Copyright
©2014 Baishideng Publishing Group Co.
World J Gastroenterol. Apr 14, 2014; 20(14): 4110-4114
Published online Apr 14, 2014. doi: 10.3748/wjg.v20.i14.4110
Published online Apr 14, 2014. doi: 10.3748/wjg.v20.i14.4110
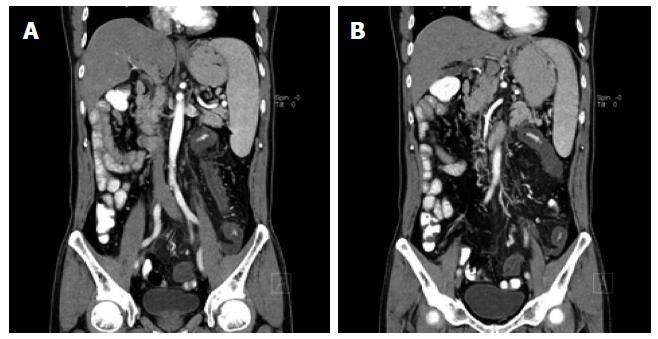
Figure 1 Magnetic resonance imaging of the abdomen and pelvic showed a stenosis of the mesenteric inferior artery branch (A) and thickening of the mesenteric inferior artery branch walls (B).
The image shows a diffuse lesion of the left colon suggesting ischaemic injury.
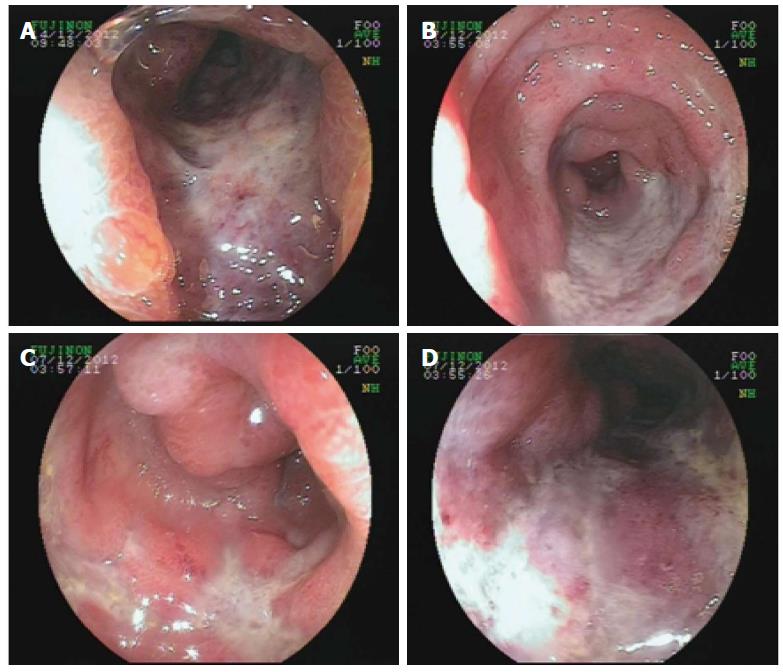
Figure 2 Colonoscopy showed a deep ulcer lesion and granulated tissue of the sigmoid colon and rectum.
Lumenal stenosis is obvious.
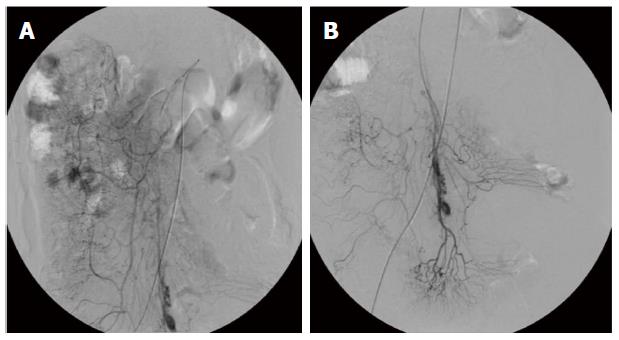
Figure 3 Digital subtraction angiography showed abnormalities in the architecture of the superior mesenteric artery including chaotic distribution (A) and pooling of contrast material (B).
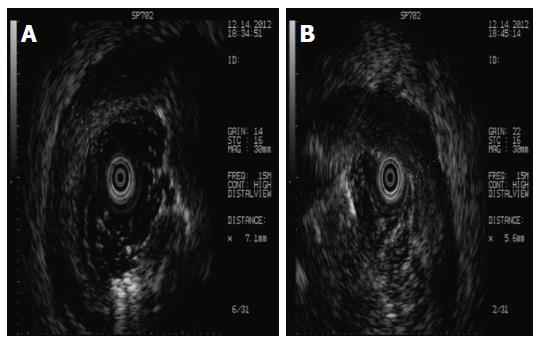
Figure 4 Endoscopic ultrasonography showed ulcers and necrosis in the depth of the mucosa or submucosa (A) and circumscribed mucosal thickening (B).
The image shows a characteristic change of chronic nonspecific inflammation, but not malignant lymphoma.
Figure 5 Sigmoid colon mucosal biopsy revealed chronic nonspecific colitis (A, B: HE stain, 100 ×; C, D: HE stain, 200 ×).
The image shows formation of granulation tissue, lymphoid hyperplasia, and infiltration of plasma cells, neutrophils, and monocytes into the mucosa. Increased blood vessels with hyaline degeneration and thickening vessel wall are seen. Lymphocytes surround the wall of the submucosal venules, especially in the deeper parts.
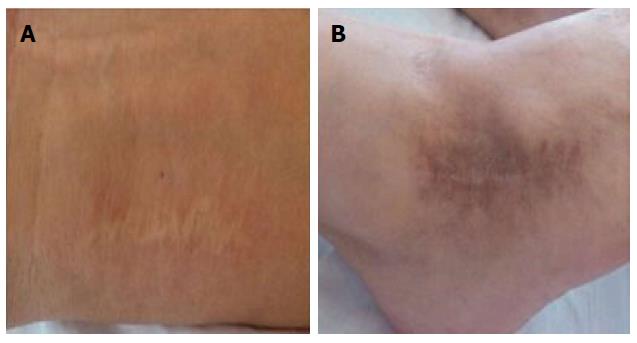
Figure 6 Surgical scar on the left wrist from surgery for tenosynovitis (A) and left ankle cyst (B).
- Citation: Yang XN, Ye ZS, Fan YY, Hu YQ. Prolonged small vessel vasculitis with colon mucosal inflammation as first manifestations of Behçet’s disease. World J Gastroenterol 2014; 20(14): 4110-4114
- URL: https://www.wjgnet.com/1007-9327/full/v20/i14/4110.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i14.4110