Copyright
©The Author(s) 2025.
World J Gastroenterol. Aug 14, 2025; 31(30): 108680
Published online Aug 14, 2025. doi: 10.3748/wjg.v31.i30.108680
Published online Aug 14, 2025. doi: 10.3748/wjg.v31.i30.108680
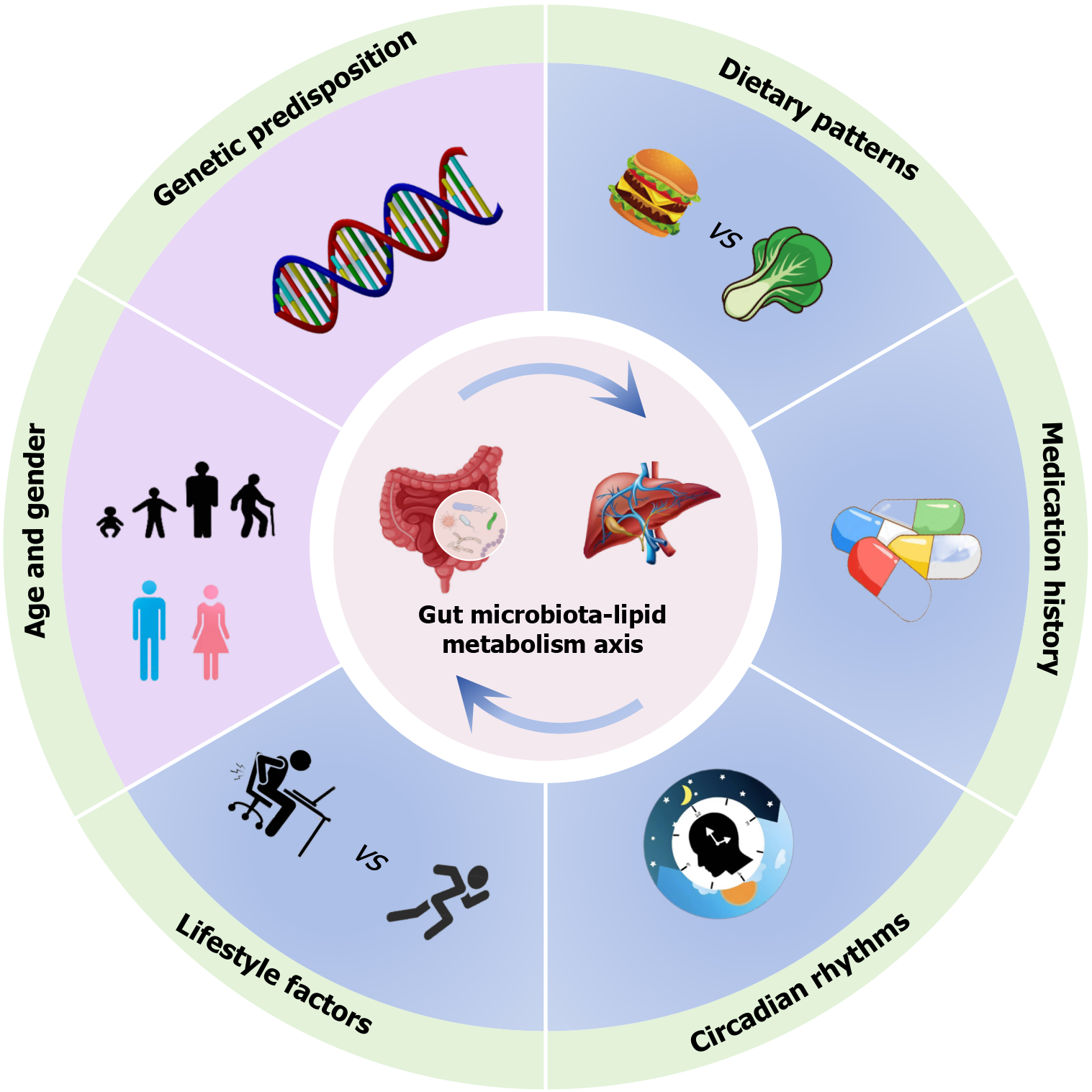
Figure 1 Host-environment co-dependencies shaping the gut microbiota-lipid metabolism axis.
The gut microbiota function as a dynamic meta-organism whose composition and metabolic activity are differentially regulated by host genetic factors and environmental modulators, including lifestyle factors, dietary patterns, pharmacological exposures, and circadian rhythms, which are also potent regulators of lipid metabolism.
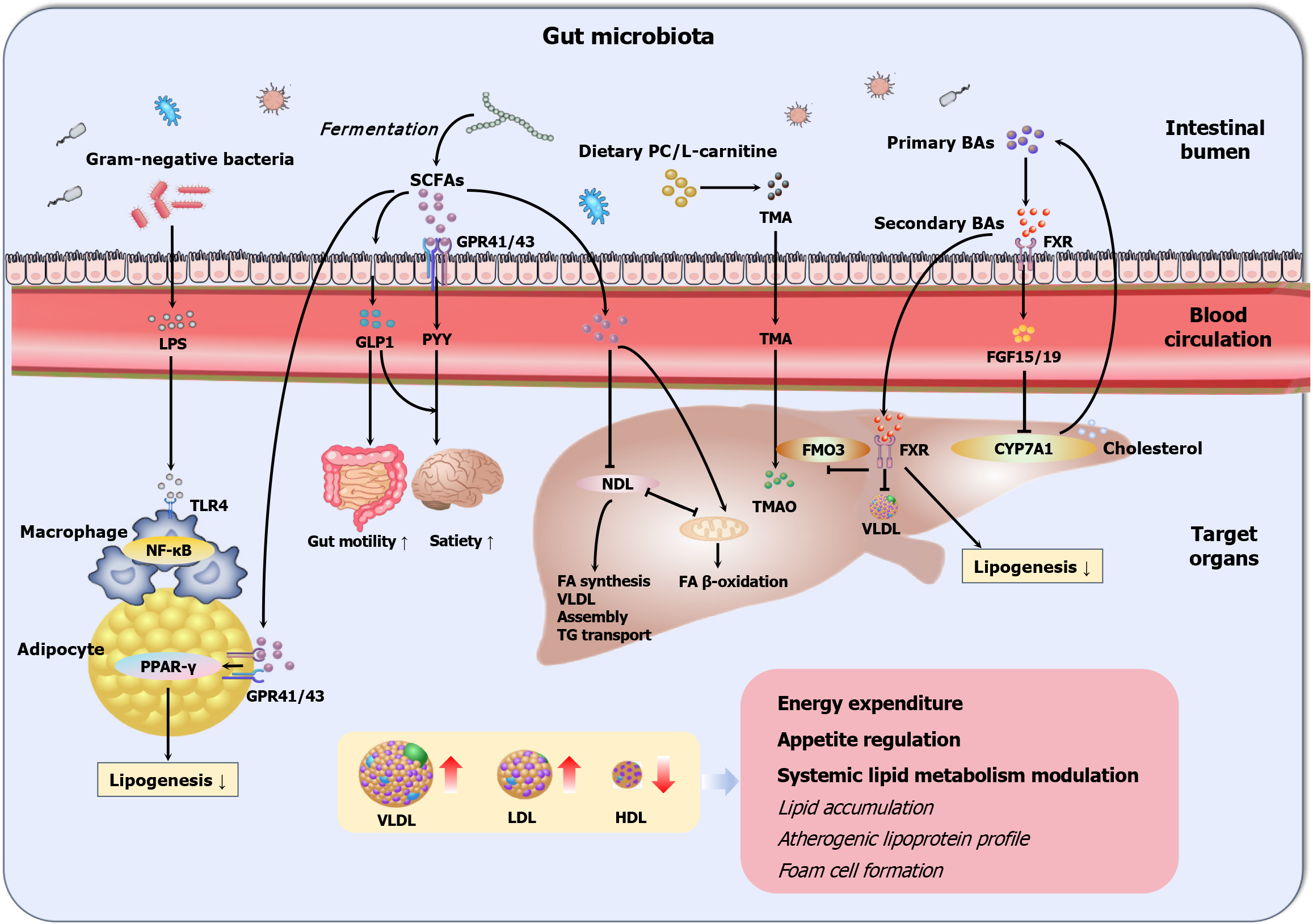
Figure 2 Schematic illustration of gut microbiota and lipid metabolism interactions.
Different pathways have been proposed for the influences of gut microbiota (GM) on systemic lipid metabolism. The liver operates as the metabolic command center governing systemic lipid homeostasis through an intricate balance of de novo lipogenesis converting excess carbohydrates to fatty acids, very low-density lipoprotein assembly, triglyceride transport, and mitochondrial β-oxidation regulating fatty acid catabolism. Parallel to hepatic regulation, GM engages in systemic lipid modulation through bidirectional molecular dialogues. Microbial structural components such as lipopolysaccharide translocate across the intestinal barrier, activating host pattern recognition receptors including toll-like receptors. These interactions trigger pro-inflammatory or immunomodulatory cascades. Concurrently, GM-derived metabolites such as short-chain fatty acids and bile acids exert multifaceted regulatory effects, and molecular mechanisms of short-chain fatty acids center on G protein-coupled receptor networks, with interactions stimulating anorexigenic hormone secretion, while trimethylamine N-oxide exacerbates atherosclerosis through foam cell formation. SCFAs: Short-chain fatty acids; PC: Phosphatidylcholine; BAs: Bile acids; GPR: G protein-coupled receptor; TMA: Trimethylamine; FXR: Farnesoid X receptor; LPS: Lipopolysaccharide; GLP-1: Glucagon-like peptide-1; PYY: Peptide YY; FGF: Fibroblast growth factor; TLR: Toll-like receptor; NF-κB: Nuclear factor-kappa B; PPAR: Peroxisome proliferator-activated receptor; NDL: De novo lipogenesis; TMAO: Trimethylamine N-oxide; FMO3: Flavin monooxygenase 3; CYP7A1: Cholesterol 7α-hydroxylase; FAs: Fatty acids; VLDL: Very low-density lipoprotein; TG: Triglyceride; LDL: Low-density lipoprotein; HDL: High-density lipoprotein.
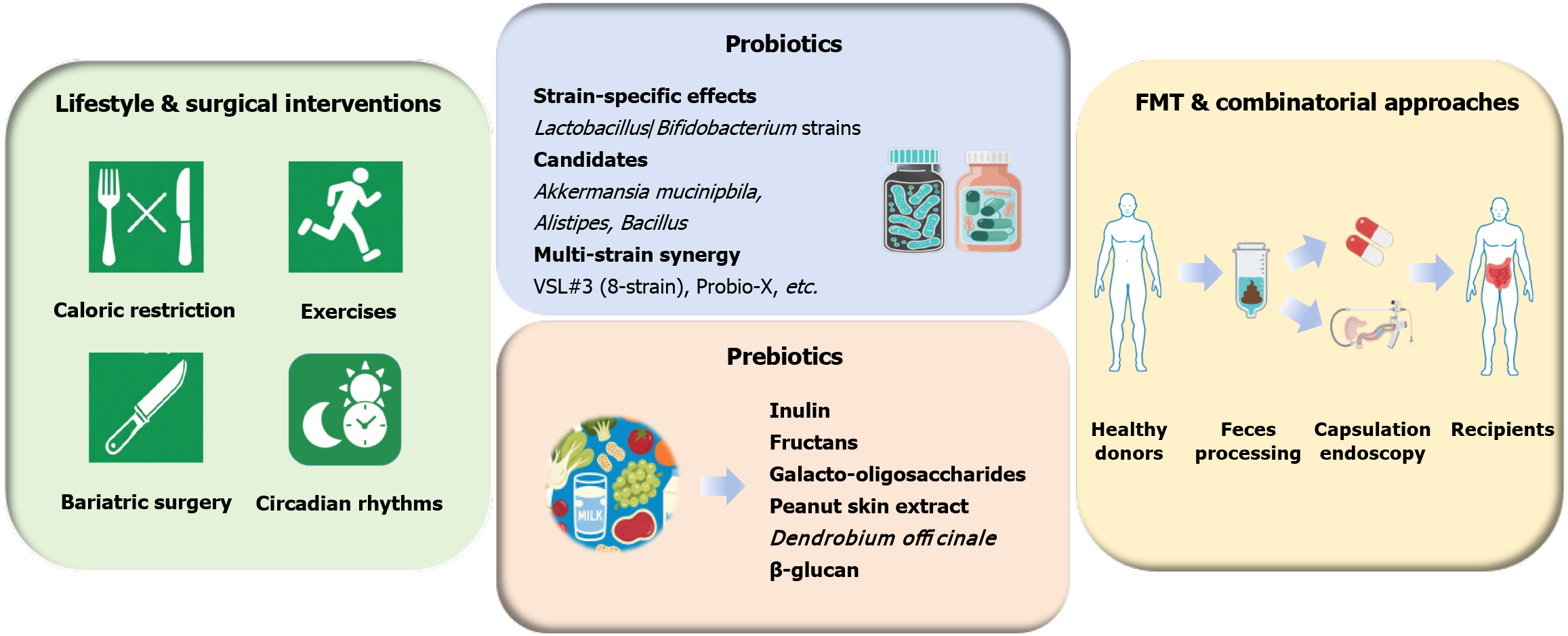
Figure 3 Therapeutic strategies targeting gut microbiota for dyslipidemia.
The gut microbiota (GM) has emerged as a therapeutic target in dyslipidemia management. Lifestyle modifications, including caloric restriction and aerobic exercise, induce beneficial GM shifts, which are strongly correlated with restored microbial gene richness and improved lipid profiles. Current GM-targeting strategies employ probiotics (e.g., Lactobacillus and Bifidobacterium strains), prebiotics (e.g., inulin and resistant starches), and fecal microbiota transplantation. While, future synergistic design integrating probiotics, prebiotics or fecal microbiota transplantation with lifestyle intervention and pharmacotherapies may amplify strain-specific effects. FMT: Fecal microbiota transplantation.
- Citation: Lv J, Zhao HP, Yu Y, Wang JH, Zhang XJ, Guo ZQ, Jiang WY, Wang K, Guo L. From gut microbial ecology to lipid homeostasis: Decoding the role of gut microbiota in dyslipidemia pathogenesis and intervention. World J Gastroenterol 2025; 31(30): 108680
- URL: https://www.wjgnet.com/1007-9327/full/v31/i30/108680.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i30.108680