Copyright
©The Author(s) 2020.
World J Gastroenterol. Aug 14, 2020; 26(30): 4557-4563
Published online Aug 14, 2020. doi: 10.3748/wjg.v26.i30.4557
Published online Aug 14, 2020. doi: 10.3748/wjg.v26.i30.4557
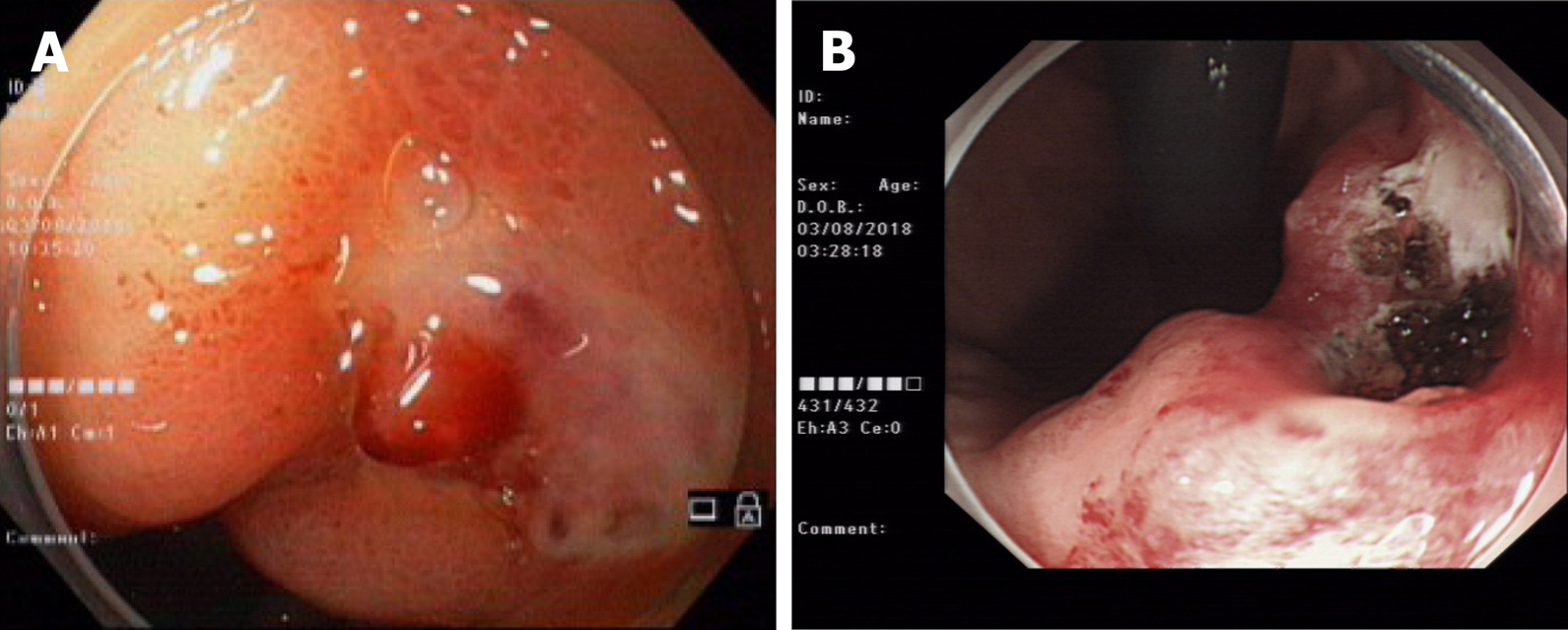
Figure 1 One year ago, bleeding in the small curvature of the stomach suggested Dieulafoy’s disease (A), and high-frequency electrocoagulation was applied for hemostasis (B).
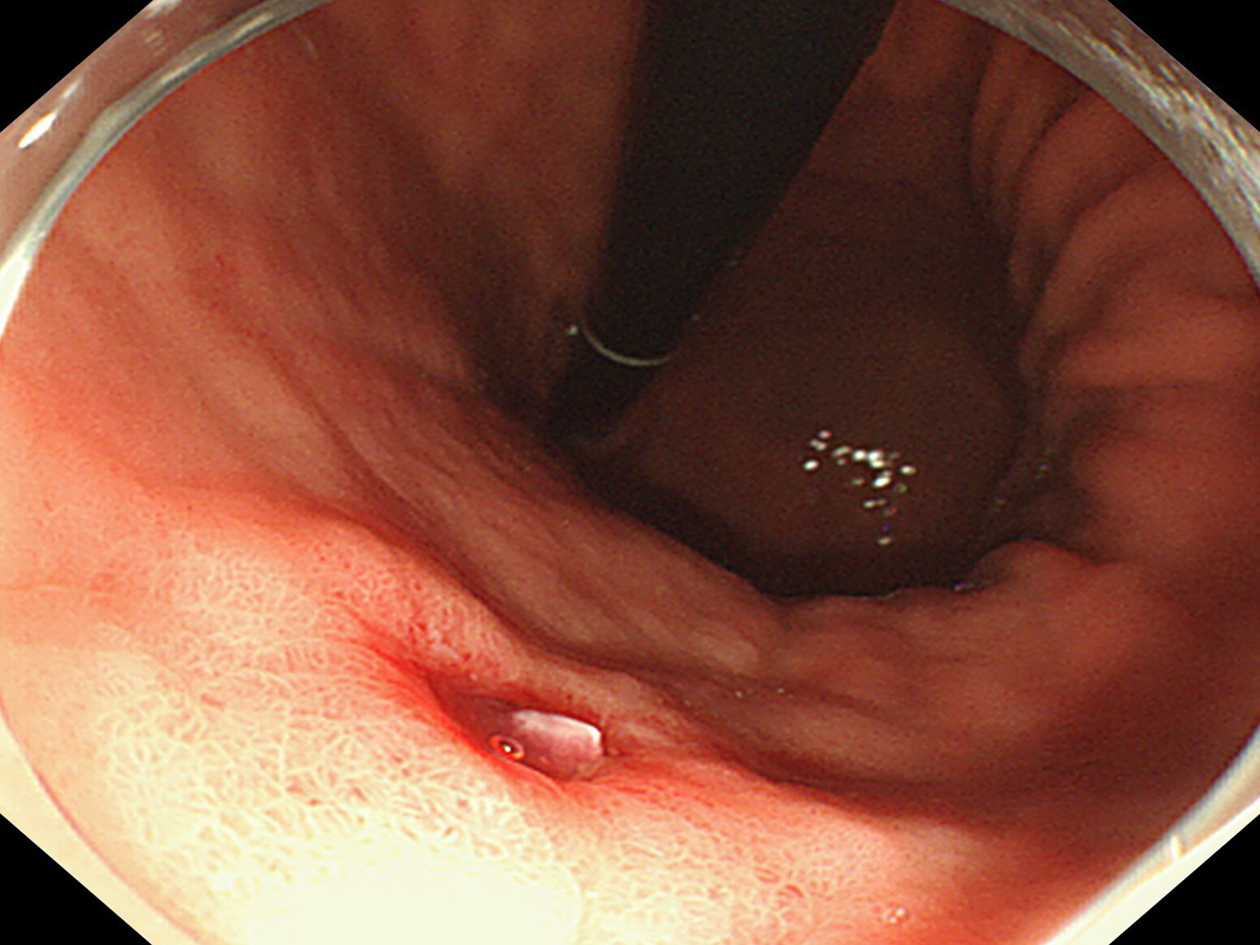
Figure 2 Dieulafoy’s lesion under white light endoscopy.
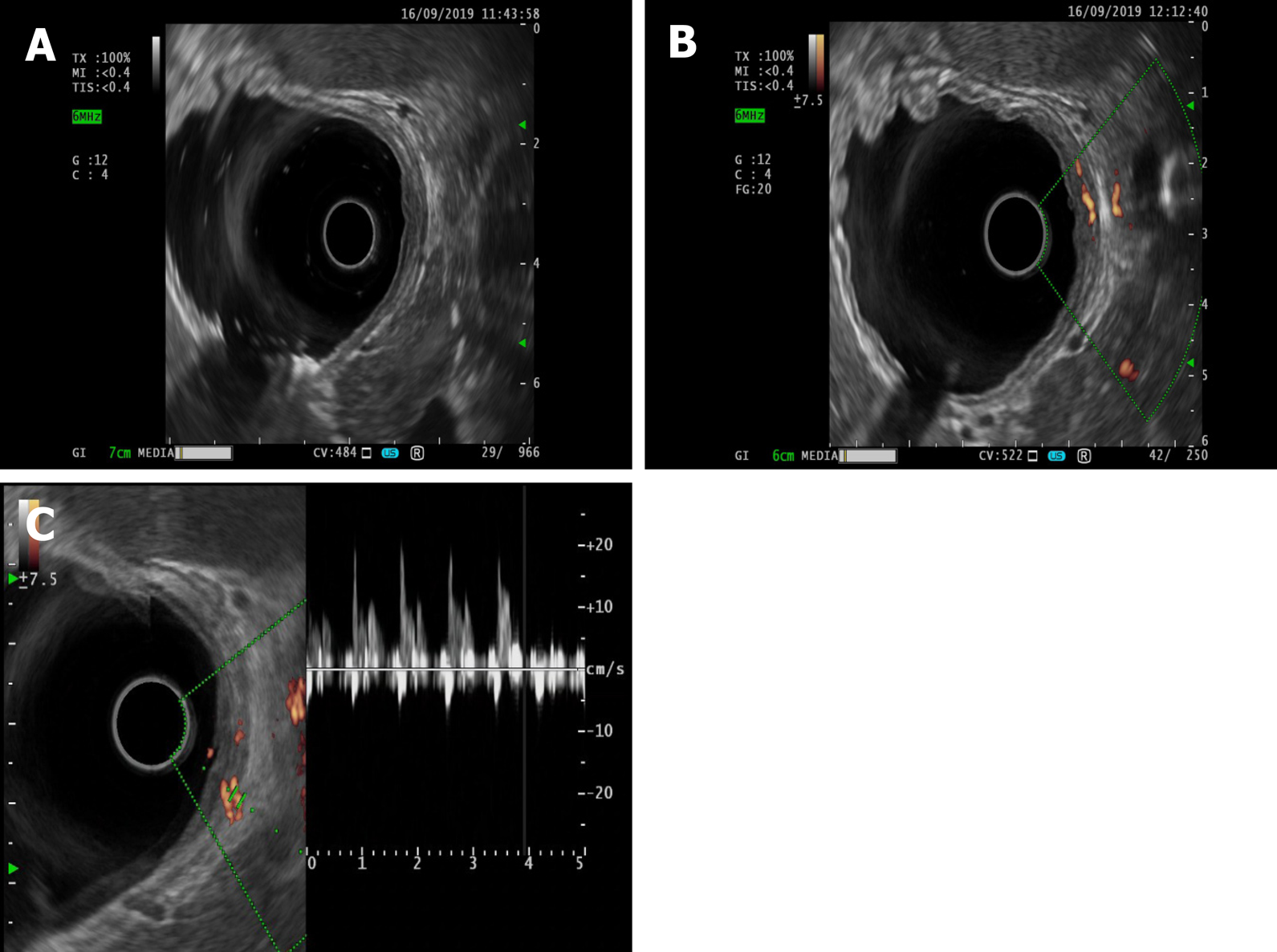
Figure 3 Endoscopic ultrasonography.
A: Dieulafoy’s lesion under endoscopic ultrasonography; B: Ultrasonic Doppler showing the blood flow signal of the mycomembrane muscle and submucosa in the lesion area; C: Doppler spectrum representing the arterial blood flow spectrum.
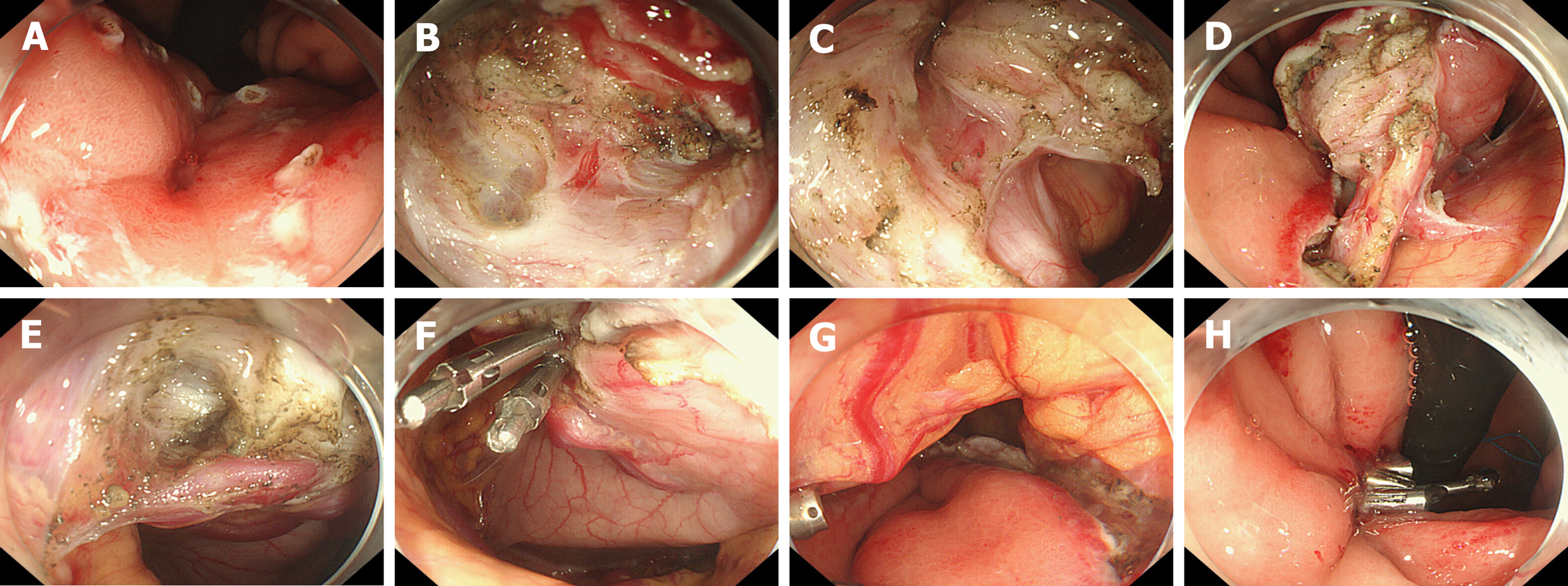
Figure 4 Operational procedures.
A: Mark the lesion; B: Dissect the lesion layer by layer; C: Cut the full thickness of the lesion through the stomach wall to the abdominal cavity; D: Provide traction to the lesion; E: Expose the large vessels on the serosal surface; F: Clip thick vessels on the serosal surface; G: Examine the wound postoperatively; H: Suture the wound.
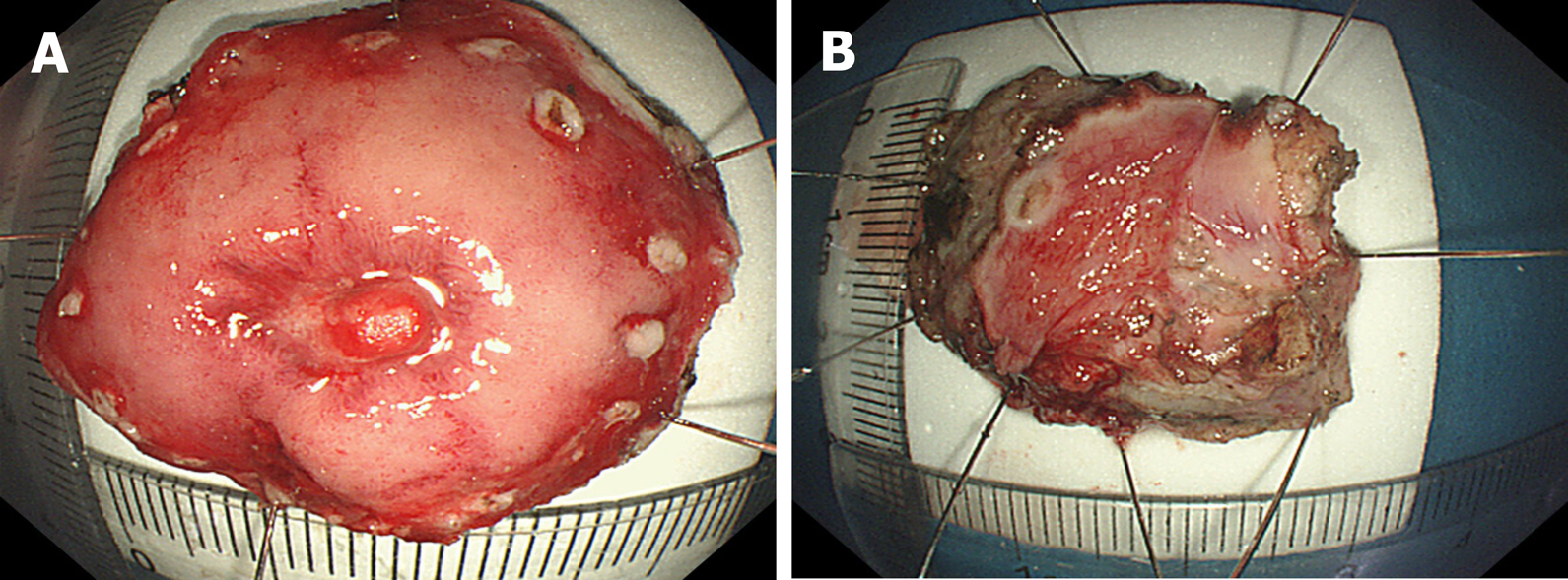
Figure 5 Excision of the specimen.
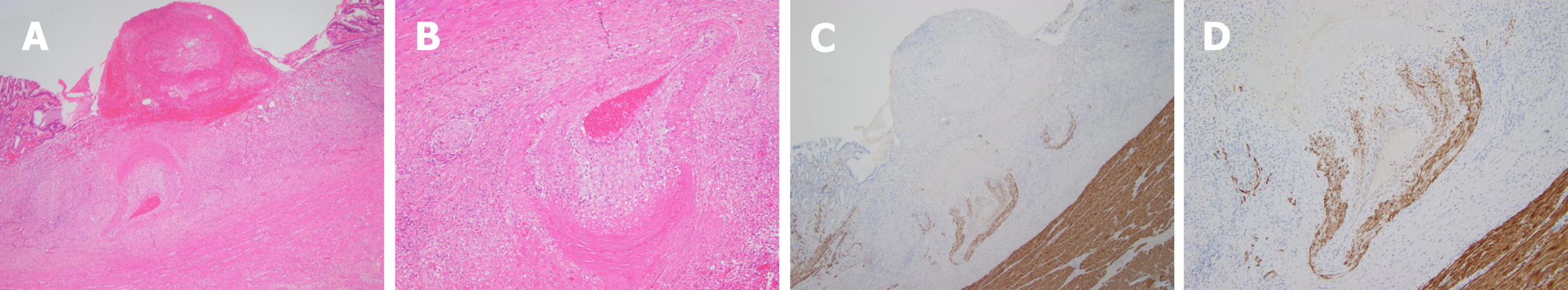
Figure 6 Postoperative pathology.
A: An ulcer that reached the muscular layer of the mucous membrane. Blood clots were present in the middle. There was denatured fibrous tissue at the bottom, a dilated and tortuous artery, intimal degeneration, vitreous degeneration of the smooth muscle near the ulcer side, and uneven thickness between the left and the right. Hematoxylin and eosin (HE) staining, × 40; B: Magnified image of Figure 6A. HE staining, × 100; C: Immunohistochemical desmin staining showing incomplete smooth muscle of the arterial wall and varying thickness, × 40; D: Magnified image of Figure 6C; magnification ×100.
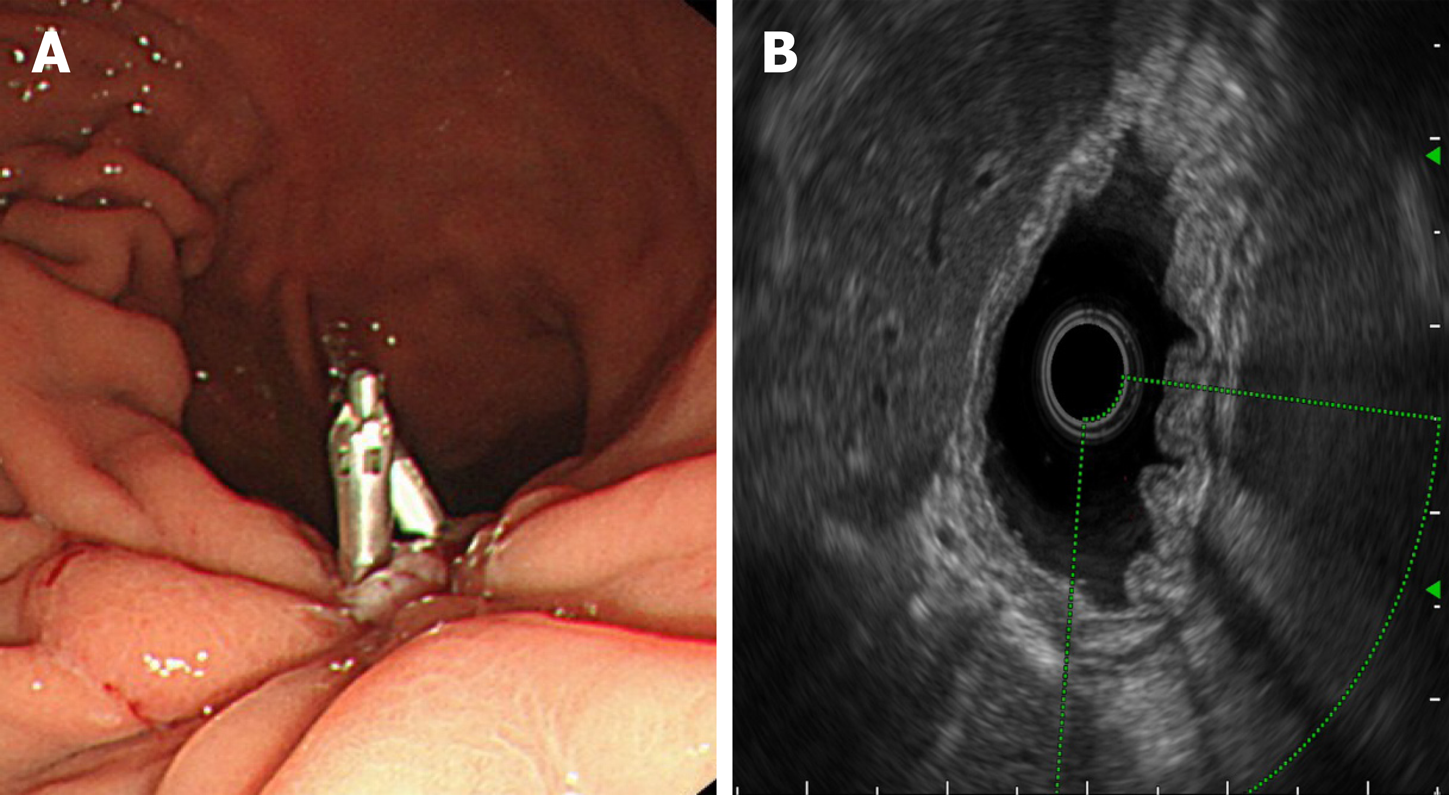
Figure 7 Endoscopic ultrasonography.
A: Wound healing, residual small ulcer and metal clip; B: Focus scar area showing thickening and hyperechoic changes, with no blood flow signals on ultrasonic Doppler.
- Citation: Yu S, Wang XM, Chen X, Xu HY, Wang GJ, Ni N, Sun YX. Endoscopic full-thickness resection to treat active Dieulafoy's disease: A case report. World J Gastroenterol 2020; 26(30): 4557-4563
- URL: https://www.wjgnet.com/1007-9327/full/v26/i30/4557.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i30.4557