Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Apr 21, 2013; 19(15): 2319-2330
Published online Apr 21, 2013. doi: 10.3748/wjg.v19.i15.2319
Published online Apr 21, 2013. doi: 10.3748/wjg.v19.i15.2319
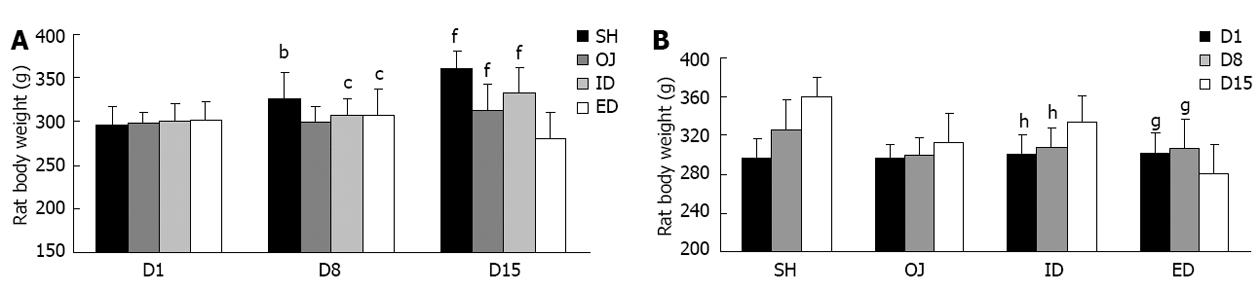
Figure 1 Changes of rat body weight with time following operations among the four groups.
A: Obstructive jaundice (OJ) rats ate markedly less food and there was a slowly increasing trend of body weight between the 1st, 8th and 15th day (P = 0.155). On the contrary, weight gain was more significant in sham operation (SH) rats compared with that in OJ rats on the 8th and 15th day. After relief of OJ, the appetite of internal biliary drainage (ID) rats recovered and the body weight of ID rats on the 15th day became significantly higher than that on the 8th day. bP < 0.01 vs OJ; cP < 0.05 vs SH; fP < 0.01 vs external biliary drainage (ED); B: Weight loss was observed in ED rats and the body weight on day 15 was significantly lower than that on the 1st or 8th day. gP < 0.05, hP < 0.01 vs D15.
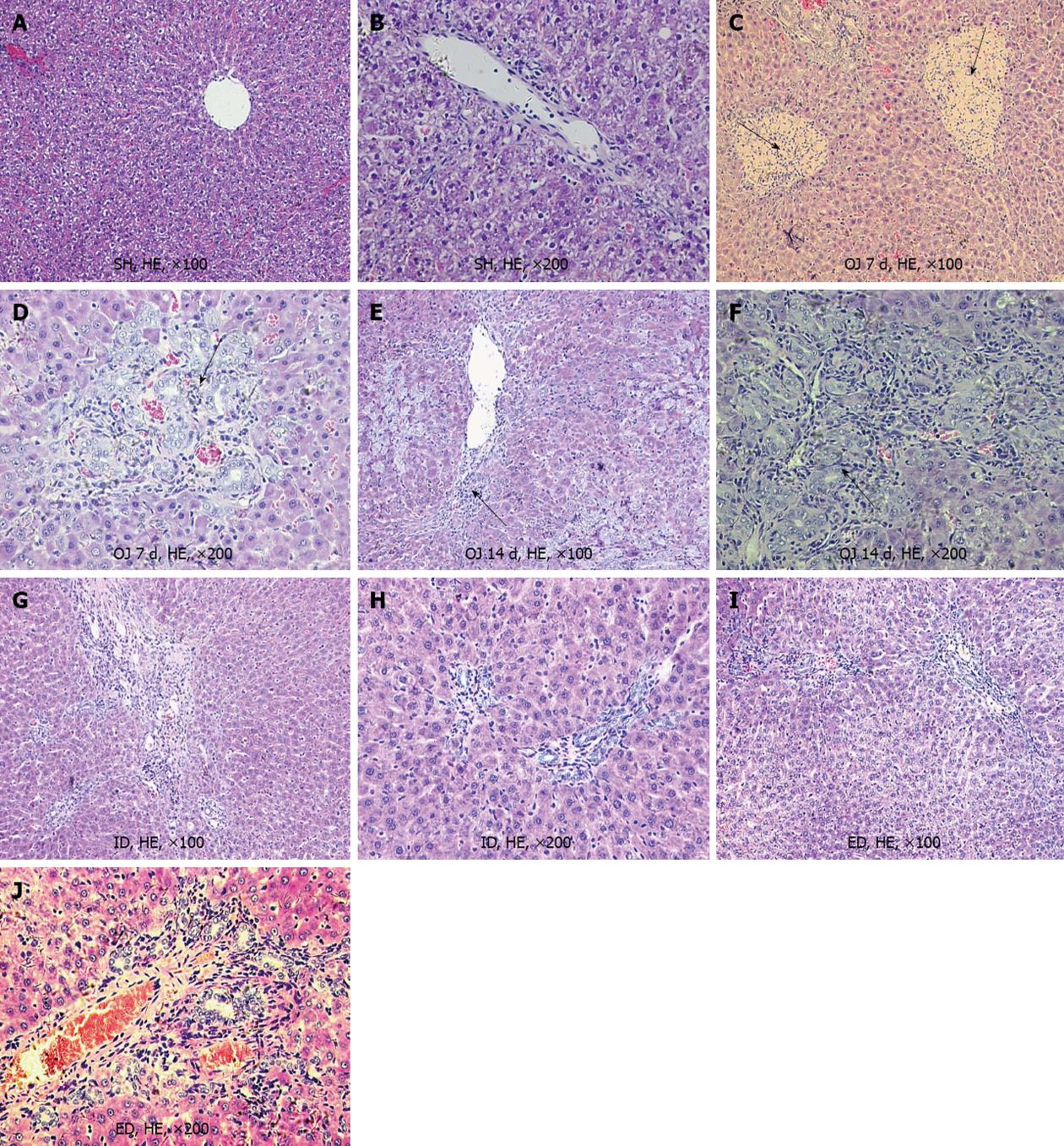
Figure 2 Micrograph of liver sections from rats of sham operation, obstructive jaundice, internal and external biliary drainage groups (the pathological changes were marked by black arrows).
A, B: There was almost no pathological changes in the liver of sham operation (SH) rats, the liver lobular architecture was intact; C, D: After bile duct ligation for 7 d, the liver showed focal necrosis and mild bile duct proliferation with acute inflammatory cell infiltration in the portal and periportal areas, but the lobular architecture was still intact in the cholestatic liver; E, F: After bile duct ligation for 14 d, the liver showed striking liver fibrosis and prominent bile duct proliferation in the portal tracts; G, H: Following 7 d of internal biliary drainage (ID), the liver displayed preserved lobular architecture with only mild bile duct proliferation, and the progression of liver fibrosis and cirrhosis stopped; I, J: After external biliary drainage (ED), lobular architecture was preserved with only mild biliary proliferation, but the degree of liver fibrosis was still at a high level. HE: Hematoxylin and eosin; OJ: Obstructive jaundice.
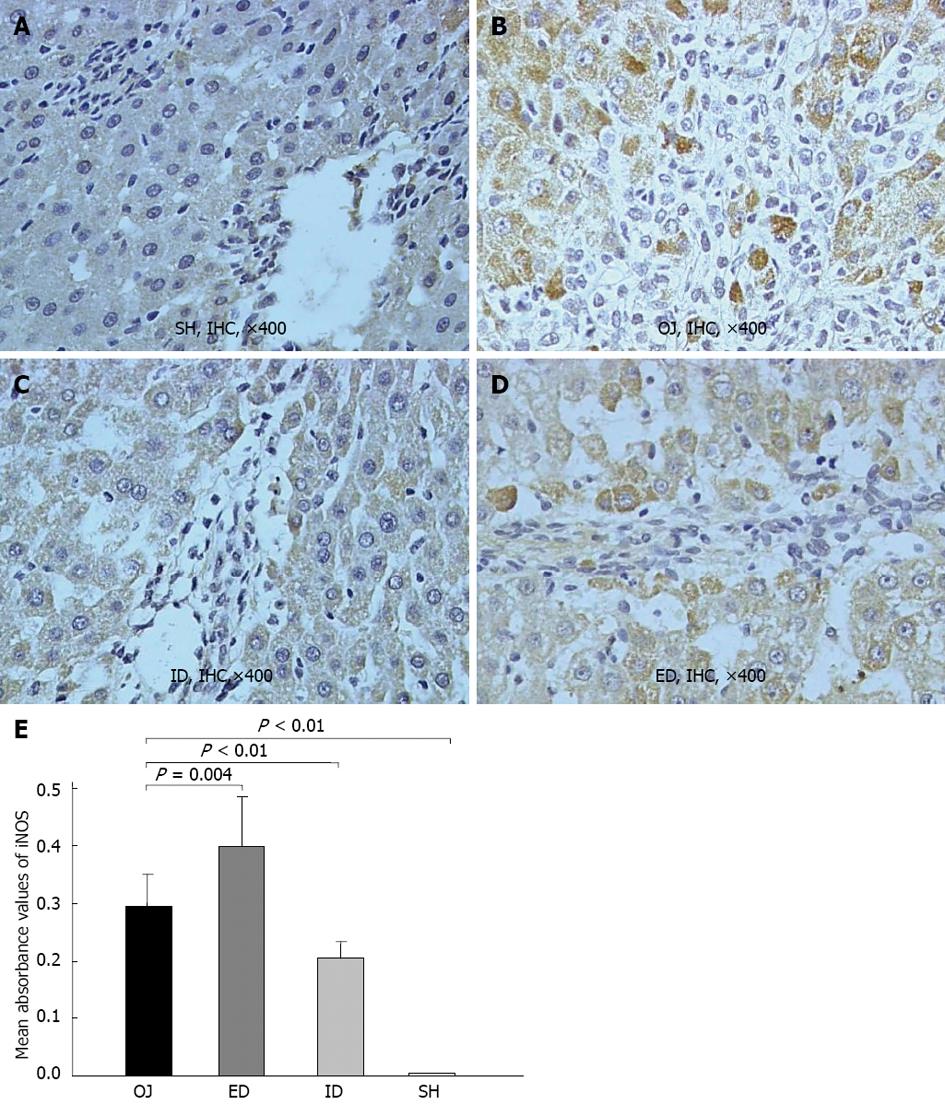
Figure 3 Representative immunohistochemical analysis of inducible nitric oxide synthase in rat liver of sham operation, obstructive jaundice, internal and external biliary drainage groups.
A: There was rare expression of inducible nitric oxide synthase (iNOS) in sham operation (SH) group; B: 14 d after bile duct ligation, the iNOS-immunoreactivity became stronger as compared with SH group; C: After relief of obstructive jaundice (OJ) by internal biliary drainage (ID), the expression of iNOS was markedly suppressed; D: The expression of iNOS obviously increased in rat liver of external biliary drainage (ED); E: Comparison of mean absorbance values of iNOS in rat liver tissues among the four groups. IHC: Immunohistochemical.
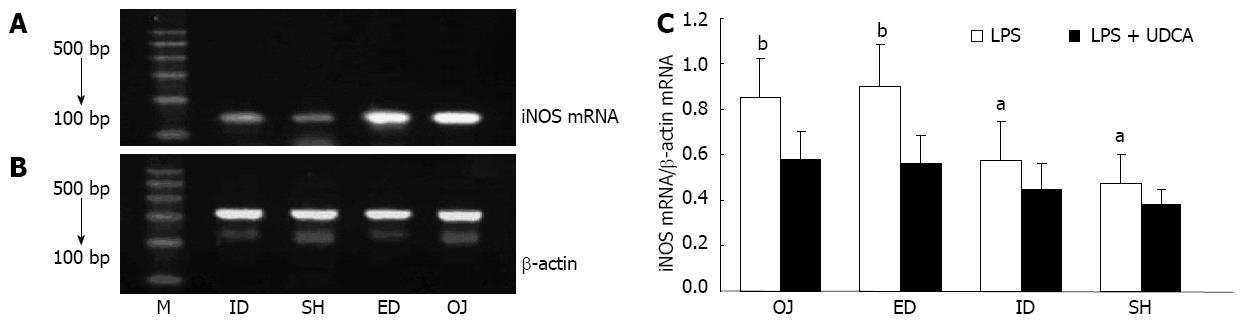
Figure 4 Ethidium bromide-stained agarose gel of inducible nitric oxide synthase reverse transcription polymerase chain reaction products, expression of inducible nitric oxide synthase messenger RNA on Kupffer cell interfered with lipopolysaccharide + ursodeoxycholic acid.
A: Lane M, 100 bp molecular marker. The 138 bp-inducible nitric oxide synthase (iNOS) band; B: The 300 bp-β-action products; C: Expression of iNOS messenger RNA (mRNA) interfered with lipopolysaccharide (LPS) as compared with LPS + ursodeoxycholic acid (UDCA). aP < 0.05, bP < 0.01 vs LPS + UDCA. M: Marker; ID: Internal biliary drainage; SH: Sham operation; ED: External biliary drainage; OJ: Obstructive jaundice.
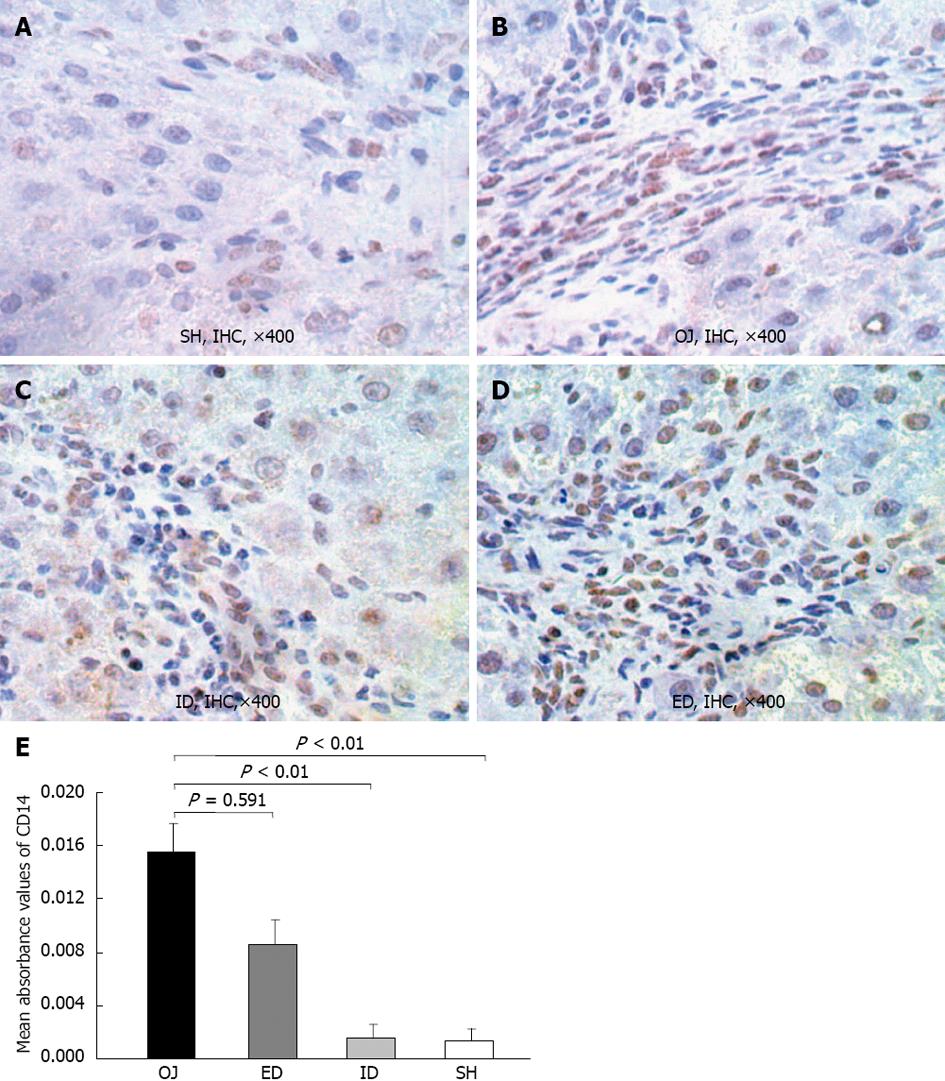
Figure 5 Representative immunohistochemical analysis of CD14 in rat liver tissues of sham operation, obstructive jaundice, internal and external biliary drainage groups.
A: CD14-immunoreactivity was detected mainly in the membrane of Kupffer cell on the edge of liver sinusoid and portal areas. There was slight expression of CD14 in sham operation (SH) rats; B: 14 d after bile duct ligation, the CD14-immunoreactivity became stronger as compared to SH rats; C: After relief of obstructive jaundice (OJ) by internal biliary drainage (ID), the expression of CD14 was markedly suppressed; D: The expression of CD14 in external biliary drainage (ED) rats was still at a high level; E: Comparison of mean absorbance values of CD14 in liver tissues among the four groups. IHC: Immunohistochemical.
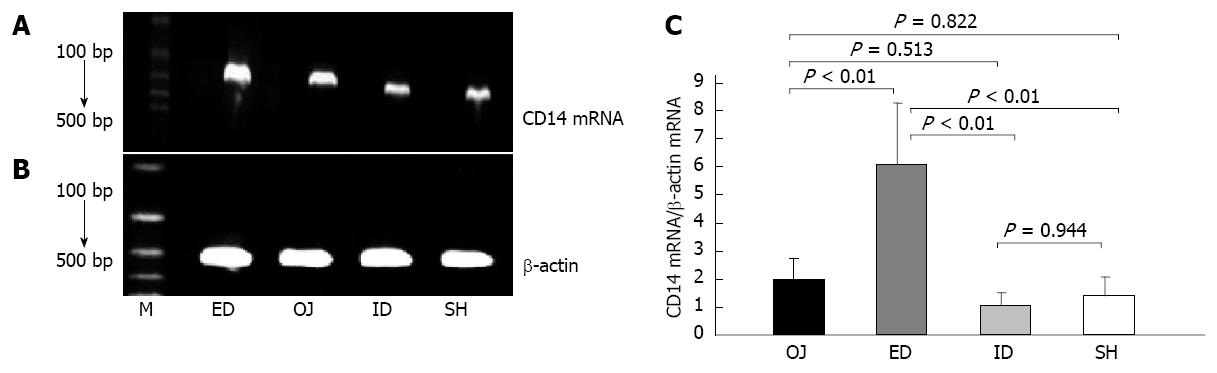
Figure 6 Ethidium bromide-stained agarose gel of CD14 reverse transcription polymerase chain reaction products products.
A: Lane M, 100 bp molecular marker. The 267 bp-CD14 band; B: The 300 bp-β-actin reverse transcription polymerase chain reaction products products; C: Comparison of CD14 messenger RNA (mRNA) expression by Kupffer cell interfered with lipopolysaccharide. CD14 mRNA levels were standardized using β-actin mRNA. M: Marker; ID: Internal biliary drainage; SH: Sham operation; ED: External biliary drainage; OJ: Obstructive jaundice.
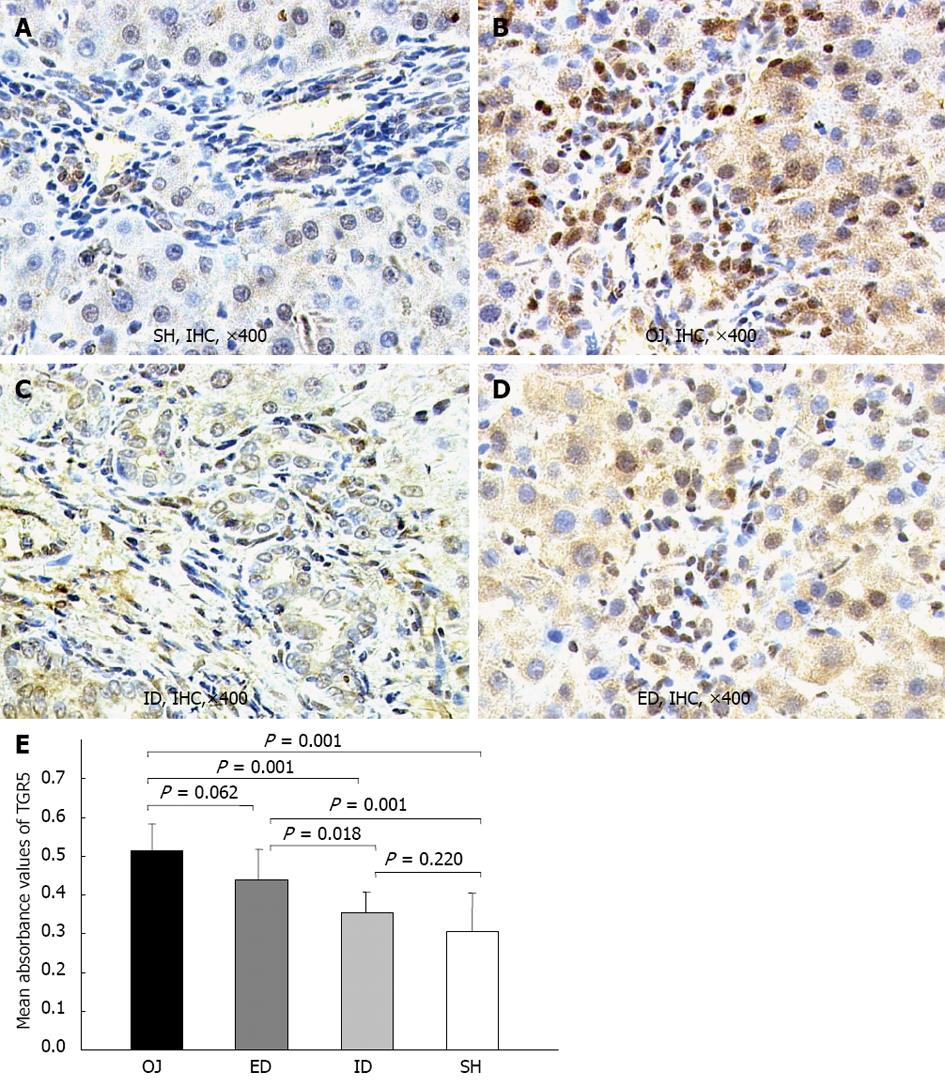
Figure 7 Representative immunohistochemical analysis of TGR5 in rat liver tissues of sham operation, obstructive jaundice, internal and external biliary drainage groups.
TGR5-immunoreactivity was detected mainly in the plasma membrane of Kupffer cell and its intracellular compartments, and also localized in some sinusoidal endothelial cells and biliary epithelial cells, but merely in hepatocytes. A: There was slight expression of TGR5 in rats of sham operation (SH); B: After bile duct ligation, the TGR5-immunoreactivity became stronger as compared to SH rats; C: After relief of jaundice by internal biliary drainage (ID), the expression of TGR5 was markedly suppressed; D: The expression of TGR5 in external biliary drainage (ED) rats was still at a high level; E: Comparison of mean absorbance values of TGR5 in rat liver tissues among the four groups. OJ: Obstructive jaundice; IHC: Immunohistochemical.
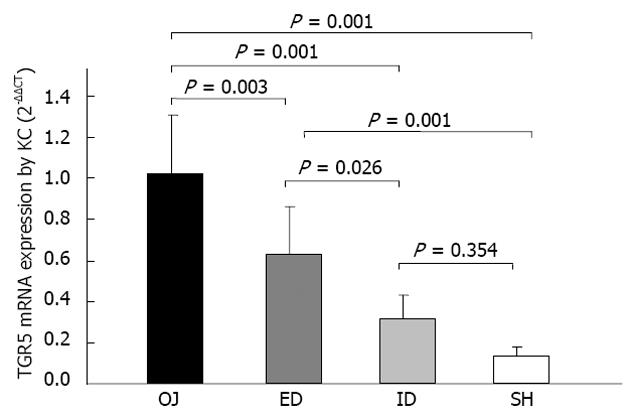
Figure 8 Effect of biliary drainages on TGR5 messenger RNA expression by Kupffer cell (2-ΔΔCT).
ID: Internal biliary drainage; SH: Sham operation; ED: External biliary drainage; OJ: Obstructive jaundice; KC: Kupffer cell; mRNA: Messenger RNA.
- Citation: Wang ZK, Xiao JG, Huang XF, Gong YC, Li W. Effect of biliary drainage on inducible nitric oxide synthase, CD14 and TGR5 expression in obstructive jaundice rats. World J Gastroenterol 2013; 19(15): 2319-2330
- URL: https://www.wjgnet.com/1007-9327/full/v19/i15/2319.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i15.2319