Copyright
©The Author(s) 2015.
World J Gastroenterol. Jun 7, 2015; 21(21): 6759-6763
Published online Jun 7, 2015. doi: 10.3748/wjg.v21.i21.6759
Published online Jun 7, 2015. doi: 10.3748/wjg.v21.i21.6759
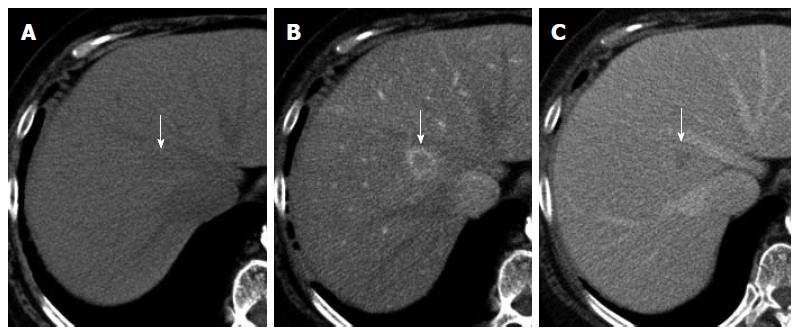
Figure 1 Unenhanced and double-phase contrast-enhanced computed tomography images of the liver, showing a nodule in Segment 1 (arrows).
The nodule shows subtle low attenuation relative to that of liver parenchyma on the unenhanced image (A). On contrast-enhanced computed tomography, the nodule shows perinodular enhancement in the arterial dominant phase (B) and washout of contrast medium in the equilibrium phase (C).
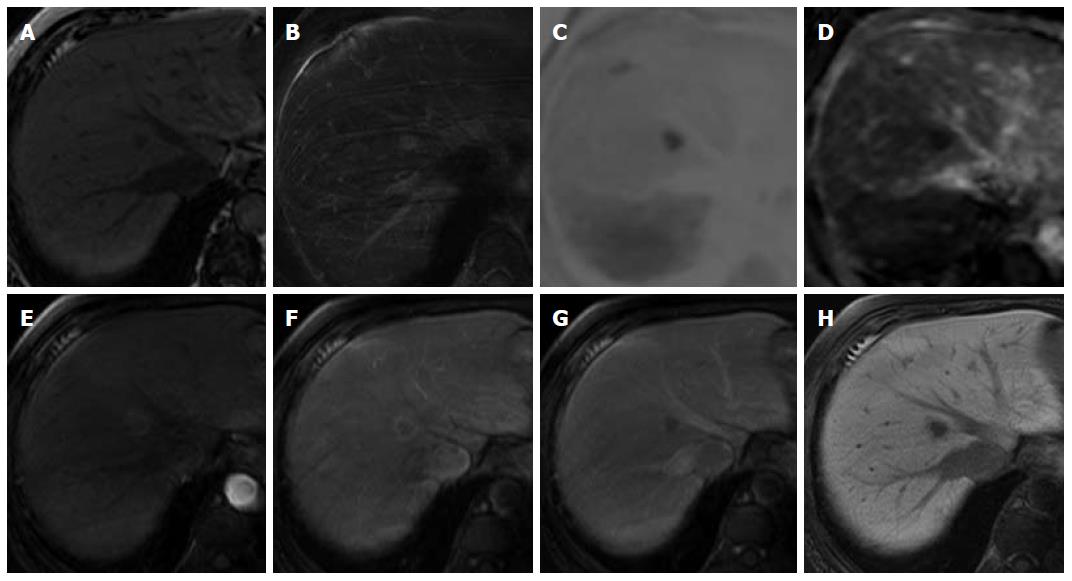
Figure 2 Unenhanced and Gd-EOB-DTPA-enhanced magnetic resonance imaging.
The nodule shows low signal intensity on an unenhanced T1-weighted image (A), and high signal intensity on a T2-weighted image (B). The nodule shows high signal intensity on diffusion-weighted imaging (C) (b = 800 m2/s, inverted black-and-white gray scale), and low signal intensity on apparent diffusion coefficient imaging (D); On Gd-EOB-DTPA-enhanced MRI, the nodule showed perinodular enhancement in the arterial dominant phase (E, F), washout of contrast medium in the late phase (G), and low signal intensity in the hepatobiliary phase (H) suggesting the absence of normal hepatocytes.
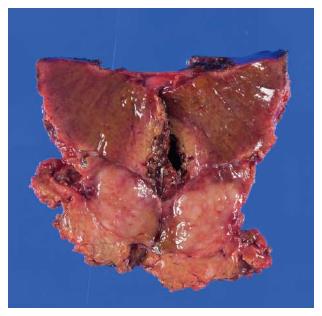
Figure 3 Cut section of the resected liver.
The lesion (15 mm × 10 mm) is well-circumscribed, yellow-white in color, and unencapsulated.
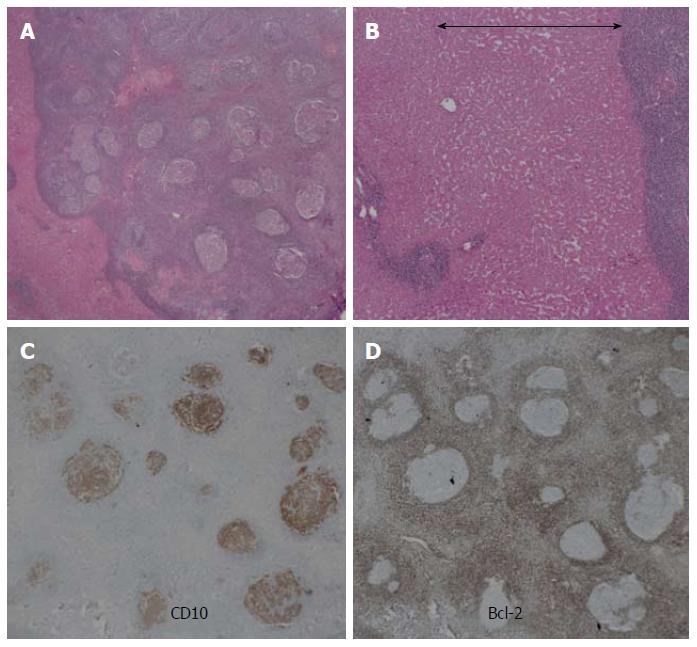
Figure 4 Histological findings.
A: The nodule is well demarcated and comprises a massive infiltration of mature lymphoid cells, forming lymphoid follicles of various sizes with germinal centers (HE staining, low magnification); B: Prominent sinusoidal dilatation (double-headed arrow) seen around the nodule (HE staining, high magnification) is the likely cause of the perinodular enhancement observed on the contrast-enhanced imaging examinations; C, D: Immunohistochemical staining is positive for CD10, and is negative for Bcl-2. These results exclude follicular lymphoma. HE: Hematoxylin and eosin.
- Citation: Sonomura T, Anami S, Takeuchi T, Nakai M, Sahara S, Tanihata H, Sakamoto K, Sato M. Reactive lymphoid hyperplasia of the liver: Perinodular enhancement on contrast-enhanced computed tomography and magnetic resonance imaging. World J Gastroenterol 2015; 21(21): 6759-6763
- URL: https://www.wjgnet.com/1007-9327/full/v21/i21/6759.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i21.6759