Copyright
©The Author(s) 2021.
World J Gastroenterol. Jul 28, 2021; 27(28): 4504-4535
Published online Jul 28, 2021. doi: 10.3748/wjg.v27.i28.4504
Published online Jul 28, 2021. doi: 10.3748/wjg.v27.i28.4504
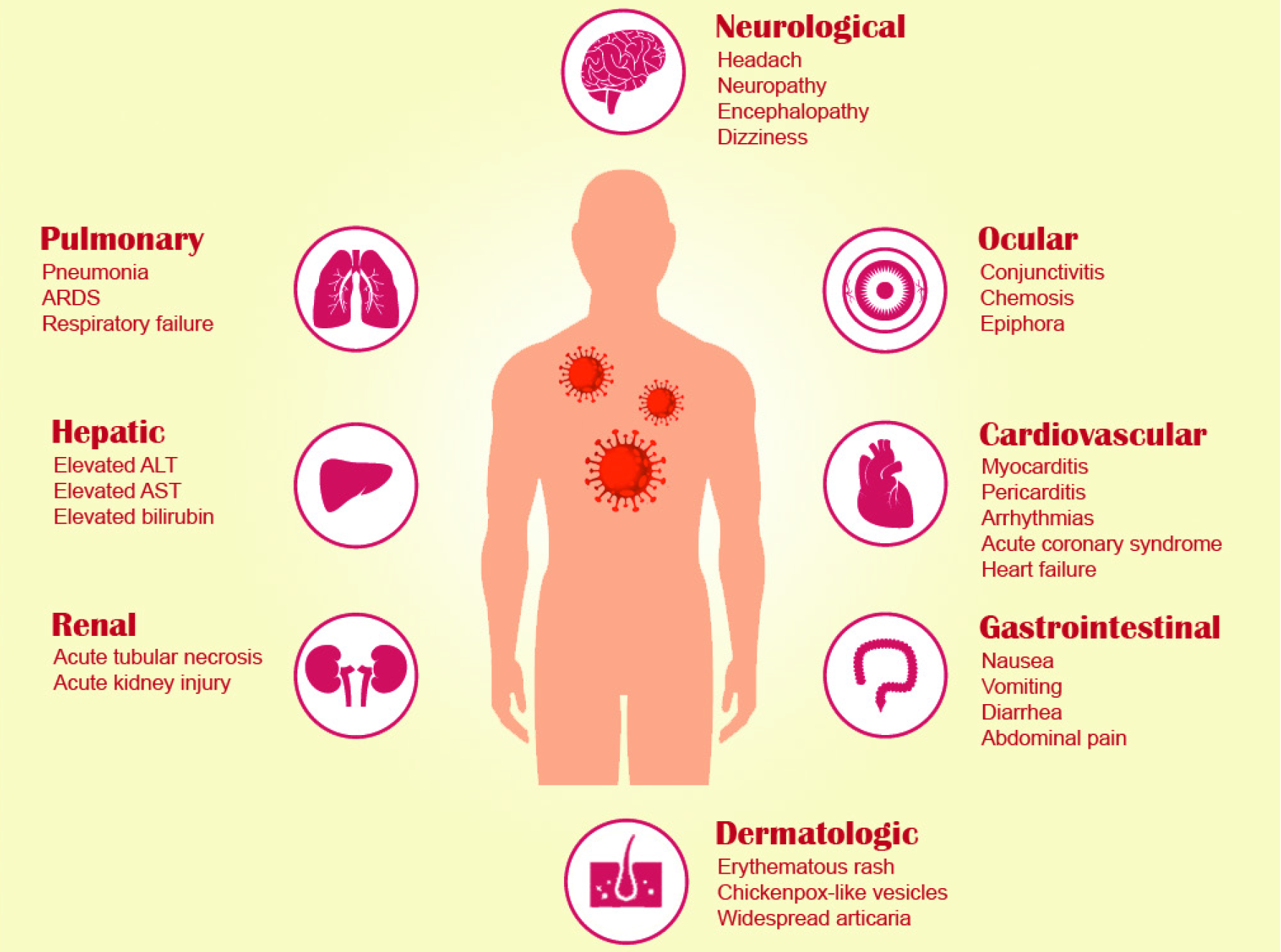
Figure 1 Pulmonary and extrapulmonary manifestations of coronavirus disease 2019.
ARDS: Acute respiratory distress syndrome; ALT: Alanine aminotransferase; AST: Aspartate aminotransferase. Headache and urticaria spelled wrongly.
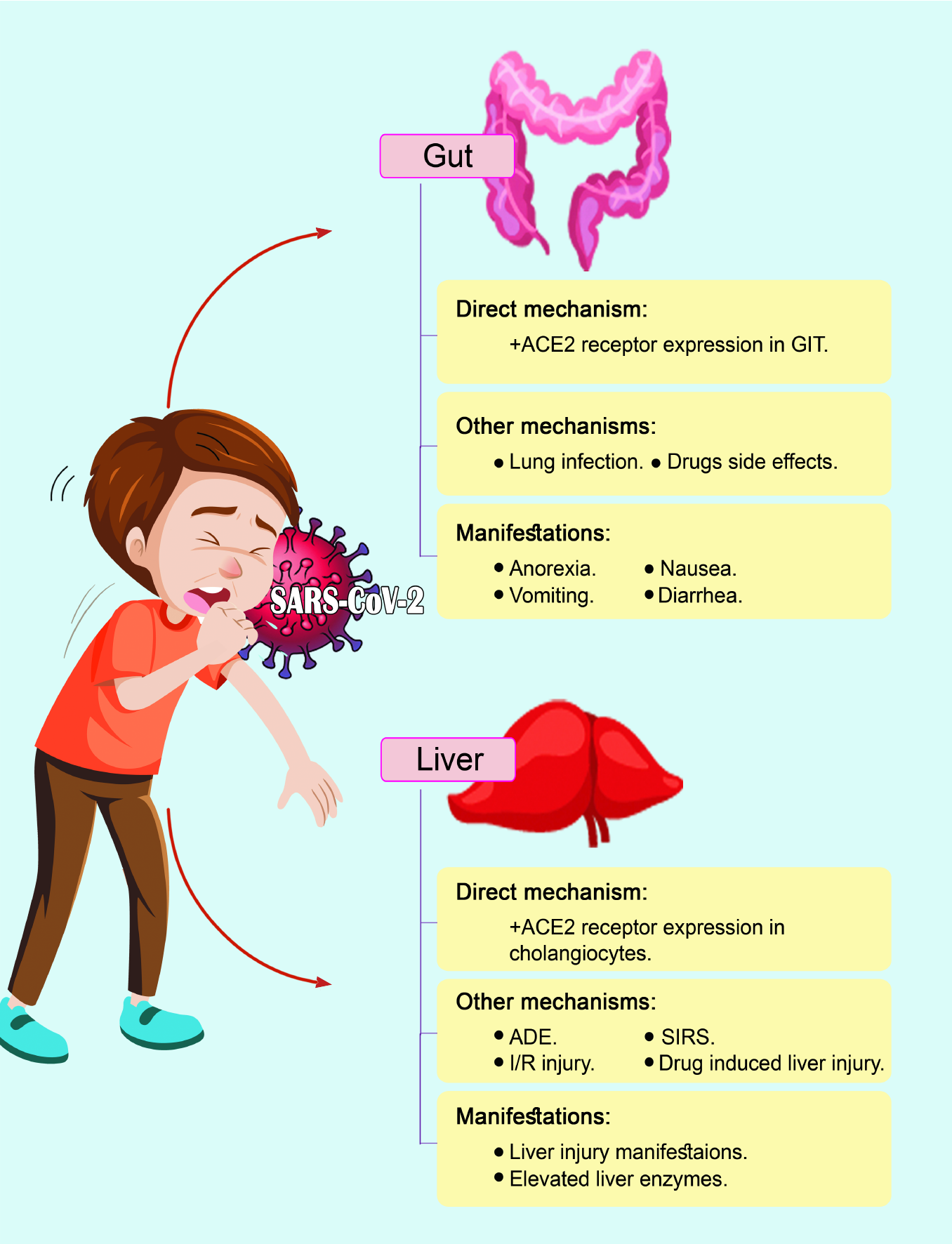
Figure 2 Mechanisms and manifestations of coronavirus disease 2019 in the gut and liver.
SARS-CoV-2: Severe acute respiratory syndrome coro
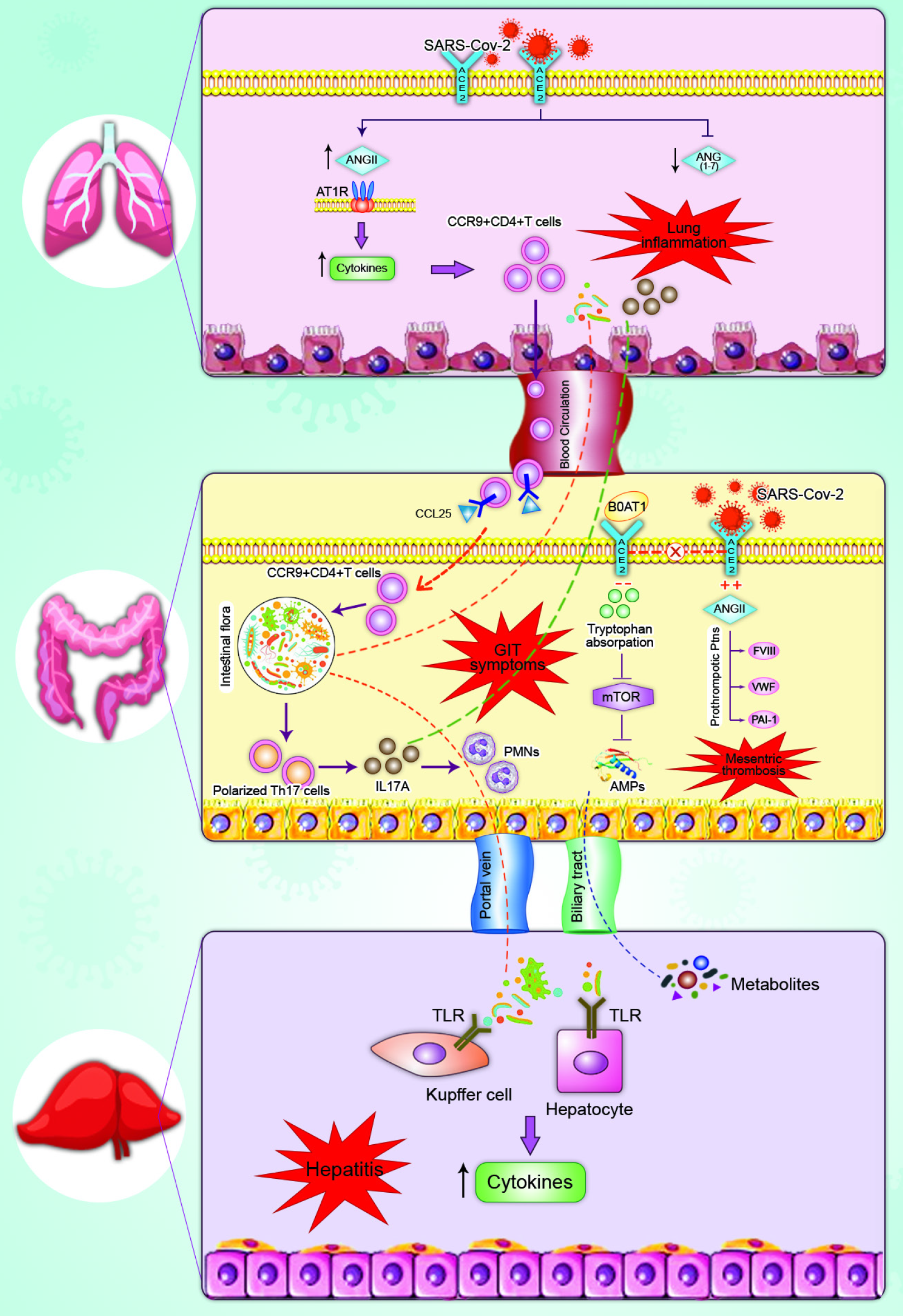
Figure 3 Mechanism of gastrointestinal symptoms in patients with coronavirus disease 2019.
(1) Gut-lung axis: Severe acute respiratory syndro
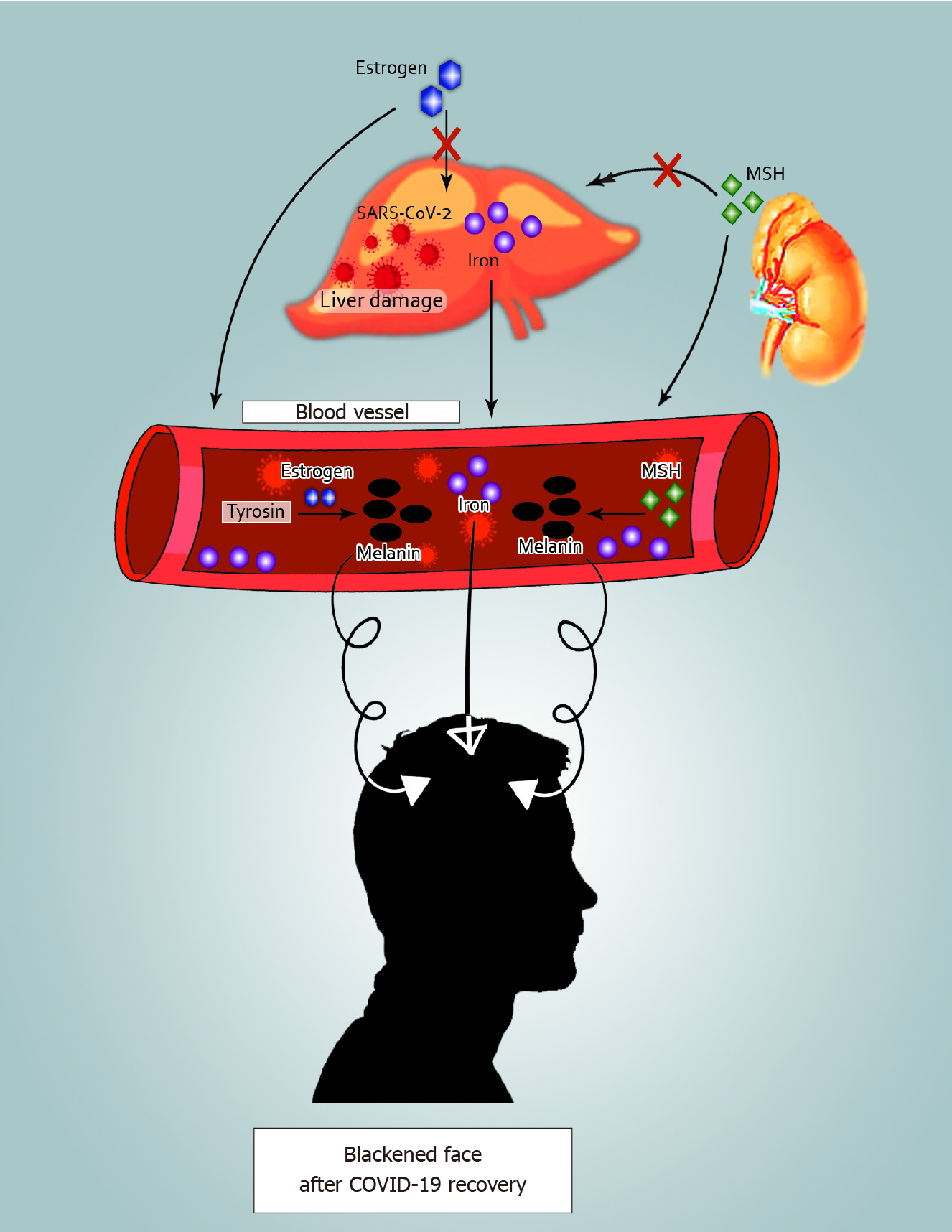
Figure 4 Facial blackness and dull skin after coronavirus disease 2019 recovery.
Three possible mechanisms are shown: (1) Iron in the damaged liver drains into blood vessels. Blood with high iron levels can lead to blackening of the face when it supplies the facial skin; (2) Estrogen cannot be metabolized in the damaged liver. Thus, elevated estrogen in the blood enhances the conversion of tyrosine to melanin; and (3) When liver function is impaired, adrenocortical function is hypoactive, and melanocyte-stimulating hormone increases resulting in an elevation in the secretion of melanin. SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2; MSH: Melanocyte-stimulating hormone; COVID-19: Coronavirus disease 2019.
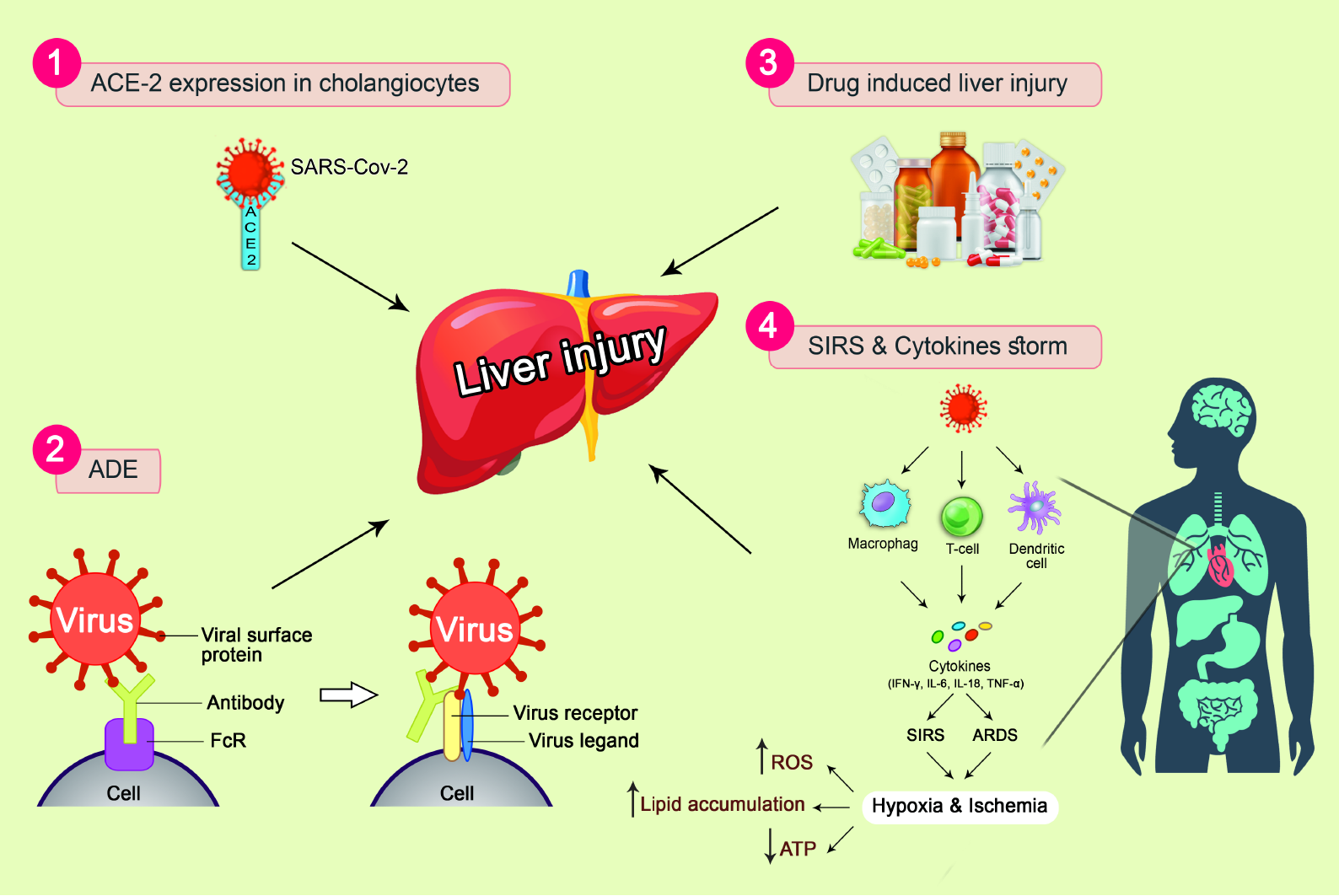
Figure 5 Mechanisms of liver injury in patients with coronavirus disease 2019.
(1) Angiotensin-converting enzyme 2-mediated targeting of cholan
- Citation: Mohamed DZ, Ghoneim MES, Abu-Risha SES, Abdelsalam RA, Farag MA. Gastrointestinal and hepatic diseases during the COVID-19 pandemic: Manifestations, mechanism and management. World J Gastroenterol 2021; 27(28): 4504-4535
- URL: https://www.wjgnet.com/1007-9327/full/v27/i28/4504.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i28.4504