Copyright
©The Author(s) 2015.
World J Gastroenterol. Jul 14, 2015; 21(26): 7970-7987
Published online Jul 14, 2015. doi: 10.3748/wjg.v21.i26.7970
Published online Jul 14, 2015. doi: 10.3748/wjg.v21.i26.7970
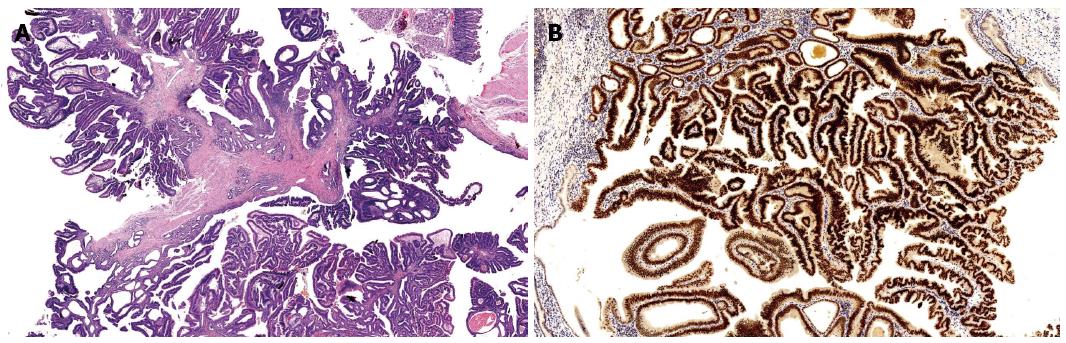
Figure 1 Intestinal type adenocarcinoma HE (A) and CDX2 (B).
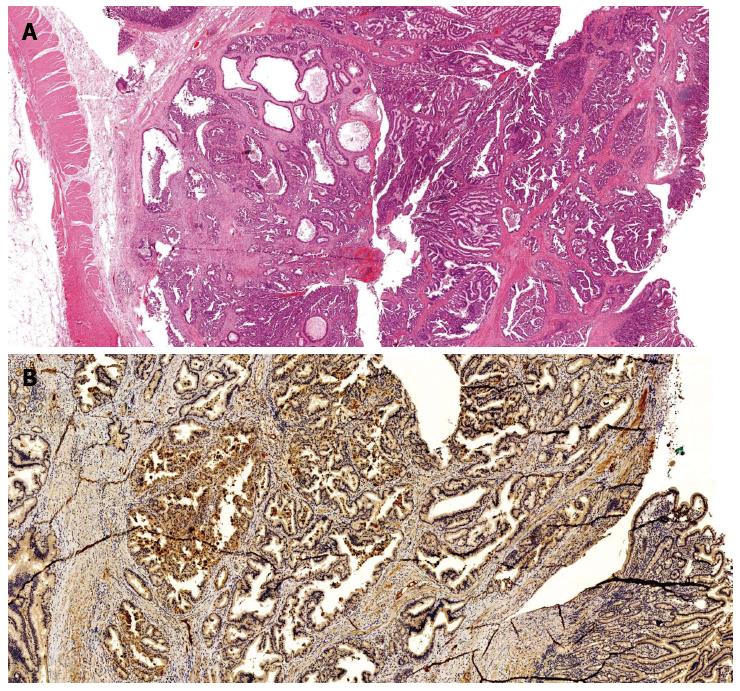
Figure 2 Pancreatobiliary type adenocarcinoma HE (A) and MUC1 (B).
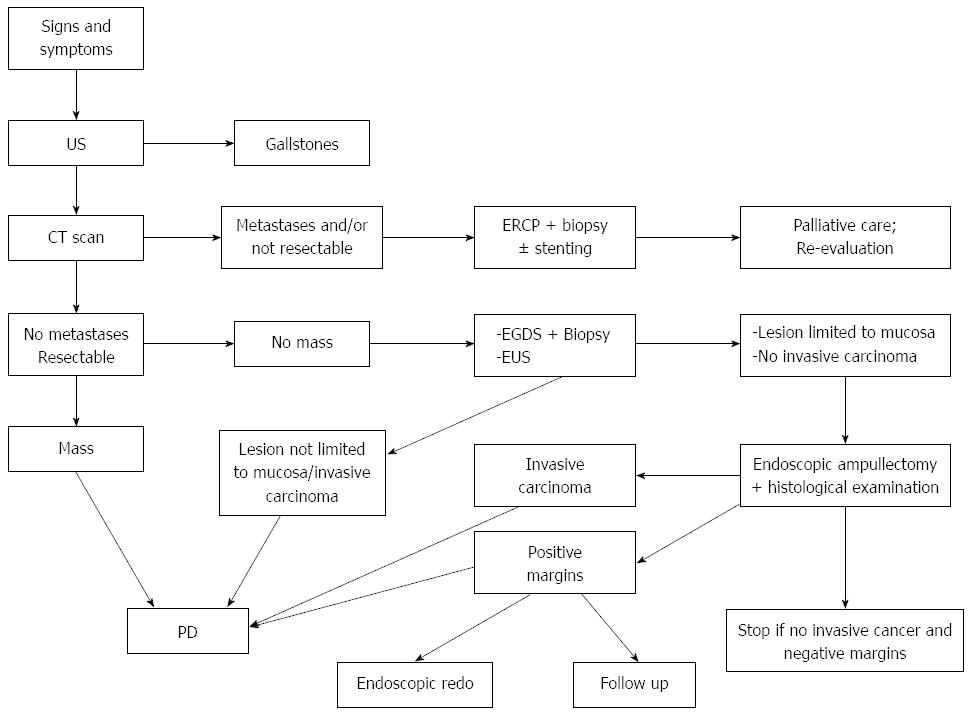
Figure 3 Diagnostic and therapeutic algorithm for suspected papillary lesions.
Once alternative diagnoses have been excluded by ultrasound (US), computerized tomography scan is typically performed in order to assess the stage of the lesion, in particular the presence of metastases and resectability. After diagnostic work-up, if the lesion appears as an infiltrating neoplasia or has a significant mass, then a pancreaticoduonectomy (PD) should be performed. If the lesion is small, then an EGDS with biopsies and endoscopic ultrasound (EUS) staging must be performed. If (1) biopsies exclude the presence of an infiltrating neoplasm; (2) an aggressive histotype and (3) EUS shows that the lesion is confined within the mucosa, endoscopic ampullectomy is the appropriate therapeutic option. If the subsequent histological exam shows the presence of infiltrating cancer, then the intervention should be converted to a PD. If histology shows no evidence of infiltrating cancer but the resection margins are positive, various options are available, including endoscopic redo, close endoscopic follow-up or PD.
- Citation: Panzeri F, Crippa S, Castelli P, Aleotti F, Pucci A, Partelli S, Zamboni G, Falconi M. Management of ampullary neoplasms: A tailored approach between endoscopy and surgery. World J Gastroenterol 2015; 21(26): 7970-7987
- URL: https://www.wjgnet.com/1007-9327/full/v21/i26/7970.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i26.7970