Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. Oct 21, 2014; 20(39): 14156-14171
Published online Oct 21, 2014. doi: 10.3748/wjg.v20.i39.14156
Published online Oct 21, 2014. doi: 10.3748/wjg.v20.i39.14156
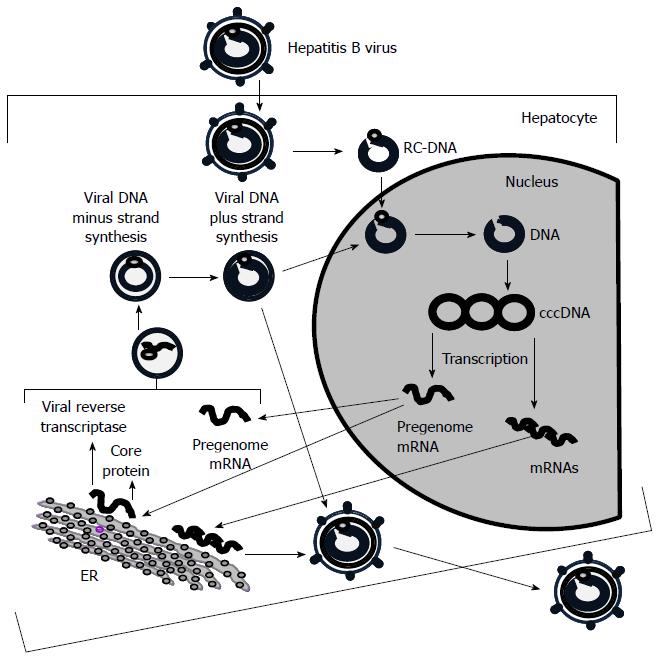
Figure 1 Hepatitis B virus DNA replication.
Hepatitis B virus (HBV) penetration inside a hepatocyte occurs via interaction of envelope proteins with the cell receptors. Viral DNA release from the nucleocapsid with the help of the cellular enzymes takes place in the cytoplasm. After that the viral DNA gets into the nucleus and forms a circular structure-covalently closed circular DNA (cccDNA) which by transcription contributes to the formation of pregenomic RNA and three more mRNAs. Pregenomic RNA leaves the nucleus, gets into endoplasmic reticulum (ER) and serves as a template for synthesis of the core protein and the viral reverse transcriptase. The newly synthesized proteins in combination with free molecules of pregenomic RNA form the nucleocapsid. In the nucleocapsid with help of the reverse transcriptase and the pregenomic RNA as template, the minus strand is synthesized, which later serves as a template for the formation of the plus strand. The formed virus nucleocapsid can either take part in amplication of the viral genome or reach the ER and associate with precore protein and envelope proteins coded by other (non-pregenomic) mRNAs to form a mature virion, then leave the hepatocyte.
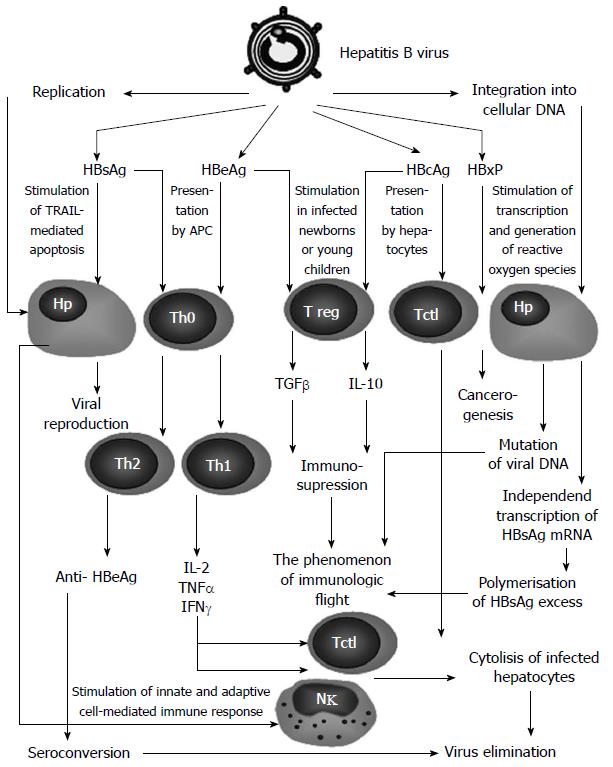
Figure 2 Structural model of hepatitis B virus protein interaction with host cells.
In the course of viral replication or in integration of viral DNA into that of hepatocytes, viral proteins are synthesized in excess. These proteins presented by hepatocytes, or released when the hepatocytes undergo apoptosis, may have a regulating impact on both hepatocytes and the immune system. Hepatitis B surface antigen (HBsAg) synthesized excessively by infected hepatocytes circulates in blood and is presented by dendritic cells, inducing T-helpers mainly of the T-helper (Th)2-type[35]. Anti-HBsAg anti-bodies help to eliminate the virus, while HBsAg itself stimulates the TRAIL-mediated apoptosis of affected hepatocytes[30]. At the same time, the excessive HBsAg is produced when viral DNA integrates into the cell genome and interferes with the formation of anti-bodies (the virus immunologic flight)[25]. Hepatitis B virus core antigen (HBcAg) is presented by hepatocytes to the cytotoxic T-cells (Tctl) that induces cytolysis of the infected hepatocytes[36]. The stimulation of Tctl also may occur indirectly, with participation of Thl cytokines [interleukin (IL)-2, Interferon (IFN)-γ, tumor necrosis factor (TNF)-α] induced by hepatitis B e antigen (HBeAg)[37]. In HBV-infected newborns or young children, HBcAg, often in combination with HBeAg, effectively stimulates regulatory T cells (Tregs) via cytokines [transforming growth factor (ТGF)-β, IL-10], suppress the immune response, facilitating virus immunologic flight[38] that is also contributed by frequent mutations of HBV when it integrates its DNA into the genome of a hepatocyte[39].
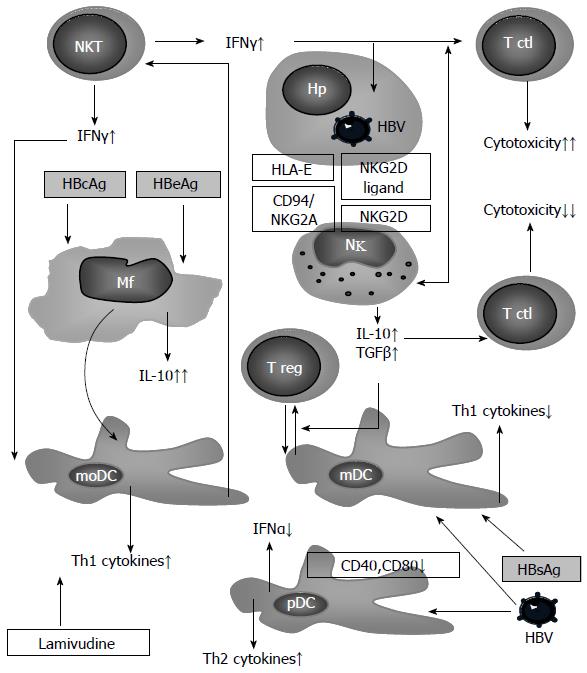
Figure 3 Intracellular interactions in the innate immune system in chronic hepatitis B patients.
An infected hepatocyte (Hp) expresses ligands for inhibiting (CD94/NKG2A) and activating (NKG2D) receptors of natural killer (NK) cells, which stimulate these cells to secrete immunosuppressive cytokines (IL-10 and TGFβ), assisting in the induction of regulatory T cells (Tregs) with the participation of mDC[98]. Under the influence of viral antigens, pDC decreases its adhesive properties as well as its abilities to produce interferon (IFN)-α[35,107,108], thus creating ideal conditions for the involvement of Th2 in the immune response. Simultaneously, there is monocyte stimulation to produce immunosuppressive IL-10. Viral antigens also contribute to the differentiation of monocytes to the dendritic cells[41]. Monocytic dendritic cells (moDC) induce Th1 defects that are characteristic of chronic hepatitis C patients[109], and that may be corrected by treatment with lamivudine[87]. NKTs, actively producing IFNγ in chronic hepatitis B (CHB)[102], assist in the increase of efficacy of cell-mediated immune response with participation of Th1 and cytotoxic T cells (CTL)[110].
- Citation: Balmasova IP, Yushchuk ND, Mynbaev OA, Alla NR, Malova ES, Shi Z, Gao CL. Immunopathogenesis of chronic hepatitis B. World J Gastroenterol 2014; 20(39): 14156-14171
- URL: https://www.wjgnet.com/1007-9327/full/v20/i39/14156.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i39.14156