Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Dec 14, 2013; 19(46): 8595-8604
Published online Dec 14, 2013. doi: 10.3748/wjg.v19.i46.8595
Published online Dec 14, 2013. doi: 10.3748/wjg.v19.i46.8595
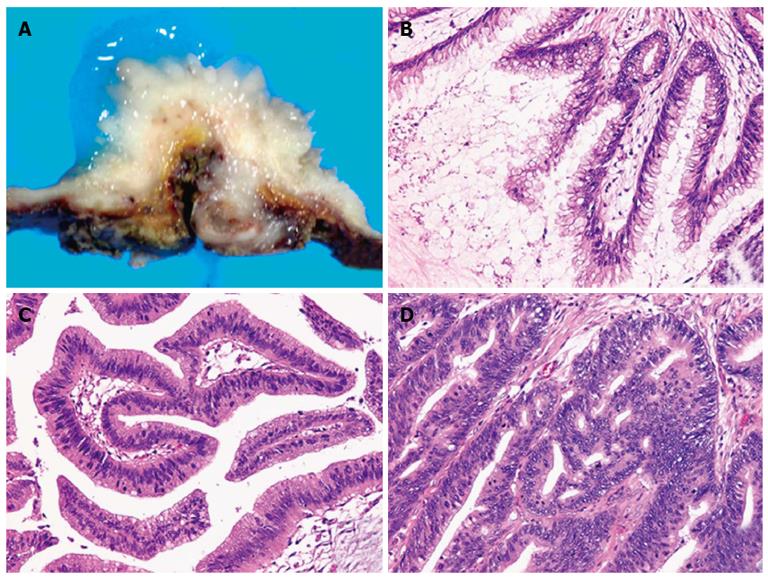
Figure 1 A representative case of intraductal papillary neoplasm of the bile duct with macroscopically visible mucin secretion.
Within a single tumor (A), the coexistence of adenoma (B), borderline lesion (C), and adenocarcinoma (D) was found (hematoxylin and eosin stain, × 200 ).
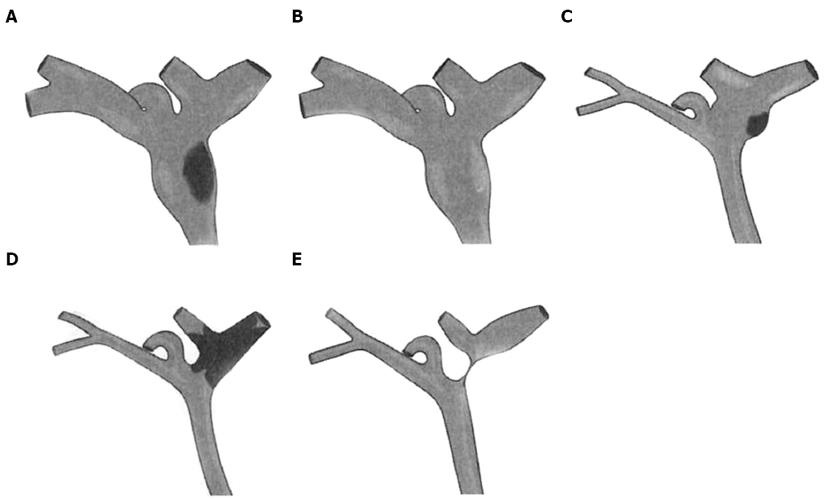
Figure 2 Schematic drawings of intraductal papillary neoplasms of the bile duct showing the five imaging patterns.
A: Type 1: Diffuse duct ectasia with a grossly visible papillary mass; B: Type 2: Diffuse duct ectasia without a visible mass; C: Type 3: An intraductal polypoid mass within localized duct dilation; D: Type 4: Intraductal cast-like lesions; E: Type 5: A focal stricture-like lesion with mild proximal ductal dilation.
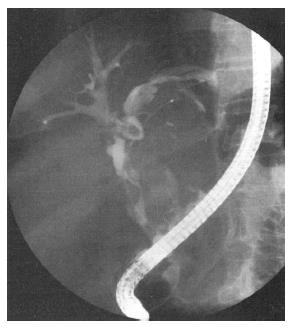
Figure 3 Endoscopic retrograde cholangiography showing an amorphous filling defect, suggesting the presence of mucobilia.
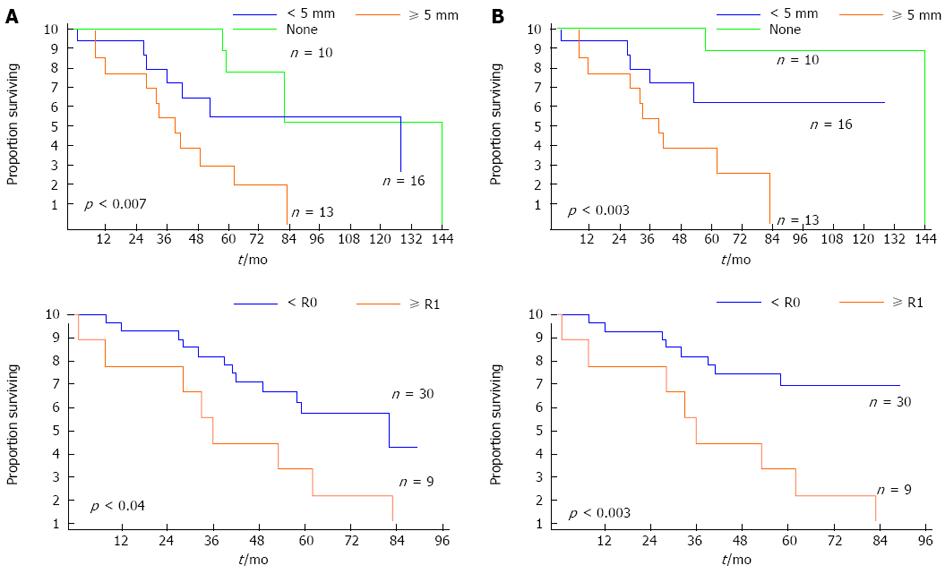
Figure 4 Kaplan-Meier survival estimates of overall survival (A) and disease-specific survival (B) according to the depth of extraductal invasion (none, < 5 mm, and ≥ 5 mm) and resection type (R0 vs R1).
P < 0.05 was considered significant.
- Citation: Wan XS, Xu YY, Qian JY, Yang XB, Wang AQ, He L, Zhao HT, Sang XT. Intraductal papillary neoplasm of the bile duct. World J Gastroenterol 2013; 19(46): 8595-8604
- URL: https://www.wjgnet.com/1007-9327/full/v19/i46/8595.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i46.8595