Copyright
©The Author(s) 2016.
World J Gastroenterol. Dec 21, 2016; 22(47): 10267-10274
Published online Dec 21, 2016. doi: 10.3748/wjg.v22.i47.10267
Published online Dec 21, 2016. doi: 10.3748/wjg.v22.i47.10267
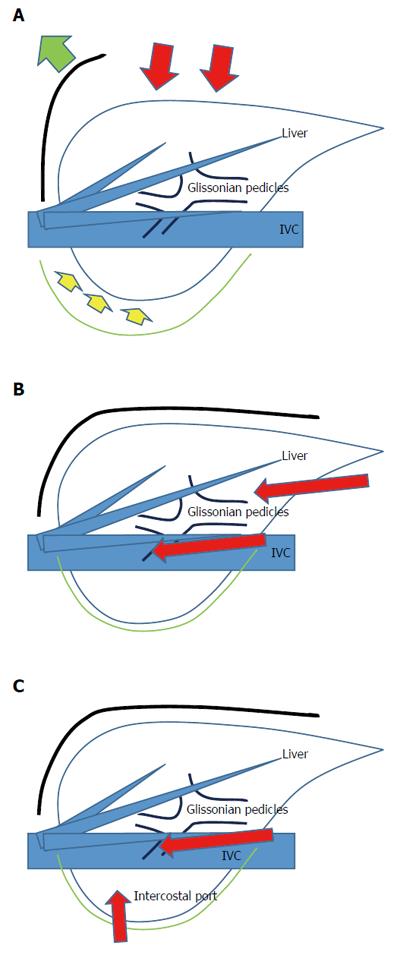
Figure 1 Liver resection (A), laparoscopic liver resection (regular caudal approach, B) and laparoscopic liver resection (lateral approach, C).
Red arrows indicate the directions of the view and manipulation in each approach. A: In the open approach, the subcostal cage containing the liver is opened with a large subcostal incision, and instruments are used to lift the costal arch. The liver is dissected and mobilized (lifted) from the retroperitoneum; B: In the regular laparoscopic caudal approach, the laparoscope and forceps are placed into the subcostal cage from caudal direction, and surgery is performed with minimal alteration and destruction of the associated structures; C: In the laparoscopic lateral approach, the intercostal (transdiaphragmatic) ports combined with total mobilization of the liver from the retroperitoneumcan allow the direct lateral approach into the cage and to the posterosuperior tumors.
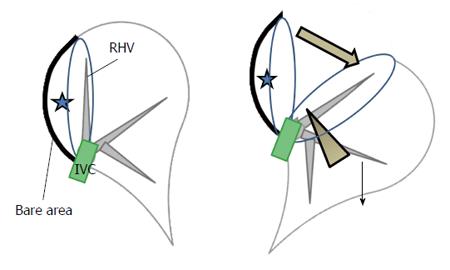
Figure 2 Schema of the caudal approach for laparoscopic posterior sectionectomy with prior transection without mobilization in the left lateral position.
Stars denote the tumor in the posterior section of the liver. The left image shows the organ pre-transection, and the right image shows the organ during transection. The transection was performed in one direction from the caudal edge of the liver, with exposure of the inferior vena cava (IVC) and the right hepatic vein on the cutting plane (arrow head, right). This procedure facilitates exposure of the cutting plane (thick arrow, right) between the retroperitoneal-fixed resected liver and the remnant liver, which has fallen downward by gravity (thin arrow, right). The decreased venous pressure in the right hepatic vein, vertically standing up from the IVC, leads to decreased intraoperative bleeding. Finally, the oncological benefit is the same as the anterior approach in open right hepatectomy.
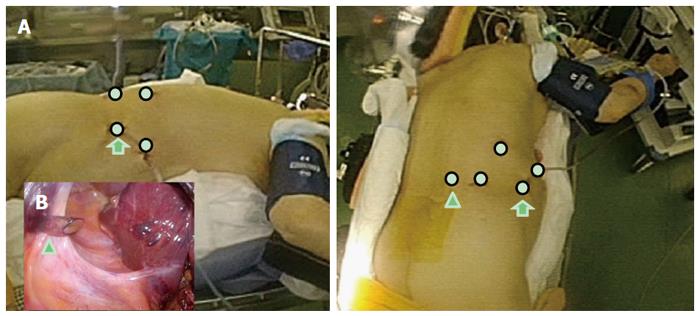
Figure 3 Schema of the settings for semi-prone positioning and port placement.
A: The patient is placed in the semi-prone position (left-lateral view, right-caudal view). The white circles indicate the locations for the ports; the arrowhead indicates the port in the para-vertebra area; the arrows indicate the port mainly used for laparoscope; B: The arrowhead indicates the port in the para-vertebra area, as seen under the view of laparoscope inside the abdomen. Morrison’s pouch is well-opened in the semi-prone position, with the gravity-assisted movement of the organs, and the port is easily inserted into the area.
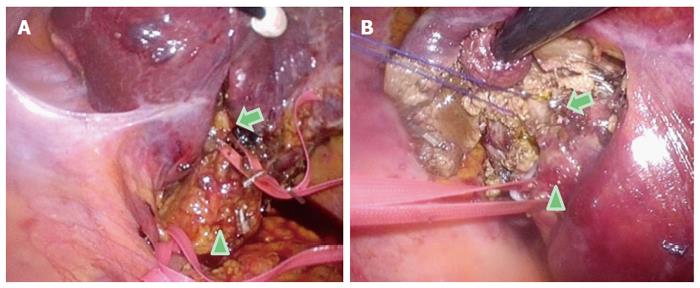
Figure 4 Intraoperative findings of Glissonian pedicles during the semi-prone position caudal approach for segment 7 segmentectomy.
For the segment (S) 7 segmentectomy, a good view and access to the right part of the hilar plate, posterior and the S7 Glissonian pedicles are established upon flipping-up of the liver S6 and of the gallbladder in the left upward direction. A: The arrowhead indicates the hepatoduodenal ligament encircled with tape; the arrow indicates the posterior branch of the Glissonian pedicle encircled with tape in the Rouviere’s sulcus; B: The arrowhead indicates the posterior branch of the Glissonian pedicle encircled with tape; the arrow shows the S7 branch of the Glissonian pedicle encircled with string.
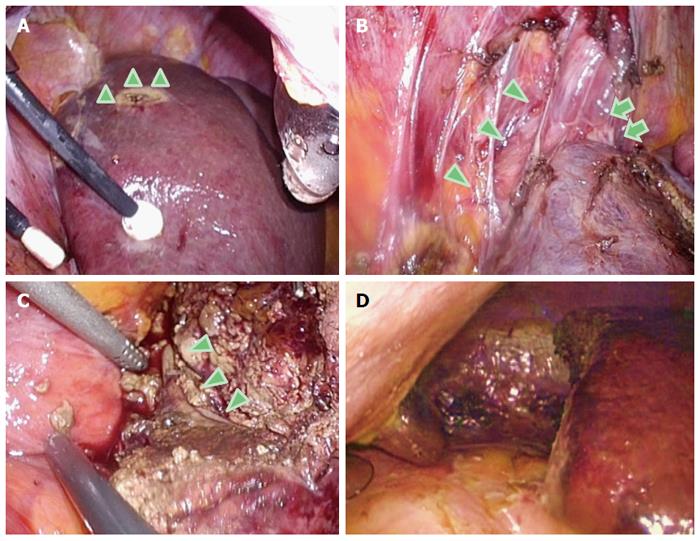
Figure 5 Intraoperative findings in the caudal approach for S7 segmentectomy in the semi-prone position.
A: Dissection and mobilization are easily performed, since the liver is hanging down from the retroperitoneum. The arrowheads indicate the tension on the retroperitoneum; B: The inferior vena cava (arrowheads) and the root of the right hepatic vein (arrows) are easily recognized and dissected after the liver mobilization from the right dorsal side; C: The right hepatic vein (arrowheads) is exposed on the transection plane in the S7 segmentectomy. This procedure is safely performed on the well-opened transection plane; D: After completion of the resection, a clear and stable view of the subphrenic area is obtained.
- Citation: Morise Z. Laparoscopic liver resection for posterosuperior tumors using caudal approach and postural changes: A new technical approach. World J Gastroenterol 2016; 22(47): 10267-10274
- URL: https://www.wjgnet.com/1007-9327/full/v22/i47/10267.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i47.10267