Copyright
©The Author(s) 2015.
World J Gastroenterol. Feb 7, 2015; 21(5): 1554-1566
Published online Feb 7, 2015. doi: 10.3748/wjg.v21.i5.1554
Published online Feb 7, 2015. doi: 10.3748/wjg.v21.i5.1554
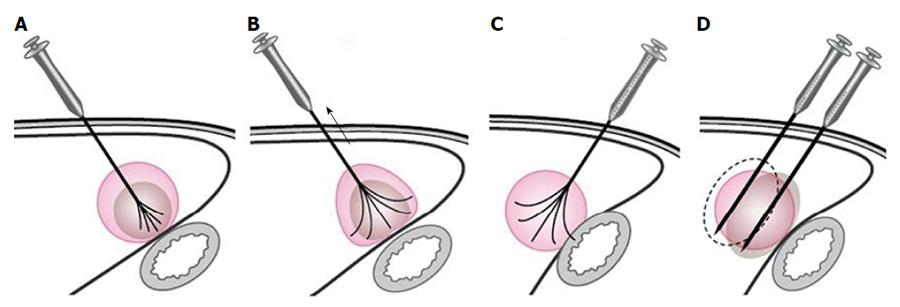
Figure 1 Diagram for ablation of a tumor near the bowel.
A: The multiple-tined electrode was inserted into the tumor perpendicular to the bowel wall, and the needle was expanded to 3 cm; B: When expanding the radiofrequency ablation (RFA) prongs from 3 cm to 4-5 cm to ablate a tumor area near the bowel, the RFA electrode was retracted slightly to draw the tumor away from the bowel. While fixing the electrode shaft in this position, the movable hub was pushed to expand the prongs; C: If the RFA electrode was inserted into the tumor parallel to the bowel wall, there is a higher risk for bowel injury when deploying the electrode tines; D: With a mono-polar electrode, the puncture direction was parallel to the wall of the adjacent bowel.
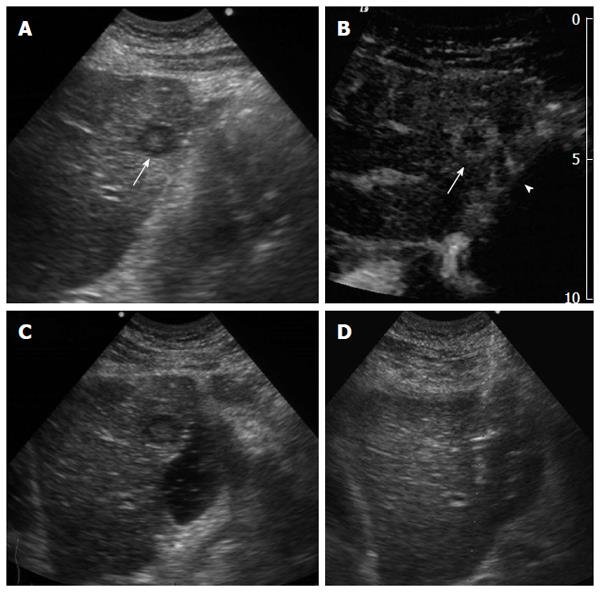
Figure 2 Artificial ascites was used between tumors and nearby bowels before and during the ablation.
Figure 3 A 71-year-old man had intrahepatic recurrence after resection of hepatocellular carcinoma.
A: Subcostal ultrasound shows a 1.2-cm tumor (arrow) in segment III; B: Contrast-enhanced ultrasound shows the tumor (arrow) peripherally enhanced and that its invasive range increased to 2.2 cm. The tumor is shown to be very close to the gastrointestinal (GI) tract (arrow head); C: Subcostal ultrasound shows an ultrasound-guided tiny needle puncture though the liver to the space between the liver and the bowel. After injection of 100 mL of fluid, the tumor is separated from the nearby GI tract; D: Subcostal ultrasound shows that two bipolar electrodes are placed parallel to the GI tract.
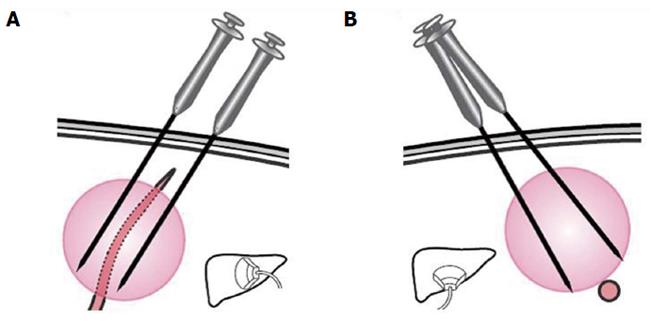
Figure 4 Schematic presentation of a liver tumor near a large vessel that was ablated with two mono-polar electrodes.
Radiofrequency ablation was applied at bilateral sides of the large vessel. A: Longitudinal section view; B: Transverse section view.
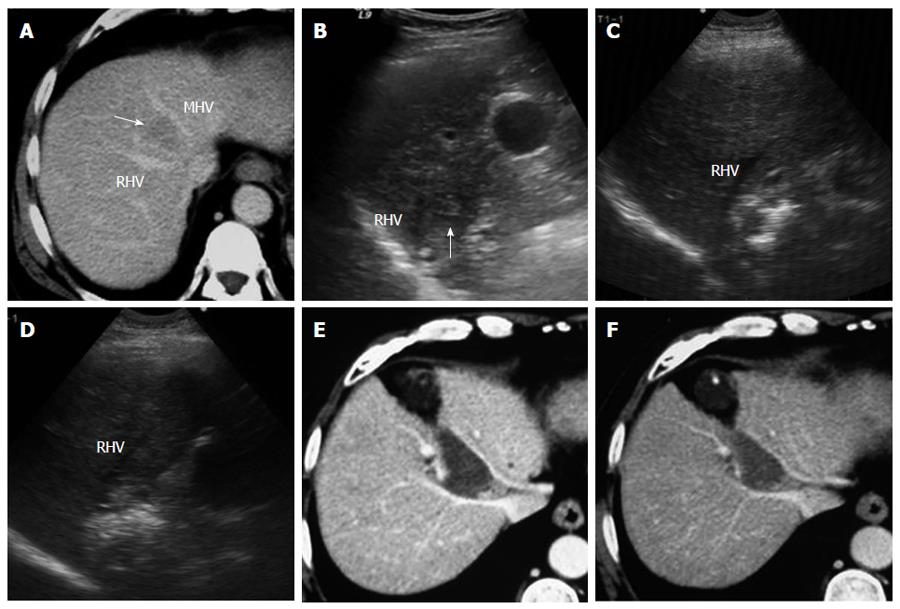
Figure 5 A 54-year-old man with hepatocellular carcinoma.
A: Contrast-enhanced transverse computed tomography (CT) image shows a 2.6-cm tumor (arrow) in segment VIII between the middle hepatic vein (MHV) and the right hepatic vein (RHV); B: Intercostal ultrasound shows that the tumor (arrow) is located next to RHV; C: Intercostal ultrasound shows that the tumor is treated by ultrasound-guided RF ablation. Two bipolar electrodes are inserted parallel to the RHV; D: Intercostal ultrasound immediately after RF ablation shows the hepatic veins remain normal; E: Contrast-enhanced transverse CT image obtained 1 mo later shows that a coagulation area is surrounded by hepatic veins with no enhancement. No injury to the large vessels occurred in this patient; F: Contrast-enhanced transverse CT image obtained 5 mo later shows a coagulation area without viability.
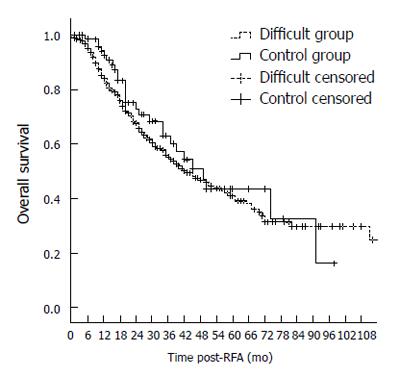
Figure 6 Graph shows the overall survival of hepatocellular carcinoma patients after radiofrequency ablation in different groups.
The 1-, 3-, 5-, and 7-year overall survival rates in the difficult group were similar to those in the control group (84.3%, 54.4%, 41.2%, and 29.9% vs 92.5%, 60.3%, 43.2%, and 32.8%, respectively, P = 0.371). RFA: Radiofrequency ablation.
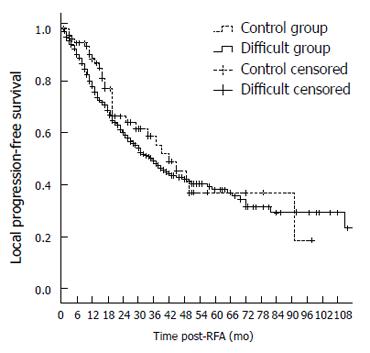
Figure 7 Graph shows the local progression-free survival of hepatocellular carcinoma patients after radiofrequency ablation in different groups.
The 1-, 3-, 5-, and 7-year local progression-free survival rates in the difficult group were not significantly different from those in the control group (77.9%, 49.0%, 38.0%, and 29.1% vs 88.3%, 55.6%, 36.3%, and 36.3%, respectively, P = 0.584). RFA: Radiofrequency ablation.
- Citation: Yang W, Yan K, Wu GX, Wu W, Fu Y, Lee JC, Zhang ZY, Wang S, Chen MH. Radiofrequency ablation of hepatocellular carcinoma in difficult locations: Strategies and long-term outcomes. World J Gastroenterol 2015; 21(5): 1554-1566
- URL: https://www.wjgnet.com/1007-9327/full/v21/i5/1554.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i5.1554