Copyright
©The Author(s) 2016.
World J Gastroenterol. Jan 7, 2016; 22(1): 446-466
Published online Jan 7, 2016. doi: 10.3748/wjg.v22.i1.446
Published online Jan 7, 2016. doi: 10.3748/wjg.v22.i1.446
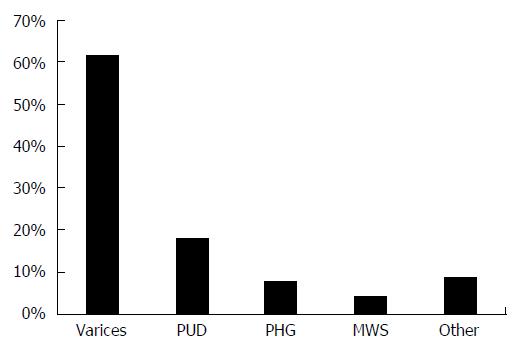
Figure 1 Reported distribution of common etiologies of upper gastrointestinal bleeding in patients with cirrhosis.
Frequency distribution of the etiologies of upper gastrointestinal bleeding in patients with cirrhosis. Varices include esophageal or gastric varices. Adapted from Ref. [39,44-47]. PUD: Peptic ulcer disease; PHG: Portal hypertensive gastropathy; MWS: Mallory-Weiss syndrome; Other: Other etiologies of upper gastrointestinal bleeding.
Figure 2 Seventy-year-old male with Child-Pugh class A alcoholic cirrhosis presented with hematemesis, melena, and orthostatic dizziness.
Esophagogastroduodenoscopy (EGD) revealed an acute 14 mm × 5 mm ulcer in the distal duodenal bulb with stigma of recent hemorrhage (SRH) represented by a prominent, nonbleeding, flat, pigmented spot; trace esophageal varies with no SRH, such as wale bites; and no portal hypertensive gastropathy. Note the deep erosion adjacent to the ulcer. The etiology of the ulcer was idiopathic. The patient had no history of taking nonsteroidal anti-inflammatory drugs or aspirin. Pathologic examination of gastric biopsies taken at EGD revealed no Helicobacter pylori. No endoscopic therapy was performed because the only SRH was a flat pigmented spot which has a low risk of rebleeding. The patient, however, required transfusion of 4 units of packed erythrocytes. The patient was treated medically with pantoprazole with no recurrence of the bleeding. This patient illustrates that peptic ulcers are in the differential of acute upper gastrointestinal bleeding in a patient with cirrhosis, even in the absence of risk factor for peptic ulcers, and that bleeding from peptic ulcers in cirrhotic patients may be unusually severe.
- Citation: Nojkov B, Cappell MS. Distinctive aspects of peptic ulcer disease, Dieulafoy's lesion, and Mallory-Weiss syndrome in patients with advanced alcoholic liver disease or cirrhosis. World J Gastroenterol 2016; 22(1): 446-466
- URL: https://www.wjgnet.com/1007-9327/full/v22/i1/446.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i1.446