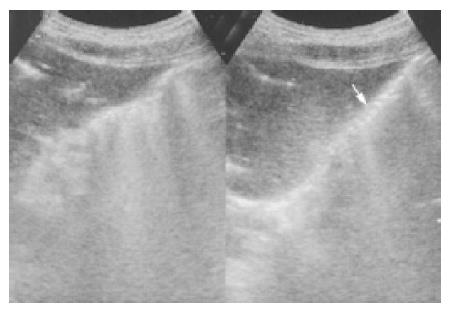
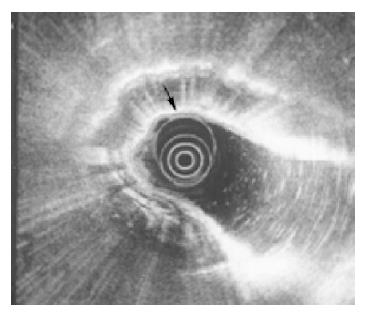
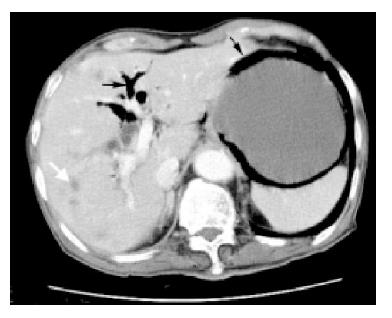
Abdominal ultrasonography revealed multiple- liver metastases, pneumobilia and persistent air in the gastric wall despite changing the patient’s position (Figure 1). Gastric emphysema was suspected. Because of this, endoscopic ultrasonography was performed using an Olympus GFUM200 echoendoscope with Olympus EU-M20 system (Olympus America Inc., Melville, NY). This showed a band of bright echogenicity arising from the submucosa layer, representing a large amount of gas in the gastric wall (Figure 2). Abdominal computerized tomography confirmed the presence of air in the gastric wall, pneumobilia and multiple- liver metastases (Figure 3). The mesenteric artery and vein were both patent.
Figure 1 Abdominal sonography showing air in the gastric wall (arrow).
Figure 2 Endoscopic ultrasonography showing a band of bright echogenicity arising from the submucosal layer with shadowing (arrow), representing air in the gastric wall.
Figure 3 Abdominal computerized tomography revealing multiple liver metastases (white arrow), pneumobilia (thin arrow) and persistent air in the gastric wall (thick arrow).
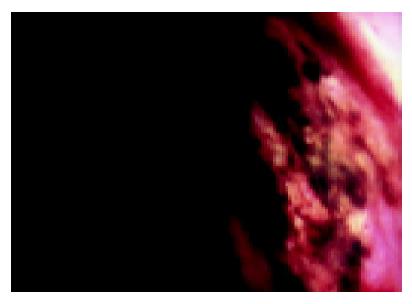
Nasogastric aspirate yielded coffee-ground material on the third hospital day and prompting upper endoscopy revealed diffuse erythema, edema, erosions and sloughing of the mucosa throughout the stomach, without active bleeding (Figure 4). There was also partial duodenal obstruction by the periampullary cancer.
Figure 4 Upper endoscopy showing diffuse erythema, edema, erosions and sloughing of the gastric mucosa.
The patient was treated with acid suppression therapy using intravenous omeprazole and the bleeding resolved. The patient died 1 mo later from an episode of nosocomial pneumonia and progressive liver failure. Gastric emphysema was persistently detected throughout this period by serial abdominal ultrasonography.
DISCUSSION
The presence of air in the gastric wall is a very rare condition. Emphysematous gastritis (or phlegmonous gastritis) and gastric emphysema (or gastric pneumatosis) are variations of conditions associated with the presence of intramural air in the stomach[1,10]. In children, this is associated with pyloric stenosis, gastric malrotation, annular pancreas, cardiac surgery and incorrect positioning of feeding catheters[11-15]. In adults, instrumentation-related injury[16], gastric outlet obstruction by gastric, duodenal or pancreatic malignancies, and bowel ischemia or infarction account for the majority of cases[1].
Four theories have been proposed to explain the development of gas within the gastric wall[17]. In the bacterial theory, Clostridium welchii and other gas-forming aerobic colonic bacilli, including Escherichia coli, Streptococcus, Bacillus subtili and Bacillus proteus generate the intramucosal gas seen in emphysematous gastritis[10]. The outcome in these situations is almost always fatal despite surgical intervention and broad spectrum antibiotic therapy. In the mechanical theory, air is thought to enter the gastric wall due to increased mural pressure[17], possibly caused by air insufflation during endoscopy[18] or intestinal obstruction[19,20]. In the mucosal damage theory, air enters the gastric wall through disrupted mucosa. This may account for gastric wall air associated with a penetrating gastric ulcer[5]. In the pulmonary disease theory, alveolar air dissecting down the mediastinum into the gastric wall in patients with severe asthma or emphysema results in the presence of gastric wall air. In our present case, we believe that repeated biliary stenting led to dissection of air into the gastric wall. In addition, increased intragastric air pressure due to partial duodenal obstruction may have contributed to the development of gastric emphysema as well.
The diagnosis of gastric wall air is usually made radiographically. Two radiological patterns of gastric intramural air have been described. The linear lucency pattern is usually associated with gastric emphysema and the cystic, mottled pattern is usually associated with emphysematous gastritis, a much more serious condition[1]. However, these patterns are not specific enough to distinguish between these two clinical entities[1,2]. Gastric emphysema can also mimic pneumoperitoneum[16]. Therefore, computerized tomography is the test of choice because it evaluates the entire abdominal cavity[2,21,22].
Endoscopic findings in patients with gastric emphysema or emphysematous gastritis have been described. These include submucosal gas bubbles, necroinflammatory changes, and erosions; in some cases, the mucosa appears normal[3]. Endoscopic biopsy may reveal numerous empty spaces in the lamina propria[3]. In our patient, endoscopy revealed only non-specific inflammatory changes and did not help in the diagnosis or management of gastric emphysema.
Unlike the nonspecific endoscopic findings, endoscopic ultrasonography clearly demonstrates the presence of a linear band of air in the submucosal layer. To our knowledge, this is the first report of endoscopic ultrasonographic findings in gastric emphysema or emphysematous gastritis. Although the presence of air in the gastric wall can be easily diagnosed by non-invasive tests such as abdominal ultrasonography or computerized tomography, endoscopic ultrasonography allows better visualization of the gastric wall and be useful in differentiating between gastric emphysema and emphysematous gastritis. More data from additional patients are needed to establish the role of endoscopic ultrasonography in this rare condition.