Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. Oct 21, 2014; 20(39): 14156-14171
Published online Oct 21, 2014. doi: 10.3748/wjg.v20.i39.14156
Published online Oct 21, 2014. doi: 10.3748/wjg.v20.i39.14156
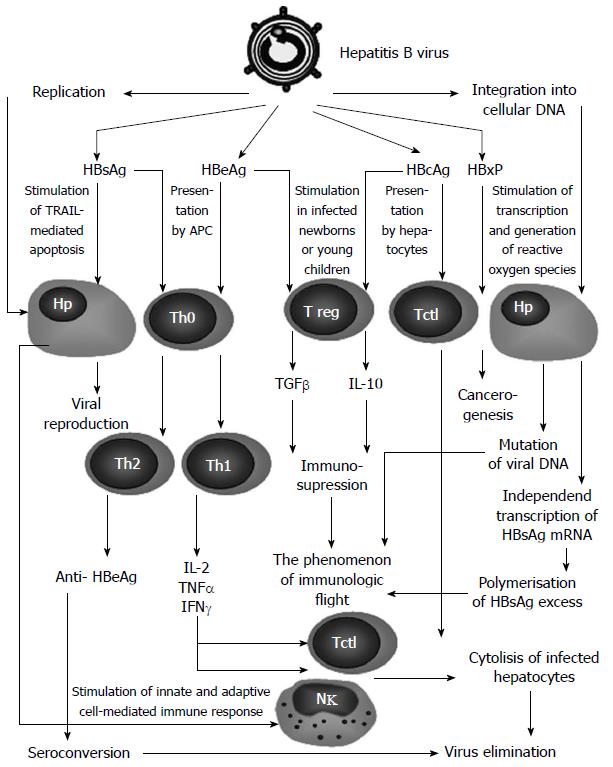
Figure 2 Structural model of hepatitis B virus protein interaction with host cells.
In the course of viral replication or in integration of viral DNA into that of hepatocytes, viral proteins are synthesized in excess. These proteins presented by hepatocytes, or released when the hepatocytes undergo apoptosis, may have a regulating impact on both hepatocytes and the immune system. Hepatitis B surface antigen (HBsAg) synthesized excessively by infected hepatocytes circulates in blood and is presented by dendritic cells, inducing T-helpers mainly of the T-helper (Th)2-type[35]. Anti-HBsAg anti-bodies help to eliminate the virus, while HBsAg itself stimulates the TRAIL-mediated apoptosis of affected hepatocytes[30]. At the same time, the excessive HBsAg is produced when viral DNA integrates into the cell genome and interferes with the formation of anti-bodies (the virus immunologic flight)[25]. Hepatitis B virus core antigen (HBcAg) is presented by hepatocytes to the cytotoxic T-cells (Tctl) that induces cytolysis of the infected hepatocytes[36]. The stimulation of Tctl also may occur indirectly, with participation of Thl cytokines [interleukin (IL)-2, Interferon (IFN)-γ, tumor necrosis factor (TNF)-α] induced by hepatitis B e antigen (HBeAg)[37]. In HBV-infected newborns or young children, HBcAg, often in combination with HBeAg, effectively stimulates regulatory T cells (Tregs) via cytokines [transforming growth factor (ТGF)-β, IL-10], suppress the immune response, facilitating virus immunologic flight[38] that is also contributed by frequent mutations of HBV when it integrates its DNA into the genome of a hepatocyte[39].
- Citation: Balmasova IP, Yushchuk ND, Mynbaev OA, Alla NR, Malova ES, Shi Z, Gao CL. Immunopathogenesis of chronic hepatitis B. World J Gastroenterol 2014; 20(39): 14156-14171
- URL: https://www.wjgnet.com/1007-9327/full/v20/i39/14156.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i39.14156