Copyright
©The Author(s) 2023.
World J Gastroenterol. Jul 21, 2023; 29(27): 4222-4235
Published online Jul 21, 2023. doi: 10.3748/wjg.v29.i27.4222
Published online Jul 21, 2023. doi: 10.3748/wjg.v29.i27.4222
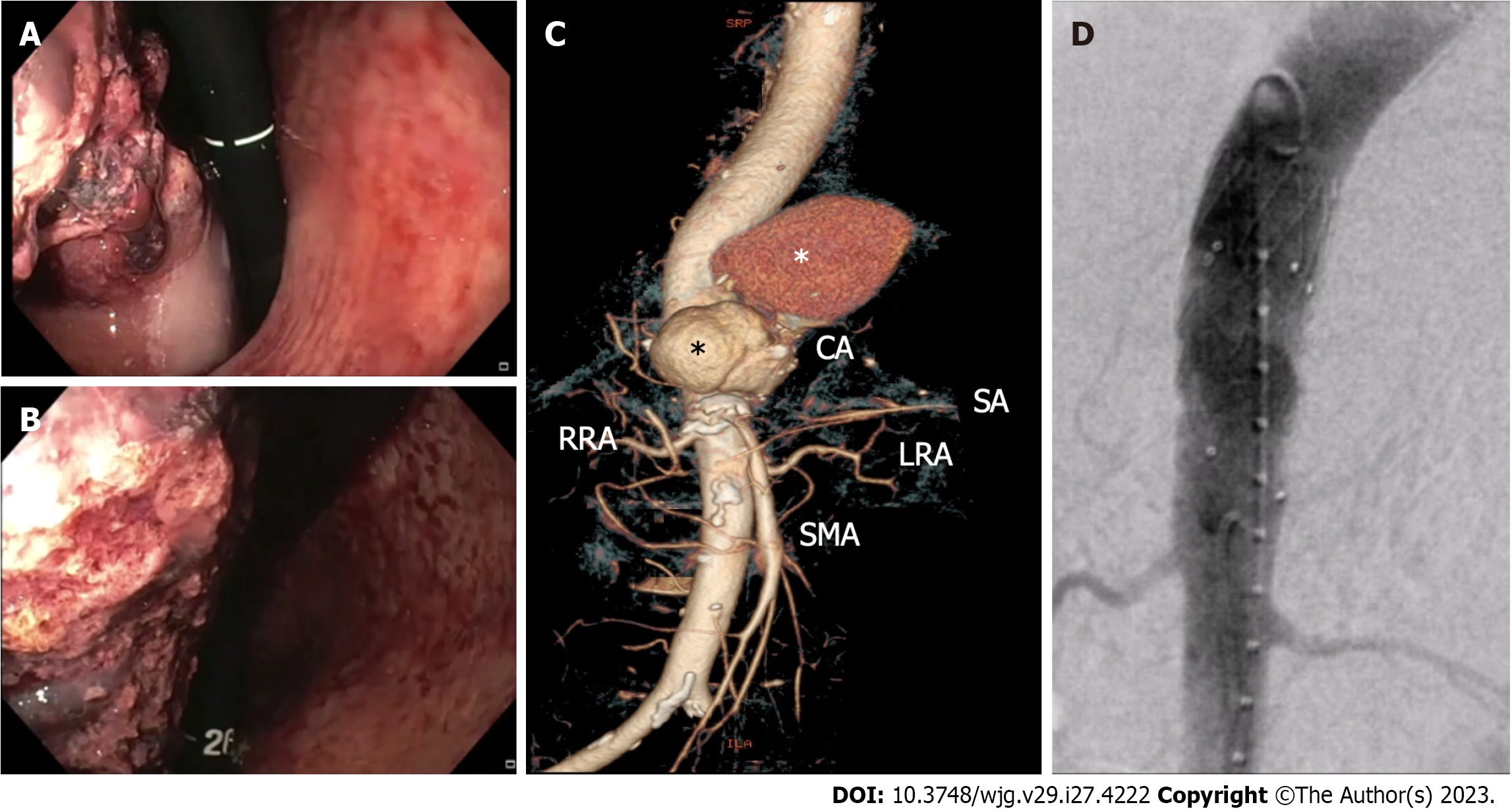
Figure 1 Non-variceal upper gastrointestinal bleeding due to primary aorto-gastric fistula.
A and B: Retroflexed endoscopic view showing gastric bulging mass partially covered by blood clots, originating from the fundus and extending to the posterior wall of the proximal body; C: Three-dimensional computed tomography angiography showing ruptured thoracoabdominal aortic aneurysm (black asterisk), retained by a periaortic hematoma (white asterisk); D: Endovascular stent graft aortic repair. CA: Celiac artery; RRA: Right renal artery; SA: Splenic artery; LRA: Left renal artery; SMA: Superior mesenteric artery.
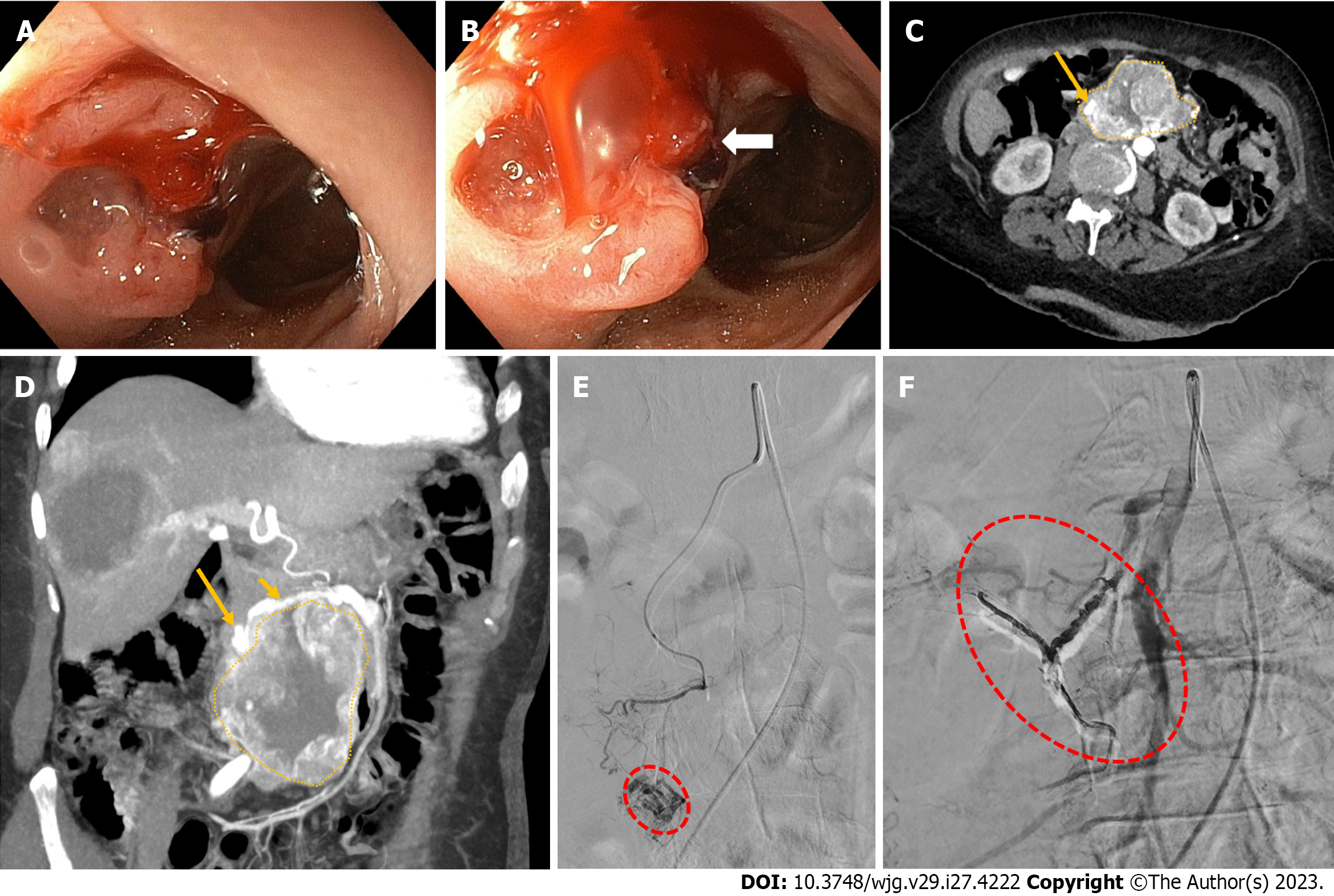
Figure 2 Non-variceal upper gastrointestinal bleeding due rupture of a superior mesenteric artery pseudoaneurysm into the duodenum.
A and B: Upper endoscopy showing a bulging, focally ulcerated, lesion in the second-third part of the duodenum, with a suspected small fistulous orifice on its surface (arrow); C and D: Contrast-enhanced computed tomography axial scan in the arterial phase (C) and its maximum intensity projection oblique-coronal reconstruction (D) showing a large lesion (dotted area, C and D) arising from the second-third part of the duodenum, with peripheral vascularity and a pseudoaneurysm (long arrow, C and D) arising from branches of the superior mesenteric artery (short arrow, B); E: Superselective superior mesenteric artery angiography showing a pseudoaneurysm (red dotted circle) fed by the inferior pancreaticoduodenal artery; F: Successful endovascular embolization by the use of cohesive glue (Onyx-18®, Medtronic, Dublin, Ireland) with disappearance of the pseudoaneurysm and visibility of the Onyx-18® cast (red dotted circle).
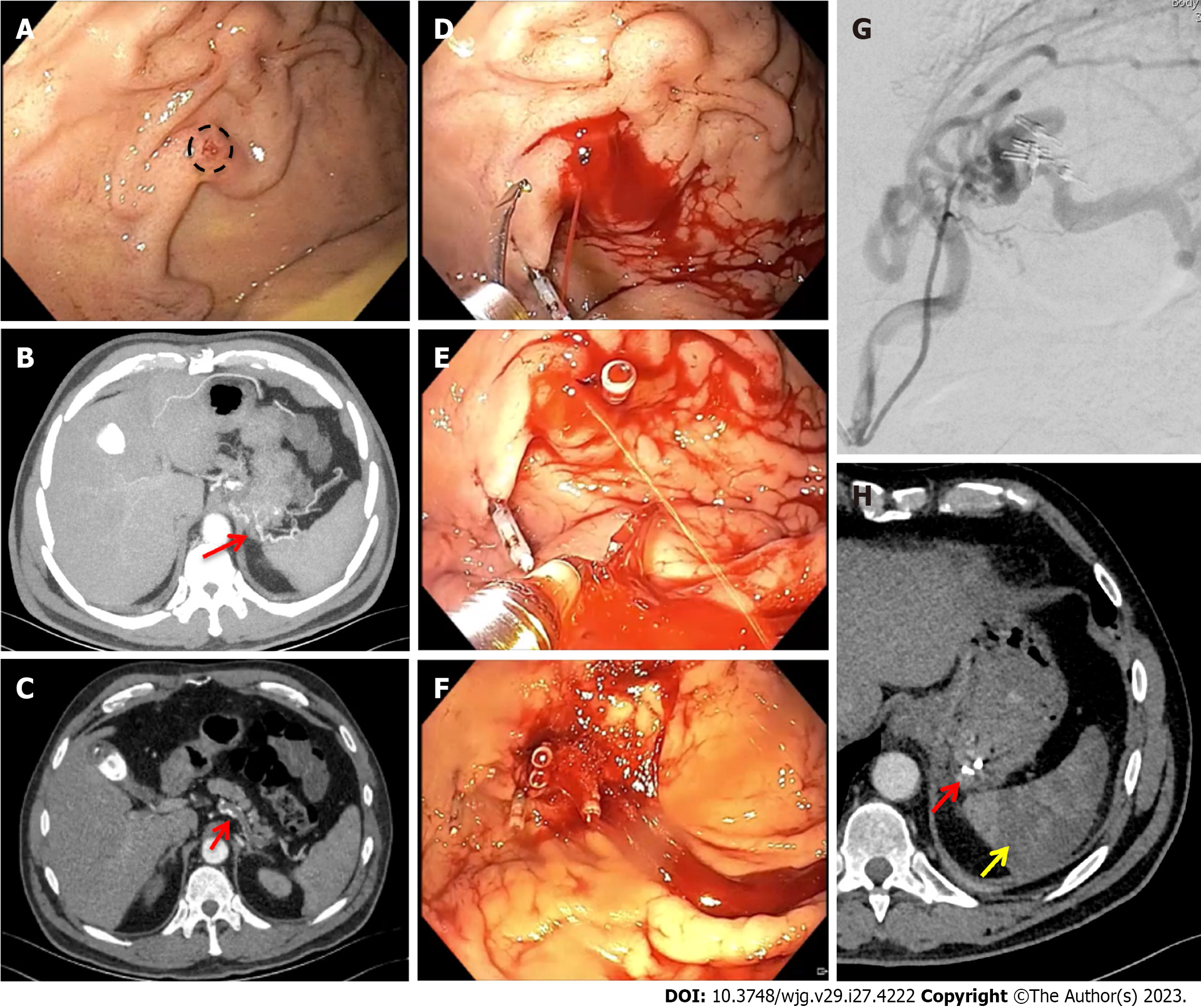
Figure 3 Non-variceal upper gastrointestinal bleeding due to gastric submucosal arterial collaterals secondary to splenic artery thrombosis.
A: Retroflexed endoscopic view of the gastric fundus showing varicose-shaped submucosal vessels with a small erosion (circle), in the absence of active bleeding; B and C: Pre-operative axial computed tomography arterial phase showing an arterial cluster at the gastric fundus (B: arrow) arising from splenic artery collateral vessels due to splenic artery complete thrombosis (C: arrow); D-F: Successful endoscopic mechanical hemostasis attempt, with intraprocedural spurting active bleeding following first endoclip application (D and E); G: Operative angiography with selective arterial embolization using microspheres; H: Post-operative axial computed tomography arterial phase showing gastric vascular lesion exclusion (red arrow) and splenic infarction (yellow arrow).
Figure 4 Non-variceal upper gastrointestinal bleeding due to Dieulafoy’s lesion.
A: Retroflexed endoscopic view of the gastric fundus showing a minute mucosal defect, surrounded by normal-appearing mucosa, without active bleeding; B: Active bleeding following provocative water-jet endoscopic irrigation; C: Successful endoscopic mechanical hemostasis.
Figure 5 Non-variceal upper gastrointestinal bleeding due to Cameron lesion.
Retroflexed endoscopic view of the gastric fundus showing a fibrin covered linear erosion (arrow) at the end of a large hiatal ernia.
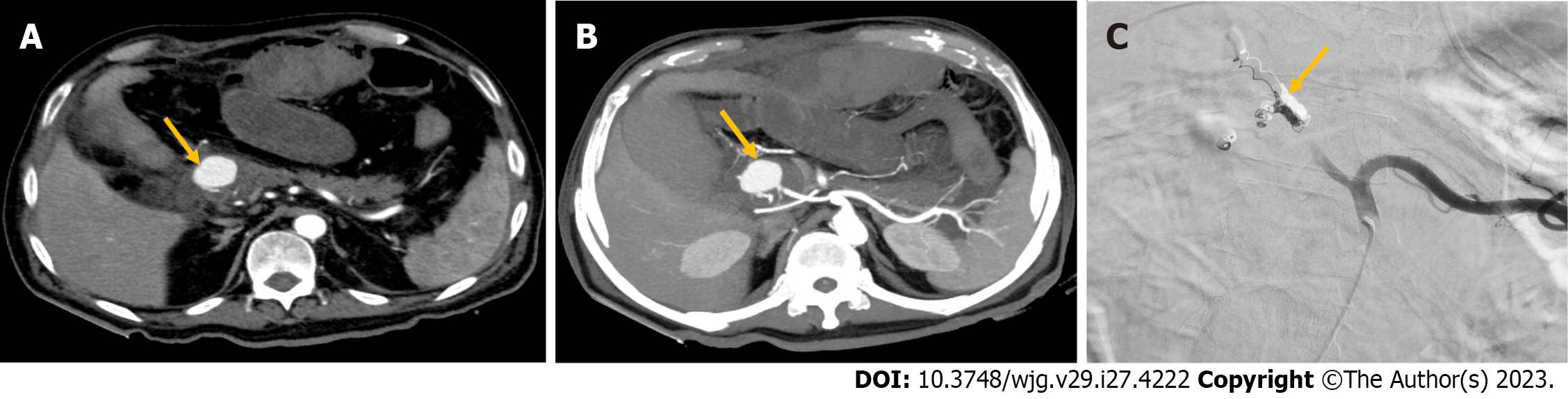
Figure 6 Non-variceal upper gastrointestinal bleeding due to hemosuccus pancreaticus.
A and B: Contrast-enhanced computed tomography axial scan in the arterial phase (A) and its maximum intensity projection axial reconstruction (B) showing a large pancreaticoduodenal artery pseudoaneurysm (arrow, A and B); C: Successful endovascular coil embolization (arrow).
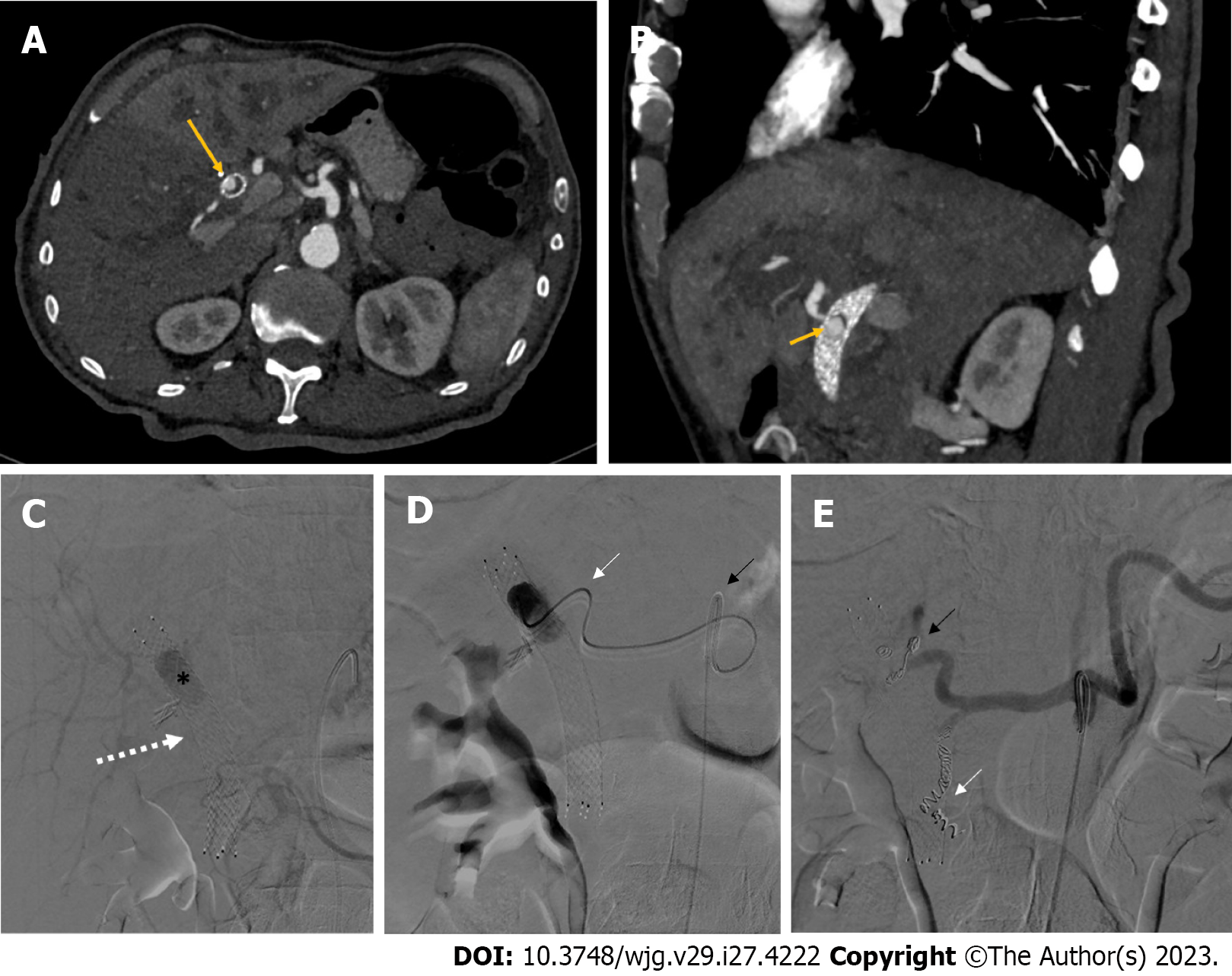
Figure 7 Non-variceal upper gastrointestinal bleeding due to hemobilia.
A and B: Contrast-enhanced computed tomography axial scan in the arterial phase (A) and its maximum intensity projection oblique-sagittal reconstruction (B) showing a pseudoaneurysm in the lumen of the metallic biliary stent (long arrow, A), arising from the hepatic artery (short arrow, B); C: Delayed phase celiac angiography showing a pseudoaneurysm (black asterisk) into the lumen of a metallic biliary stent (white arrow); D: The pseudoaneurysm of the proper hepatic artery was reached with a 2.7 Fr microcatheter (white arrow) coaxially through a 5 Fr catheter (black arrow) positioned into the celiac trunk; E: Successful coil embolization of both the proper hepatic artery (black arrow) and the gastroduodenal artery (white arrow), in order to avoid recanalization.
- Citation: Martino A, Di Serafino M, Orsini L, Giurazza F, Fiorentino R, Crolla E, Campione S, Molino C, Romano L, Lombardi G. Rare causes of acute non-variceal upper gastrointestinal bleeding: A comprehensive review. World J Gastroenterol 2023; 29(27): 4222-4235
- URL: https://www.wjgnet.com/1007-9327/full/v29/i27/4222.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i27.4222