Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. Aug 7, 2014; 20(29): 9699-9715
Published online Aug 7, 2014. doi: 10.3748/wjg.v20.i29.9699
Published online Aug 7, 2014. doi: 10.3748/wjg.v20.i29.9699
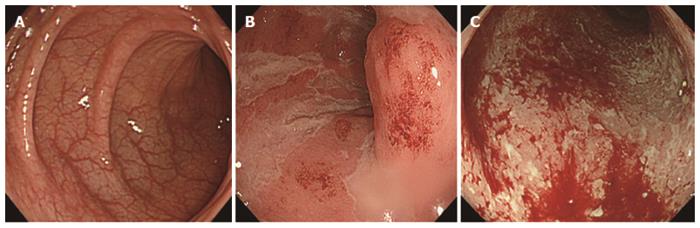
Figure 1 Colonoscopy images.
A: Colonoscopy showing normal mucosa with visible vascular patterns in a healthy, non-inflammatory bowel disease (IBD) individual; B: During strong inflammation in a patient with IBD, visible vascular patterns are lost; C: Inflammation can lead to ulcerated mucosa and contact bleeding. Both mucosal inflammation and ulcers lead to inadequate absorption of water and nutrients from the gut. The affected patients may lose weight and become anaemic due to bloody diarrhoea, which if untreated can be very debilitating.
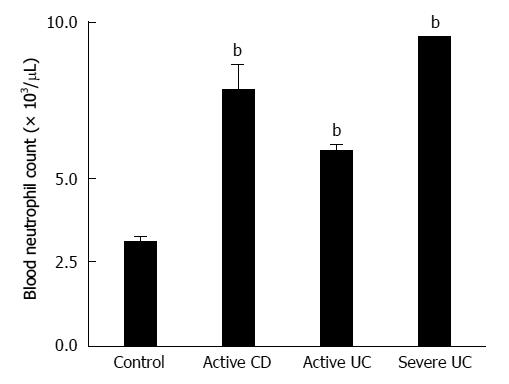
Figure 2 Blood neutrophil (granulocyte) counts in healthy controls and patients with inflammatory bowel disease.
This figure shows a very marked elevation of neutrophils during active inflammatory bowel disease (IBD). Additionally, in patients with IBD, neutrophils show activation behaviour and increased survival time in the circulation[26,36] as well as within the mucosal tissue[25]. bP < 0.01 vs control group. UC: Ulcerative colitis; CD: Crohn’s disease.
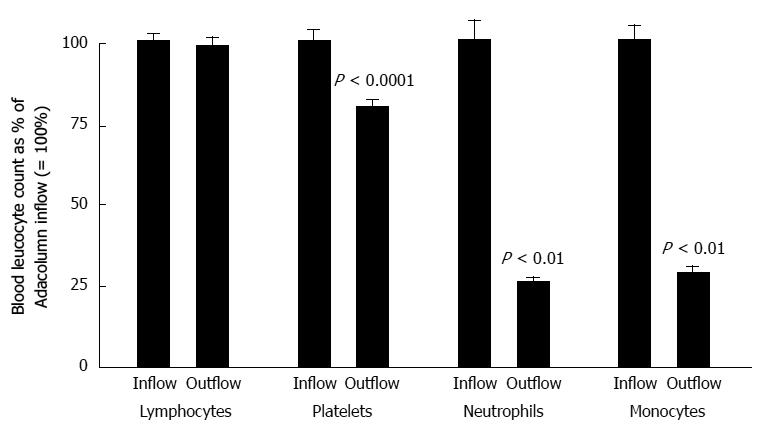
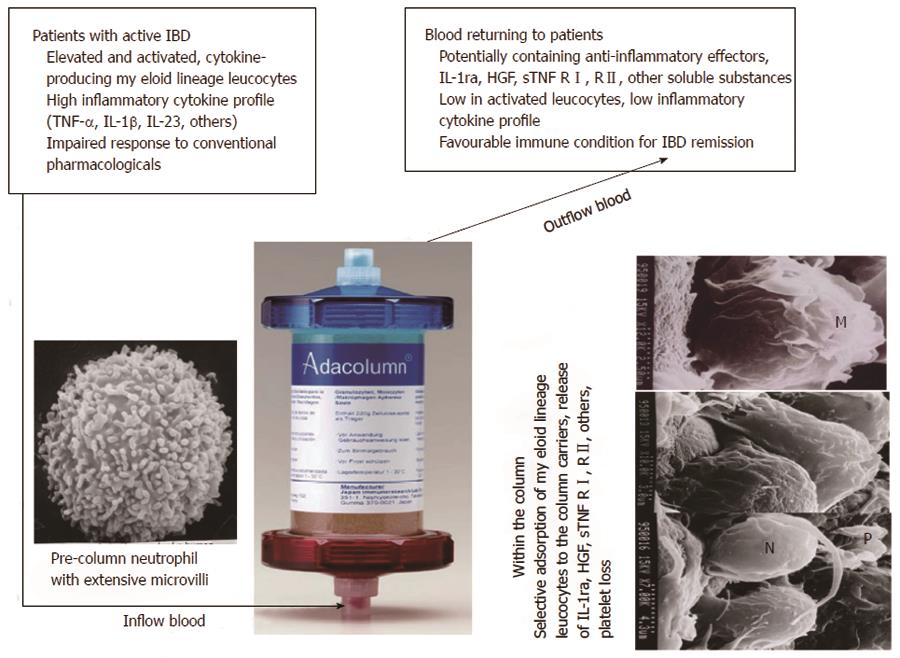
Figure 3 Selective depletion of myeloid lineage cells (neutrophils, monocytes and platelets) by adsorptive granulocyte and monocyte apheresis with the Adacolumn in patients with inflammatory bowel disease.
In each case, the column inflow count was expressed as 100% and the column outflow count (return to patient) was expressed as a percentage of the inflow count taken 30 min (peak fall) during a 60-min granulocyte and monocyte apheresis (GMA) session. The data serve as a solid basis for the argument that GMA selectively depletes granulocytes, monocytes/macrophages together with a significant fraction of platelets, but spares lymphocytes[22,23,48,117].
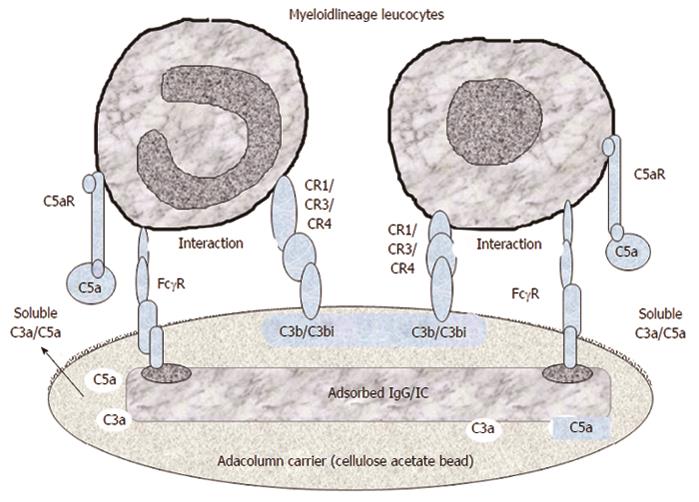
Figure 4 A tentative illustration of the mechanisms, which mediate the selective adhesion of myeloid lineage leucocytes to the granulocyte and monocyte apheresis cellulose acetate carriers.
The first event is adhesion of plasma immunoglobulin (IgG) and immune complexes (IC) to the carriers, which serve as the binding sites for the fragment crystallizable gamma receptor (FcγR) on myeloid leucocytes. Then complement activation (helped by IgG and IC) generates C3a, C5a, C3b/C3bi fragments. Of these C3b/C3bi (opsonins) adsorb onto the carriers and serve as the binding sites for the complement receptors (CR) on myeloid leucocytes. Adhesion of leucocytes results in the release of interleukin-1 receptor antagonis, hepatocyte growth factor, soluble tumour necrosis factor receptors, all with therapeutic effects (Figure 13). Modified from Reference[23].
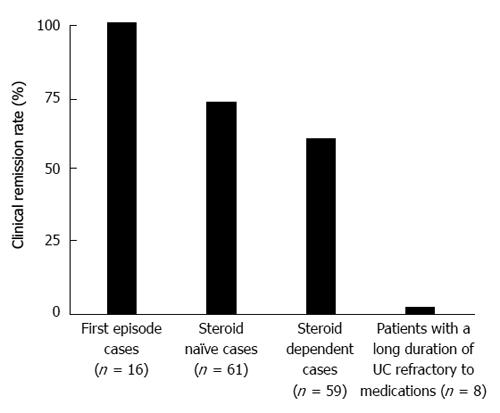
Figure 5 Clinical remission rates in typical cohorts of patients with active ulcerative colitis.
The remission rate for patients with the first ulcerative colitis (UC) episode was 100%. All these first episode cases were steroid naïve with a short (< 4 mo) duration of UC; both steroid naïve and short disease duration are granulocyte and monocyte apheresis (GMA)-responder features. Accordingly, the remission rate in corticosteroid naïve cohort looks better than for steroid dependent cohort. GMA non-responder patients had deep ulcers with near total loss of the mucosal tissue at the lesion sites, a long duration of UC, and exposure to multiple drugs; a few were candidates for colectomy[42,49,52].
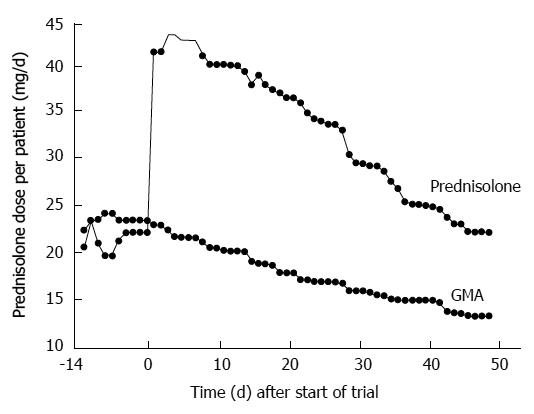
Figure 6 Steroid sparing effect of granulocyte and monocyte apheresis.
In this trial, 105 patients with active ulcerative colitis while on the corticosteroid prednisolone (PSL) were randomly assigned to granulocyte and monocyte apheresis (GMA) (n = 53) or to PSL (n = 52). In the PSL group, the steroid dose was increased at entry to induce remission, while patients in the GMA group received GMA, at one session per week over five consecutive weeks. PSL dose was then tapered in line with disease improvement or remission. At the end of the trial, 21 patients (44.2%) in the PSL group and 31 patients (58.5%) in the GMA group were in remission. Therefore, GMA showed significantly better efficacy than PSL and spared patients from steroids[22,41,44].
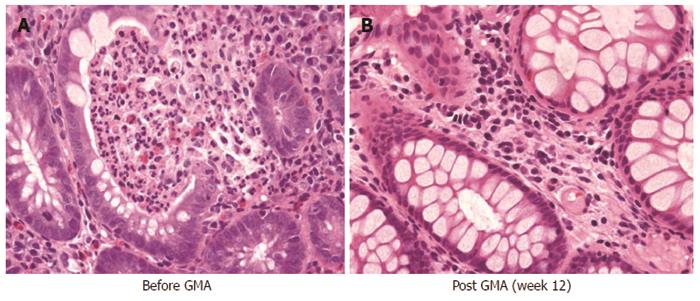
Figure 7 Typical immunohistochemical images taken from colonic biopsy specimens in a patient with total colitis in active stage (A) and following remission (B).
This figure shows that the mucosal tissue is densely infiltrated by myeloid lineage leucocytes and granulocyte and monocyte apheresis has reduced the concentration of these leucocytes in the mucosa. The specimens seen in this figure are from a 60-year-old male with moderately severe ulcerative colitis and corticosteroid naive, baseline clinical activity index, 13.
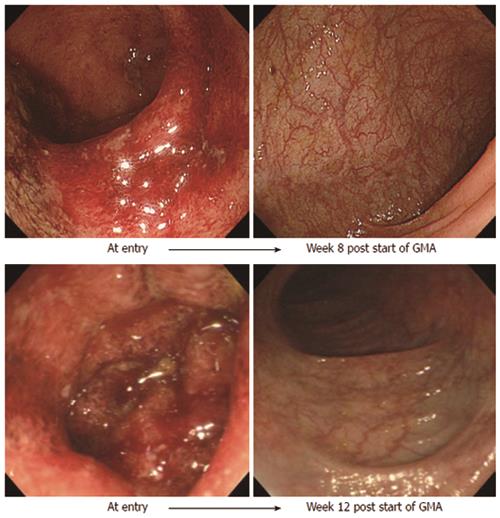
Figure 8 Typical endoscopic features of patients who may respond well to granulocyte and monocyte apheresis and be spared from drug based medications.
These cases were from a subgroup of patients who have been identified as good responders by colonoscopy. These patients were steroid naïve with severe ulcerative colitis (clinical activity indices > 14), yet good responders to granulocyte and monocyte apheresis (GMA), firstly because the mucosal tissue was preserved and secondly, the patients were corticosteroid naïve at the time of relapse. The photographs show complete restoration of the mucosal vascular patterns at post GMA.
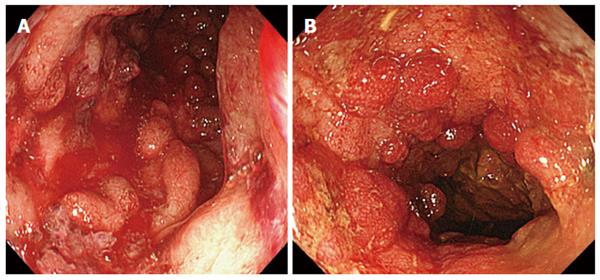
Figure 9 Colonoscopy images showing deep and extensive colonic lesions together with inflammatory polyps and contact bleeding.
Typical colonoscopic images from patients with severely damaged mucosal tissue (A), granulocyte/monocyte apheresis non-responders (B). However, most patients with the entry mucosal damage seen in this figure are medication refractory and unlikely to respond to granulocyte and monocyte apheresis, some opt for colectomy.
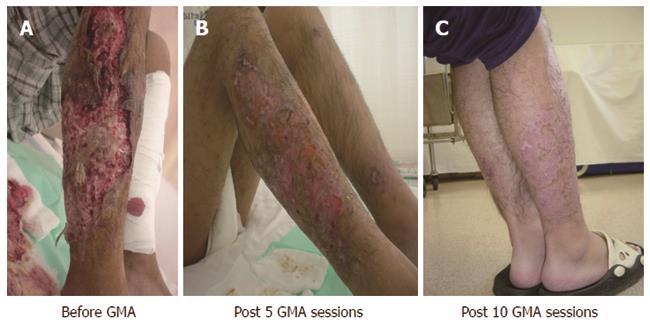
Figure 10 Pyoderma gangrenosum lesions.
Pyoderma gangrenosum lesions associated with Crohn’s disease (A), partially re-epithelialized after 5 granulocyte and monocyte apheresis (GMA), sessions (B), fully re-epithelialized after 10 GMA sessions (C)[103].
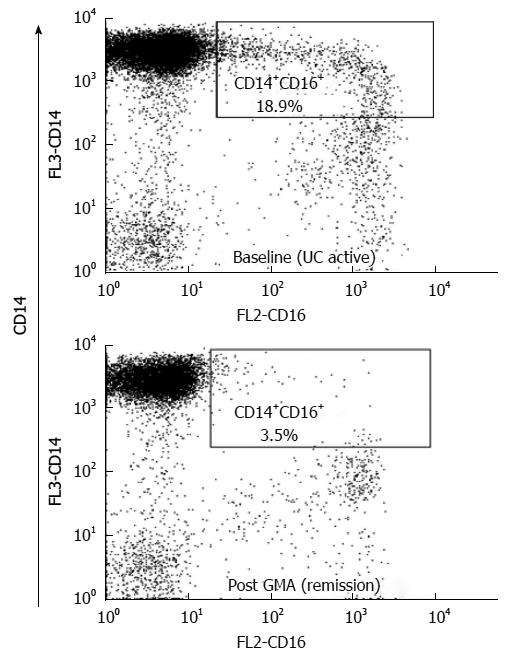
Figure 11 Typical flow cytometry outputs.
Flow cytometry showing immunophenotyping of elevated pro-inflammatory CD14(+)CD16(+)DR(++) monocytes in a patient with inflammatory bowel disease and depletion of these tumour necrosis factor-producing leucocytes by granulocyte and monocyte apheresis (GMA). In this patient, an 18.9% of monocytes were identified as CD14+CD16+ phenotype in active ulcerative colitis (UC) stage and this was reduced to just 3.5% when the patient achieved remission following a course of GMA therapy. Normal level is < 8%[109].
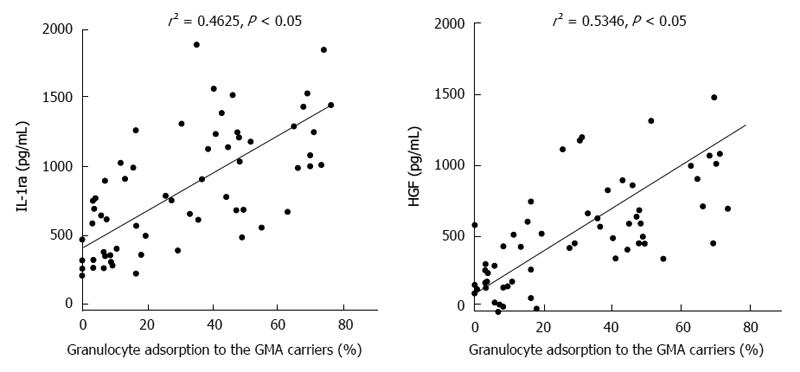
Figure 12 Adsorption dependent release of interleukin-1 receptor antagonist, and hepatocyte growth factor from myeloid lineage leucocytes (granulocytes and monocytes) in in-vitro setting.
Hepatocyte growth factor (HGF) is known to promote ulcer healing and cell regeneration, while interleukin-1 receptor antagonist (IL-1ra) is strongly anti-inflammatory[113]. GMA: Granulocyte and monocyte apheresis.
Figure 13 An idealistic view of the events attributed to therapeutic granulocyte and monocyte apheresis with the Adacolumn in patients with inflammatory bowel disease.
Scanning photomicrographs of leucocytes adsorbed onto a granulocyte and monocyte apheresis (GMA) carrier and the basic events, which follow on the surface of the carriers during GMA in clinical setting (see Figure 4 as well). Normal, non-activated and non-adherent neutrophils and monocytes/macrophages express extensive surface microvilli. The villi bear various receptors like tumour necrosis factor (TNF) receptors, and L selectin, which are shed upon adsorption of the cells to the carriers. Further as seen, adsorbed leucocytes undergo extensive release reaction. Up to now, interleukin-1 receptor antagonist (IL-1ra), hepatocyte growth factor (HGF), IL-10 and soluble TNF receptors have been measured. During GMA, the blood, which returns to patients via the column outflow line may be likened to a biologic cocktail containing a large number of soluble substances released by the adherent leucocytes. The adsorptive nature of GMA is thought to be the most intriguing feature of this non-pharmacological treatment intervention. M: Monocyte; N: Neutrophil; P: Platelet; IBD: Inflammatory bowel disease.
- Citation: Saniabadi AR, Tanaka T, Ohmori T, Sawada K, Yamamoto T, Hanai H. Treating inflammatory bowel disease by adsorptive leucocytapheresis: A desire to treat without drugs. World J Gastroenterol 2014; 20(29): 9699-9715
- URL: https://www.wjgnet.com/1007-9327/full/v20/i29/9699.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i29.9699