Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. Dec 7, 2014; 20(45): 16984-16995
Published online Dec 7, 2014. doi: 10.3748/wjg.v20.i45.16984
Published online Dec 7, 2014. doi: 10.3748/wjg.v20.i45.16984
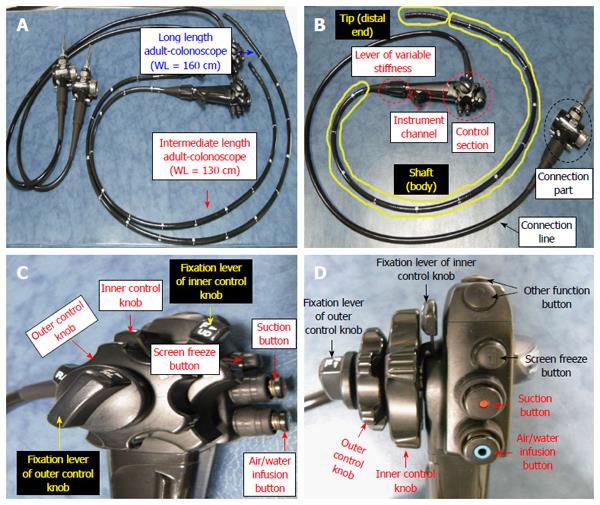
Figure 1 Comparison between normal-type colonoscope and long-type colonoscope (A), components of a colonoscope (B), control section; lateral and forward view (C, D).
WL: Working length.
Figure 2 Posture of examinee and examiner (endoscopist).
A: Left lateral decubitus position of the examinee; B: Two-man method; C: One-man standing method; D: One-man sitting method.
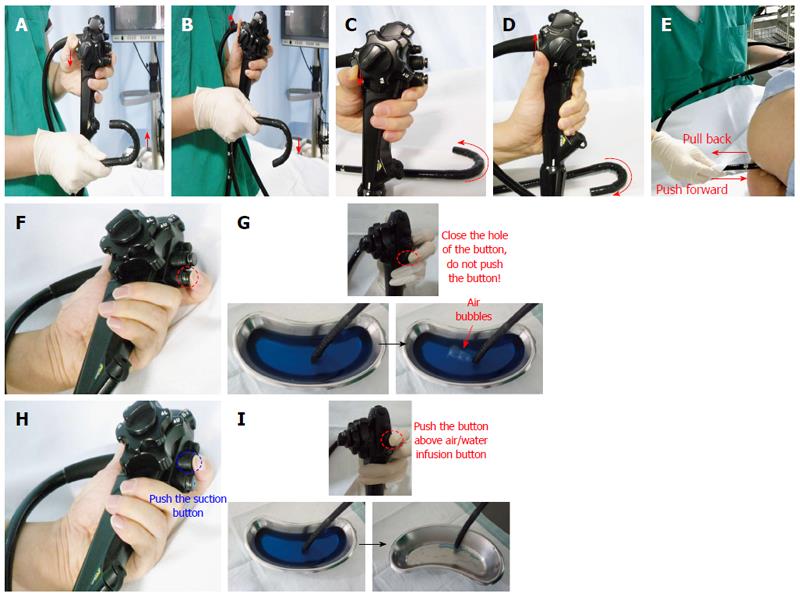
Figure 3 Basic techniques.
A: Up deflection; B: Down deflection; C: Left deflection; D: Right deflection; E: Push forward and pull back; F: Air insufflation (simple closure of hole in the air/water infusion button; pushing button not required); G: Example of air insufflation; H: Air suction (pushing the button above air/water infusion button); I: Example of water suction (because air is invisible).
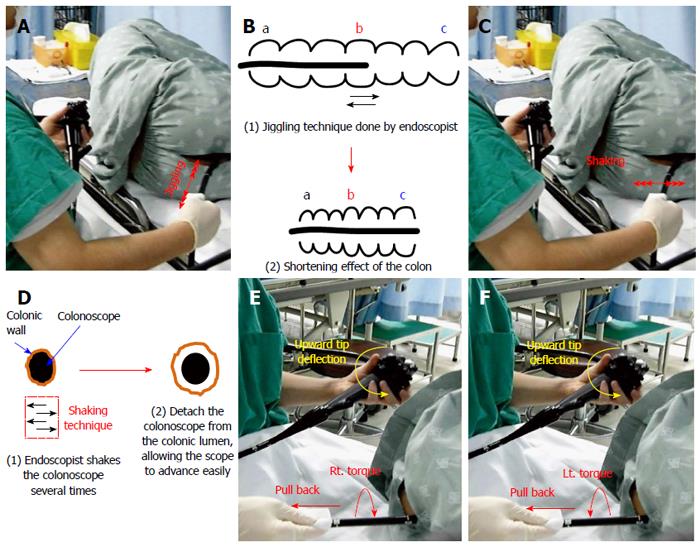
Figure 4 Advanced techniques.
A: Jiggling; B: Effect of jiggling; C: Shaking; D: Effect of shaking; E: Right turn shortening; F: Left turn shortening.
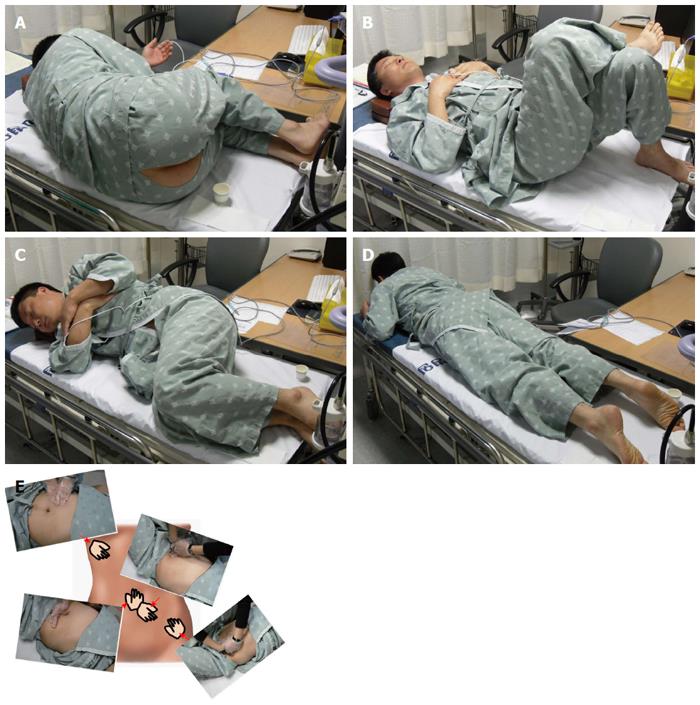
Figure 5 Auxiliary techniques.
A: Left lateral decubitus position; B: Supine position change; C: Right lateral decubitus position change; D: Prone position change; E: Abdominal compression. Left upper corner: Hepatic flexure compression; Right upper corner: Sigmoid colon compression; Left lower corner: Transverse colon compression; Right lower corner: Sigmoidodescending junction compression.
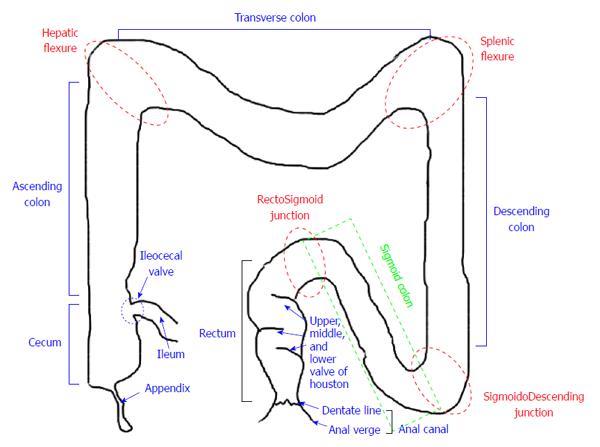
Figure 6 Schematogram of large intestine.
Red dotted circles (rectosigmoid junction, sigmoidodescending junction, splenic flexure, hepatic flexure) and green dotted box (sigmoid colon) are potential difficult segments during the procedure.
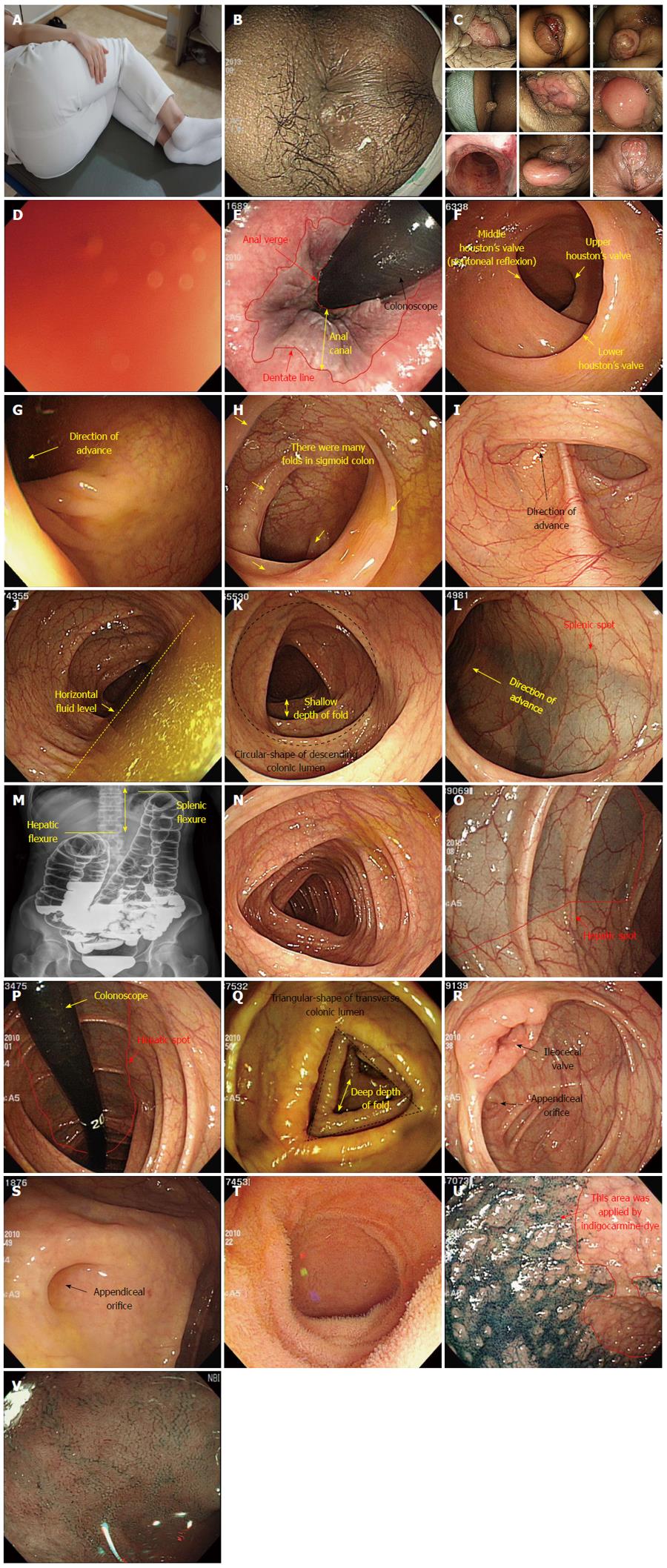
Figure 7 Procedure description.
A: For example, detailed left lateral decubitus position (the examinee with knees bent and pulled up); B: Perianal lesion; C: Various anal lesions; D: Red-out sign; E: Anal canal and distal rectum (Retroflexion view); F: rectum; G: Rectosigmoid junction; H: Sigmoid colon; I: Sigmoidodescending junction; J: Descending colon with horizontal fluid; K: Descending colon (fluid-removal view); L: Splenic flexure and spot; M: Comparison of splenic and hepatic flexures (barium study view); N: Transverse colon; O: Hepatic flexure and spot; P: Hepatic flexure and spot (retroflexion view); Q: Ascending colon; R: Cecum and ileocecal valve; S: Cecal base and appendix orifice; T, U, V: Terminal ileum (water filling view, indigocarmine-dye view, narrow-band imaging view, respectively).
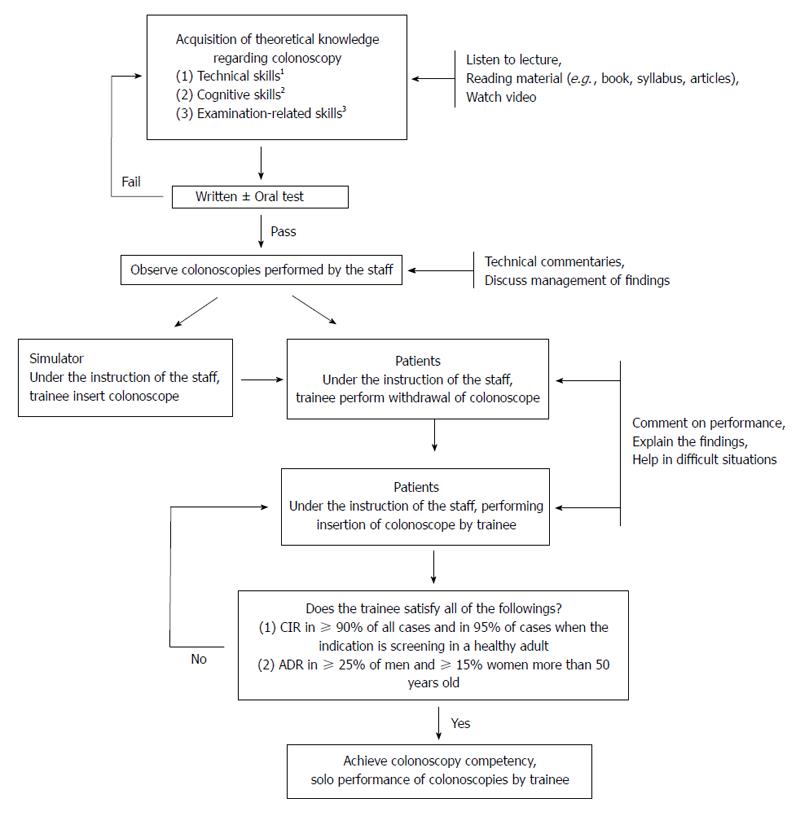
Figure 8 Suggested algorithm for structured learning and training of colonoscopy in new beginners.
1Technical skills include methods for handling the colonoscope and resolving the loops, the ability to perform the colonoscopic examination adequately and in a reasonable amount of time; 2Cognitive skills include the indications and contraindications of the colonoscopic examination, the identification and classification of lesions, clinical decision-making based on findings, and adequate reporting of the colonoscopy; 3Examination-related skills include risk assessment of the patient and the safe method of administration of sedatives and/or analgesics. CIR: Cecal intubation rate; ADR: Adenoma detection rate.
- Citation: Lee SH, Park YK, Lee DJ, Kim KM. Colonoscopy procedural skills and training for new beginners. World J Gastroenterol 2014; 20(45): 16984-16995
- URL: https://www.wjgnet.com/1007-9327/full/v20/i45/16984.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i45.16984