Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. Oct 21, 2014; 20(39): 14156-14171
Published online Oct 21, 2014. doi: 10.3748/wjg.v20.i39.14156
Published online Oct 21, 2014. doi: 10.3748/wjg.v20.i39.14156
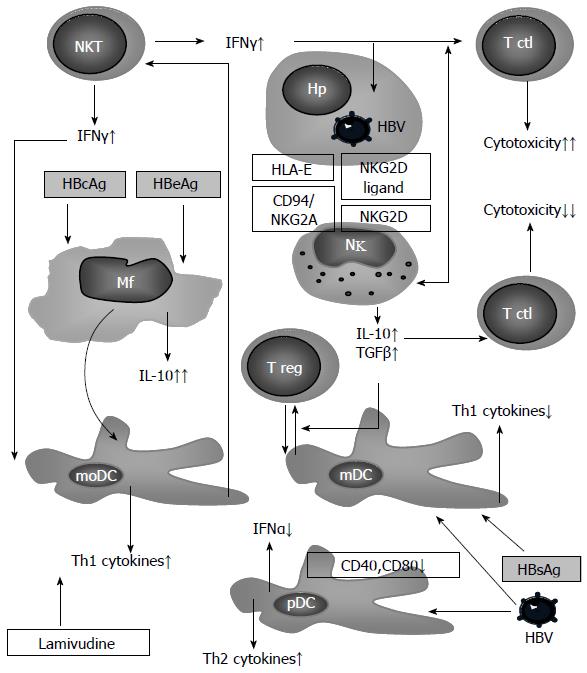
Figure 3 Intracellular interactions in the innate immune system in chronic hepatitis B patients.
An infected hepatocyte (Hp) expresses ligands for inhibiting (CD94/NKG2A) and activating (NKG2D) receptors of natural killer (NK) cells, which stimulate these cells to secrete immunosuppressive cytokines (IL-10 and TGFβ), assisting in the induction of regulatory T cells (Tregs) with the participation of mDC[98]. Under the influence of viral antigens, pDC decreases its adhesive properties as well as its abilities to produce interferon (IFN)-α[35,107,108], thus creating ideal conditions for the involvement of Th2 in the immune response. Simultaneously, there is monocyte stimulation to produce immunosuppressive IL-10. Viral antigens also contribute to the differentiation of monocytes to the dendritic cells[41]. Monocytic dendritic cells (moDC) induce Th1 defects that are characteristic of chronic hepatitis C patients[109], and that may be corrected by treatment with lamivudine[87]. NKTs, actively producing IFNγ in chronic hepatitis B (CHB)[102], assist in the increase of efficacy of cell-mediated immune response with participation of Th1 and cytotoxic T cells (CTL)[110].
- Citation: Balmasova IP, Yushchuk ND, Mynbaev OA, Alla NR, Malova ES, Shi Z, Gao CL. Immunopathogenesis of chronic hepatitis B. World J Gastroenterol 2014; 20(39): 14156-14171
- URL: https://www.wjgnet.com/1007-9327/full/v20/i39/14156.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i39.14156