Copyright
©The Author(s) 2015.
World J Gastroenterol. Nov 7, 2015; 21(41): 11502-11521
Published online Nov 7, 2015. doi: 10.3748/wjg.v21.i41.11502
Published online Nov 7, 2015. doi: 10.3748/wjg.v21.i41.11502
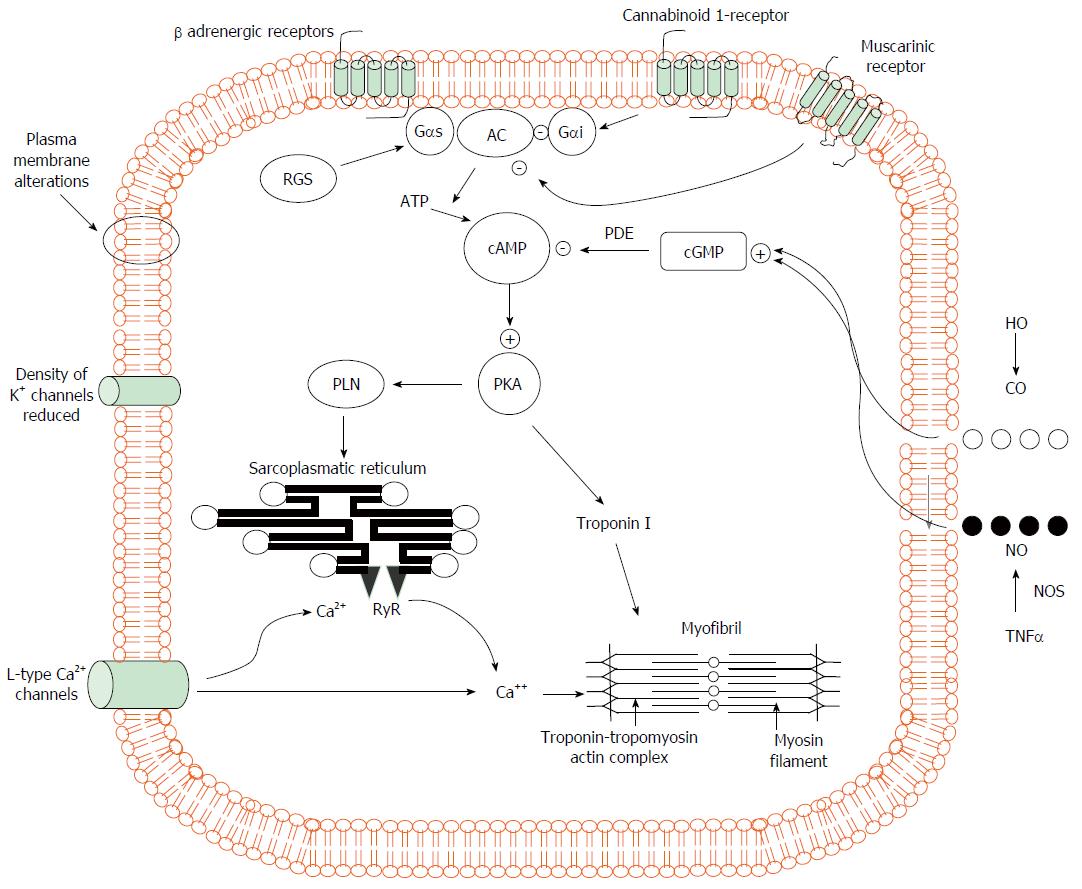
Figure 1 Pathogenic mechanisms of cardiomyocyte contraction in experimental cirrhosis.
Cardiomyocytes of cirrhotic animals showed reduced contractility via impairment of the βAR signalling (down-regulation, desensitization) which in turn leads to a reduction in βAR density, Gs proteins, and AC activity with resultant decreased cAMP generation. This second messenger cAMP, phosphorylates several proteins leading to intracellular calcium fluxes, calcium release and myocyte contraction. Postreceptor signaling through cAMP is severely impaired. In addition, the decreased fluidity of cardiomyocyte membrane interferes with the function of βAR, L-type calcium and potassium channels and impair stimulation of muscarinic acetylcholine receptors. The activation of CB1 inhibiting L-type calcium channels and AC together with increased NO and CO levels via a cGMP-dependent mechanism also contribute to decreased calcium ion influx or release from the sarcoplasmic reticulum with a related fall of calcium ion content and contractility. +: stimulatory influence; -: inhibitory influence. βAR: β-adrenergic receptors; CB1: Cannabinoid 1-receptor; AC: Adenylcyclase; cAMP: Cyclic adenosine monophosphate; Gαi: Inhibitory G protein; Gαs: Stimulatory G protein; RGS: Regulator of G-protein signaling; PLN: Phosphoslamban; PKA: Protein kinase A; cGMP: Cyclic guanosine monophosphate; PDE: Phosphosdiesterase; RyR: Ryanodine receptor; HO: Haemoxygenase; CO: Carbon monoxide; NO: Nitric oxide; NOS: Nitric oxide synthase; TNFα: Tumour necrosis factor α.
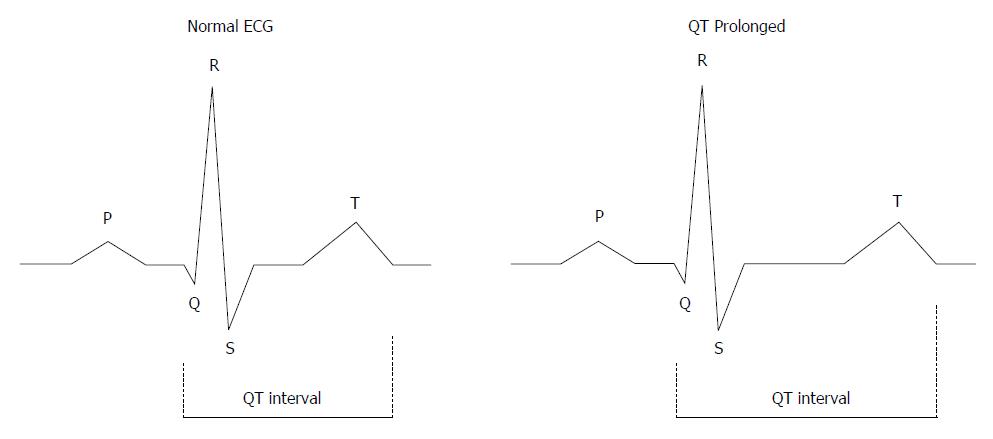
Figure 2 The QT interval.
The QT interval is a measure of the time between the start of the Q wave and the end of the T wave in the heart during electrical cycle. The QT interval is dependent on the heart rate and needs to be corrected by heart rate. The corrected QT interval (QTc) estimates the QT interval at a heart rate of 60 bpm. The standard clinical correction in cirrhosis uses Fredericia’s formula: QTc = QT/RR1/3. The RR interval is given in seconds (RR interval = 60/heart rate). QTc is prolonged if > 450 ms in men or > 470 ms in women. QTc interval prolongation is due to altered repolarization.
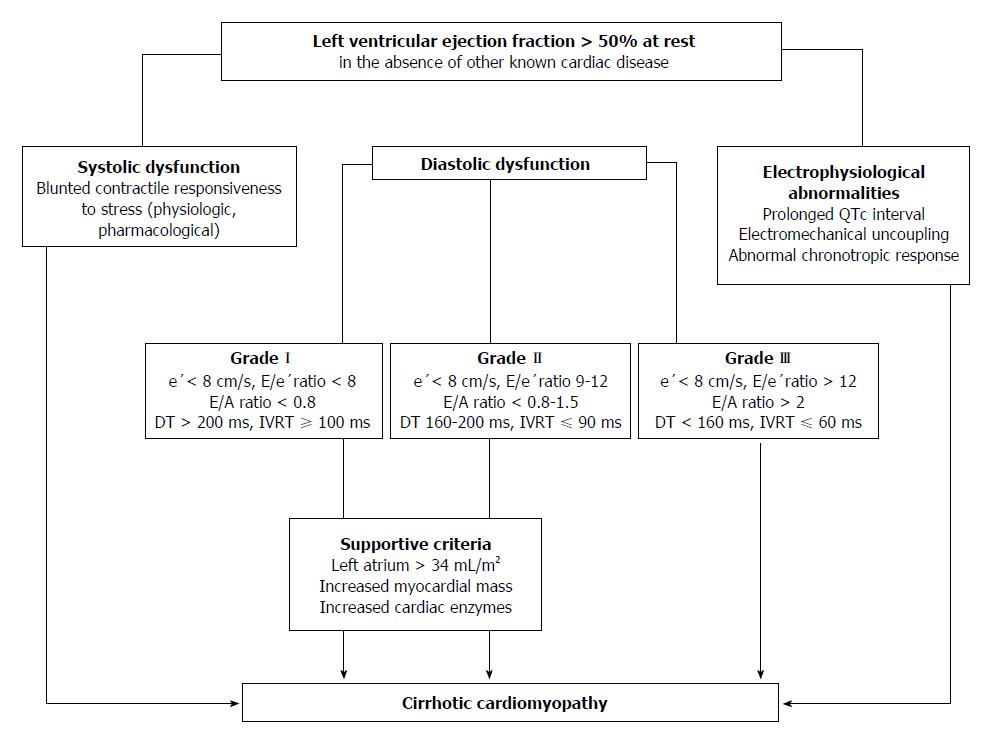
Figure 3 Algorithm for the diagnosis of cirrhotic cardiomyopathy.
Three ways to diagnose CCM with normal EF at rest have been displayed: (1) Systolic function. Patients have documented blunted responsiveness to volume and postural challenge, exercise, or pharmacological infusion but the manoeuvres that can bring systolic dysfunction have not been standardized yet; (2) Diastolic function. The diagnosis of LVDD can be obtained by TDI (E/e′ > 15). If TDI yields an E/e′ ratio (8 < E/e′ < 15) other echocardiographic investigations such as blood flow Doppler of mitral valve or pulmonary veins, LV mass index or left atrial volume index are required for diagnostic of LVDD; (3) Electrophysiological abnormalities. a, the prolongation of the electrocardiographic corrected QT interval is common in cirrhosis; b, electromechanical uncoupling is a dyssynchrony between electrical and mechanical systole. The electrical systole is longer in patients with cirrhosis; c, chronotropic incompetence is the inability of the heart to proportionally increase HR in response to stimuli (exercise, tilting, paracentesis, infections and pharmacological agents). CCM: Cirrhotic cardiomyopathy; EF: Ejection fraction; LVDD: Left ventricular diastolic dysfunction; TDI: Tissue Doppler imaging; e’: Peak early diastolic velocity at the basal part of the septal and lateral corner of the mitral annulus; E/e’ratio: Peak E-wave transmitral/early diastolic mitral annular velocity; E/A ratio: Early diastolic mitral inflow velocity/late diastolic velocity; DT: Deceleration time; IVRT: Isovolumic relaxation time.
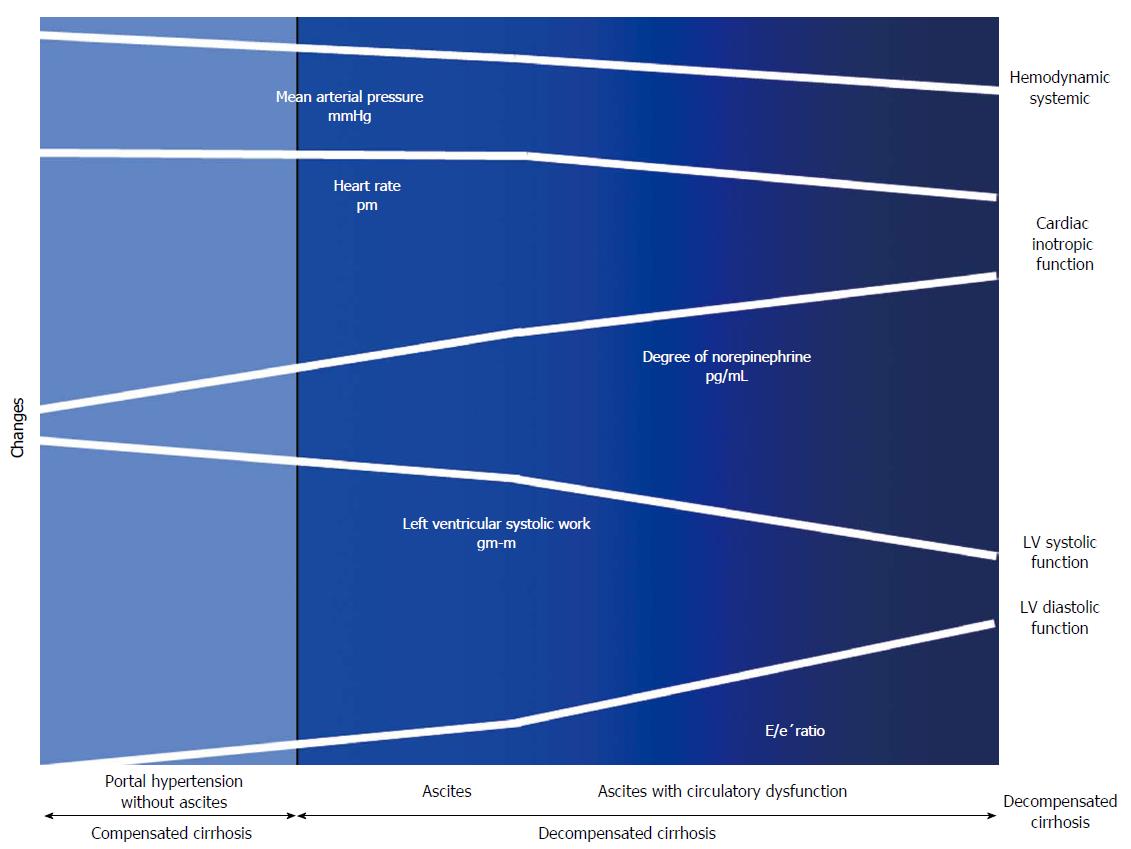
Figure 4 Cardiac and circulatory dysfunction according to presence of compensated and decompensated cirrhosis.
There is a progressive splanchnic arterial vasodilatation due to the overproduction of vasodilator molecules. Initially, circulatory homeostasis is maintained by the development of a hyperdynamic circulation. Later during the course of decompensated cirrhosis, patients develop an activation of the vasoconstrictor systems to maintain arterial pressure. In subsequent stages, the progressive decrease in cardiac afterload is not followed by an increase in HR and CO due to a decrease in cardiac function. Finally, in the advanced phase, when impairment of effective arterial blood volume is extreme, patients showed increased activity of NE concentration, arterial hypotension and reduced LVSF (CO and LV stroke work), and cardiac chronotropic function, and a higher degree in LVDD (E/e’) as compared to those with ascites, but normal NE, or without ascites. E/e’ratio: Peak E-wave transmitral/Peak early diastolic mitral annular velocity.
- Citation: Ruiz-del-Árbol L, Serradilla R. Cirrhotic cardiomyopathy. World J Gastroenterol 2015; 21(41): 11502-11521
- URL: https://www.wjgnet.com/1007-9327/full/v21/i41/11502.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i41.11502