Copyright
©The Author(s) 2015.
World J Gastroenterol. Aug 28, 2015; 21(32): 9614-9622
Published online Aug 28, 2015. doi: 10.3748/wjg.v21.i32.9614
Published online Aug 28, 2015. doi: 10.3748/wjg.v21.i32.9614
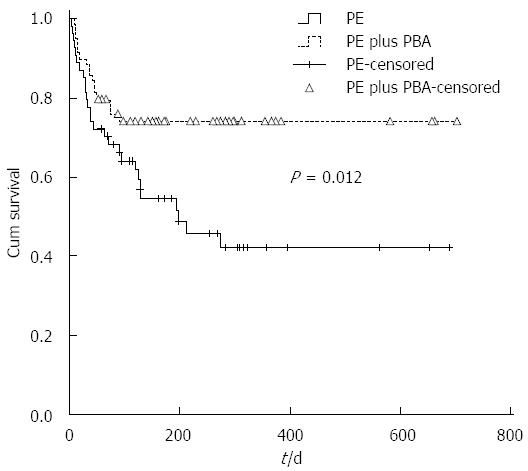
Figure 1 Comparing survival in patients with acute-on-chronic liver failure treated with different types of artificial liver support systems.
The Kaplan-Meier curves were calculated to compare the overall survival probability between acute-on-chronic liver failure patients who underwent plasma exchange (PE) vs those treated with PE plus plasma bilirubin adsorption (PBA).
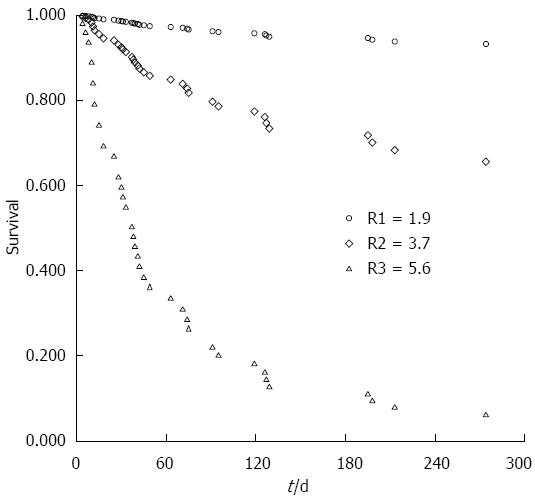
Figure 2 Prospective survival probabilities of three assumed acute-on-chronic liver failure patients.
According to the equation in Table 3, the prospective survival probabilities can be computed in individual acute-on-chronic liver failure patients with scores of 1.9, 3.7, and 5.6, respectively.
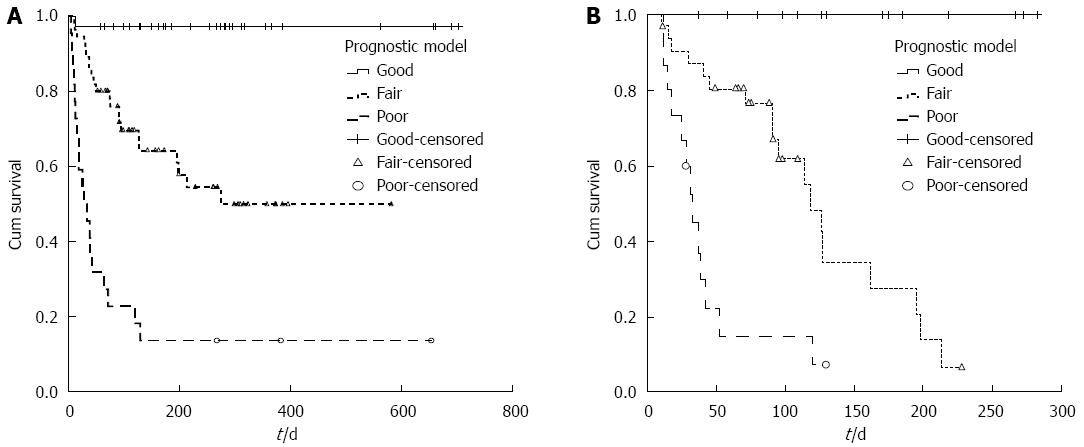
Figure 3 Survival probabilities of acute-on-chronic liver failure patients with different prognoses.
The Kaplan-Meier curves were drawn to contrast survival probabilities among acute-on-chronic liver failure patients whose prognoses were estimated to be good, fair, and poor, according to the risk scores calculated by the new model in the derivation cohort (A) and validation cohort (B).
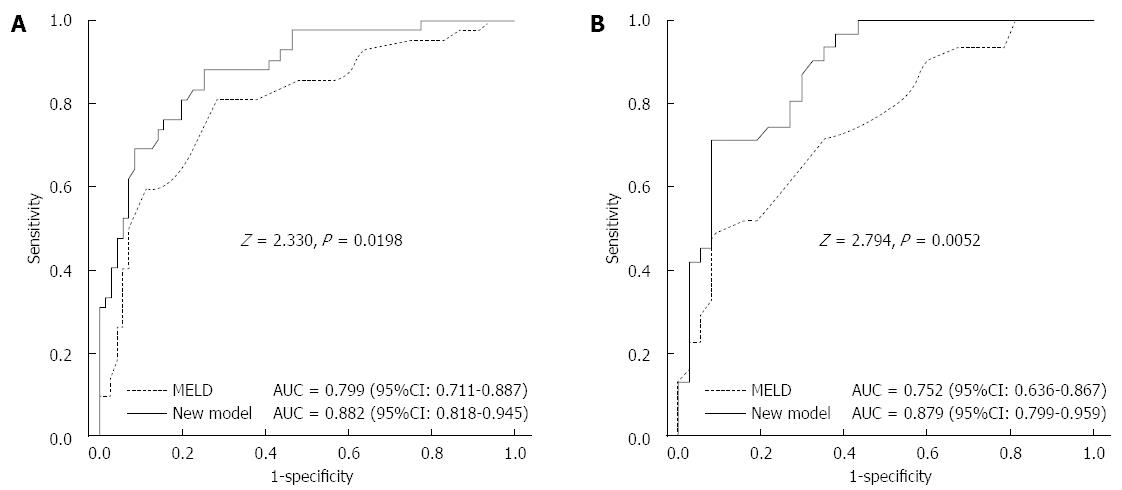
Figure 4 Comparison of the predictive accuracy for survival between the new model and the model for end-stage liver disease.
The area under the receiver-operating characteristic curve (AUC) with 95%CI of the new model and model for end-stage liver disease was 0.882 (0.818-0.945) and 0.799 (0.711-0.887), respectively, in the derivation cohort (A) and 0.879 (0.799-0.959) and 0.752 (0.636-0.867), respectively, in the validation cohort (B).
- Citation: Zhou PQ, Zheng SP, Yu M, He SS, Weng ZH. Prognosis of acute-on-chronic liver failure patients treated with artificial liver support system. World J Gastroenterol 2015; 21(32): 9614-9622
- URL: https://www.wjgnet.com/1007-9327/full/v21/i32/9614.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i32.9614