Copyright
©The Author(s) 2016.
World J Gastroenterol. Jan 7, 2016; 22(1): 126-144
Published online Jan 7, 2016. doi: 10.3748/wjg.v22.i1.126
Published online Jan 7, 2016. doi: 10.3748/wjg.v22.i1.126
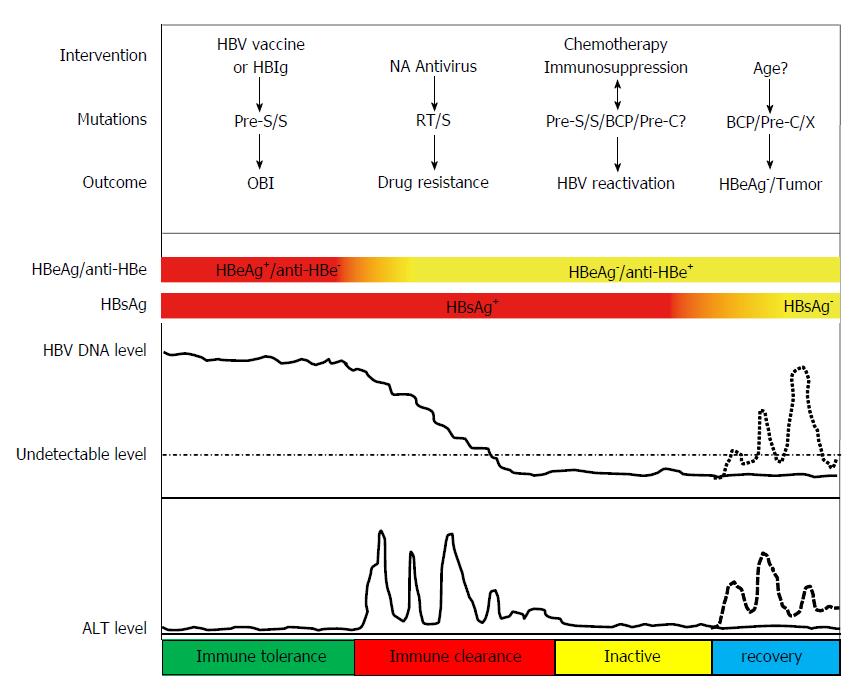
Figure 1 Interventions, mutations and clinical outcomes in the natural history of hepatitis B virus infection.
The natural history of hepatitis B virus (HBV) infection is typically classified into 4 phases: immune tolerant, immune clearance, inactive and recovery phase. Patients who receive HBV vaccine and/or hepatitis B immunoglobulin (HBIg) injection may develop chronic HBV infection with PreS and/or S gene mutations, this phenomenon is called occult HBV infection (OBI); during the immune clearance phase, long-term use of NAs can select for mutations in the reverse transcriptase (RT) and S regions; HBV reactivation may occur during the inactive phase in patients with hepatitis B surface antigens (HBsAg) and/or anti-HBc positive after chemotherapy or immunosuppression. HBV isolated from these patients may harbor mutations in the PreS, S, basal core promoter (BCP) or Pre-C regions. The causal relationship between these mutations and chemotherapy or immunosuppression is unclear; with increasing age, some patients can develop BCP, Pre-C or X region mutations or HBV DNA integration leading to hepatitis B e antigen (HBeAg) negativity or tumor.
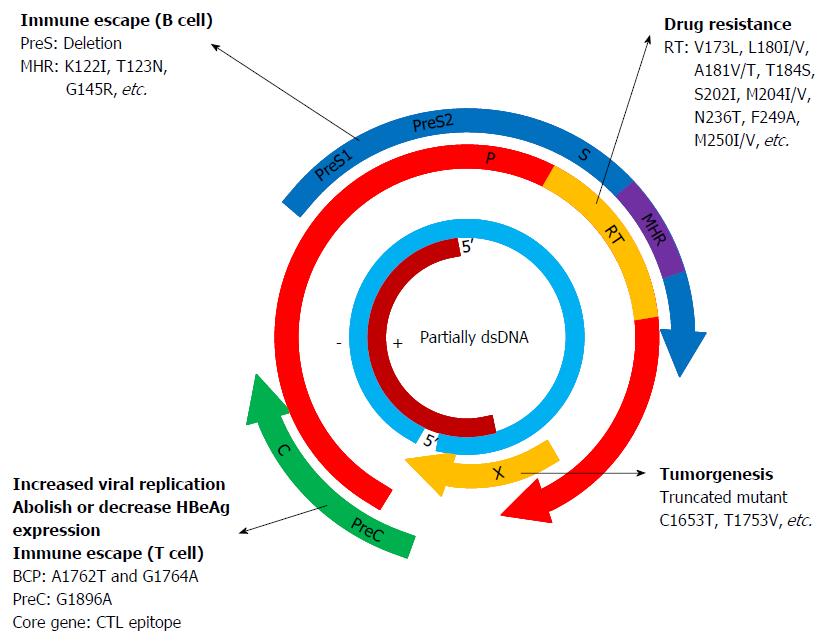
Figure 2 Hepatitis B virus genome and the major gene mutation types in hepatitis B virus open reading frames.
The hepatitis B virus (HBV) genome is a 3.2 kb double-stranded DNA molecule that is organized into four open reading frames: the polymerase, the envelope, the precore and X. The deletion mutations in the PreS gene region and/or some point mutations in the major hydrophilic region (MHR) of S gene can lead to immune escape and occult HBV infection; mutations in reverse transcriptase (RT) can lead to drug resistance after long-term use of nucleotide analogues and this drug-resistant HBV typically has an altered viral envelope of hepatitis B surface antigen because of the overlap between the polymerase and envelope, for example, A181T/V mutations in the RT region can cause W172* (stop codon mutation), W172L and L173F mutations in the S region. M204V/I mutations in the RT region can result in I195M, W196* (stop codon mutation), W196S and W196L mutations in the S region; A1762T and G1764A mutations in the base core promotor (BCP) or G1896A mutation in PreC can increased viral replication, abolish or decrease HBeAg expression. Some mutations in the CTL epitope of HBV core gene can cause T cell immune escape; some point mutations or truncated mutants in the HBV X gene can cause tumorigenesis or other end-stage liver disease.
- Citation: Zhang ZH, Wu CC, Chen XW, Li X, Li J, Lu MJ. Genetic variation of hepatitis B virus and its significance for pathogenesis. World J Gastroenterol 2016; 22(1): 126-144
- URL: https://www.wjgnet.com/1007-9327/full/v22/i1/126.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i1.126