Copyright
©The Author(s) 2019.
World J Gastroenterol. May 14, 2019; 25(18): 2149-2161
Published online May 14, 2019. doi: 10.3748/wjg.v25.i18.2149
Published online May 14, 2019. doi: 10.3748/wjg.v25.i18.2149
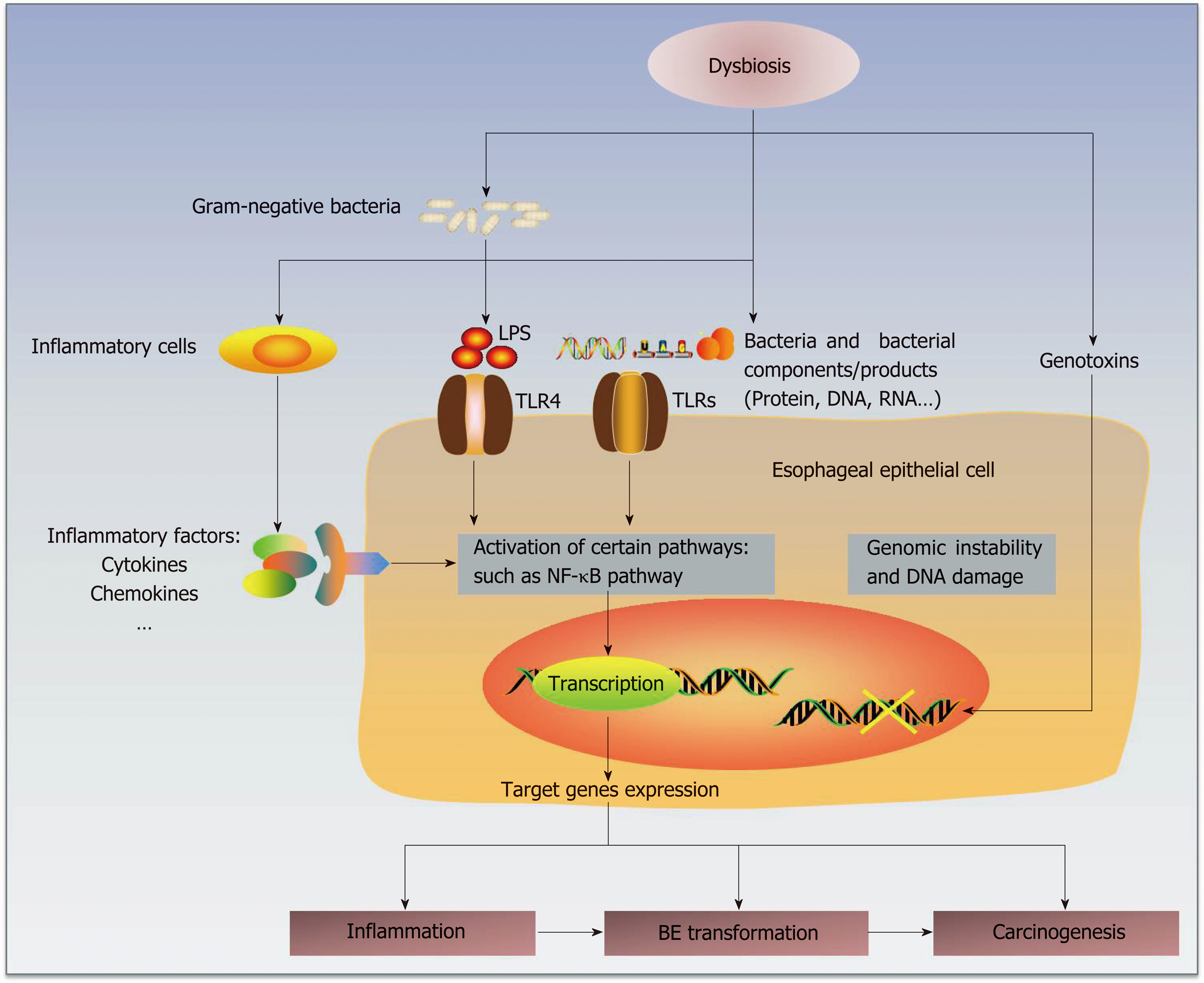
Figure 1 Hypothetical mechanisms by which the esophageal microbiota participates in the pathogenesis of Barrett's esophagus (BE) and esophageal adenocarcinoma (EAC).
The microbial dysbiosis in the esophagus is associated with abnormal esophagus. Normal esophagus harbors a larger proportion of gram-positive bacteria, whereas the microbiota in abnormal esophagus is dominated by gram-negative bacteria. This shift from a gram-positive aerobic microbiota to a gram-negative anaerobic microbiota may interact with inflammatory cells and promote the production and secretion of inflammatory factors, such as cytokines and chemokines. In addition, the increase in gram-negative bacteria and their components/products, including LPS, DNA and RNA, may stimulate TLRs (mainly TLR4). TLR4 expression in the esophageal epithelium of BE/EAC is upregulated. As the natural ligands of LPS, TLR4 may play an important role in pathogenesis, whose activation could trigger the NF-κB pathway. These interactions mentioned above may stimulate activation of certain intercellular signaling pathways, such as NF-κB. This activation may upregulate the expression of target genes. Moreover, genotoxins generated by some bacteria may cause genomic instability and DNA damage. The end effects might be the induction of inflammation, BE transformation and carcinogenesis. However, whether the microbiota plays a causative role in BE/EAC progression is still unclear. LPS: lipopolysaccharides; NF-κB: nuclear factor kappa B; TLRs: toll-like receptors; BE: Barrett's esophagus; EAC: Esophageal adenocarcinoma.
- Citation: Lv J, Guo L, Liu JJ, Zhao HP, Zhang J, Wang JH. Alteration of the esophageal microbiota in Barrett's esophagus and esophageal adenocarcinoma. World J Gastroenterol 2019; 25(18): 2149-2161
- URL: https://www.wjgnet.com/1007-9327/full/v25/i18/2149.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i18.2149