Copyright
©2012 Baishideng Publishing Group Co.
World J Gastroenterol. Jan 28, 2012; 18(4): 323-330
Published online Jan 28, 2012. doi: 10.3748/wjg.v18.i4.323
Published online Jan 28, 2012. doi: 10.3748/wjg.v18.i4.323
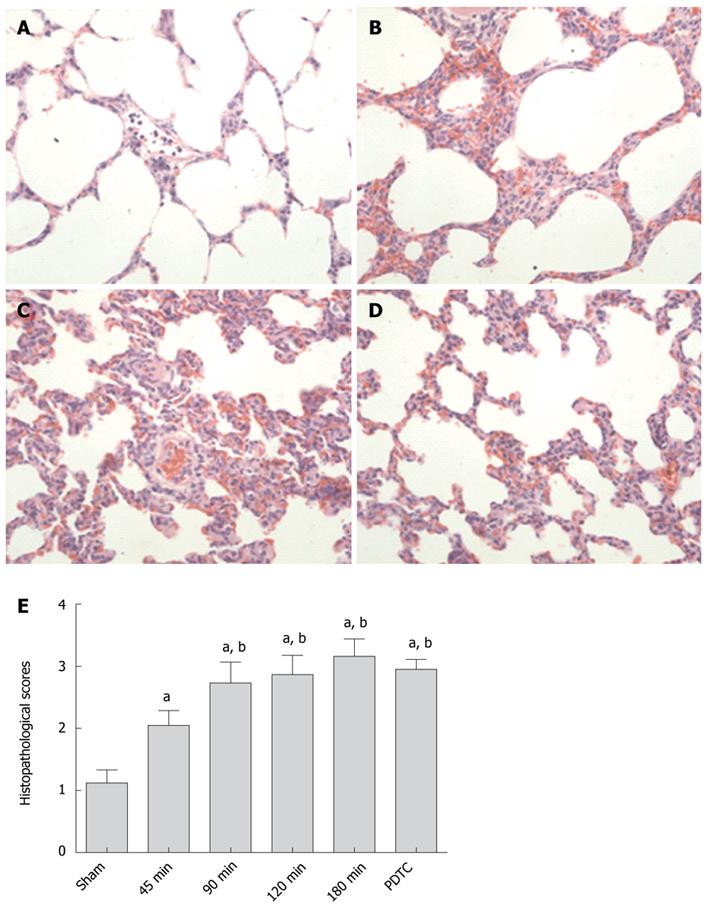
Figure 1 Representative lung tissue sections and histopathological scores.
A: Sham group; B: 90-min group; C: 180-min group; D: PDTC group. Alveolar, perivascular and interstitial edema, neutrophil infiltration, atelectasis, disruption of alveolar and bronchiolar epithelial cells, and local hemorrhage aggravated with prolonged CPT; E: Lung histopathological scores in different groups. The scores in the CPT groups were significantly higher than that in the sham group, but lower than in the PDTC group. aP < 0.05 vs sham group; bP < 0.05 vs 45-min group. PDTC: Pyrrolidinedithiocarbamate; CPT: Cold preservation time.
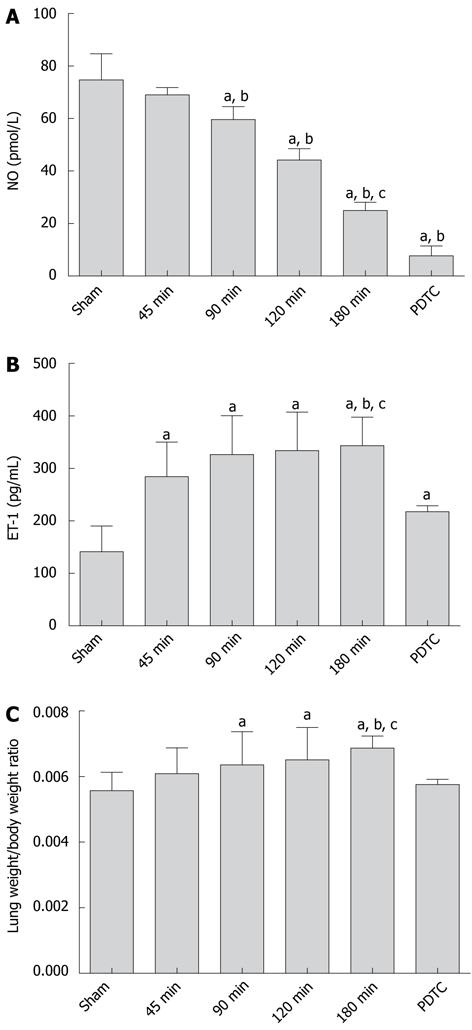
Figure 2 Serum NO, ET-1 level and lung weight/body weight ratio.
A: NO levels in different groups. With CPT prolonged, NO level decreased significantly, and became even lower with PDTC injection post-reperfusion; B: ET-1 level in different groups. With CPT prolonged, ET-1 level increased significantly compared with the sham group. The PDTC group had a significantly lower ET-1 level than 180-min group; C: Lung weight/body weight ratios in different groups. The ratios increased compared with the sham group. Significant difference was observed between the 180-min group and PDTC group. aP < 0.05 vs sham group; bP < 0.05 vs 45-min group; cP < 0.05 vs PDTC group. PDTC: Pyrrolidinedithiocarbamate; CPT: Cold preservation time; NO: Nitric oxide; ET: Endothelin.
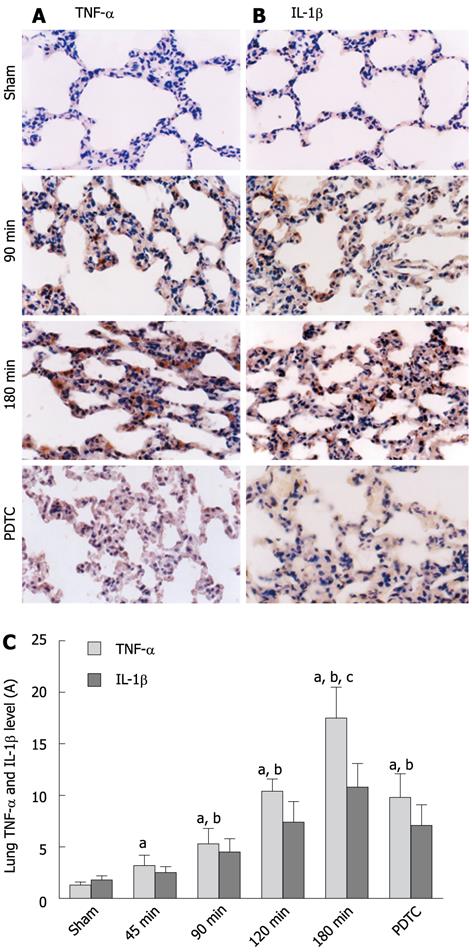
Figure 3 Immunohistochemical sections of tumor necrosis factor-α and interleukin-1β in lung (× 400).
A: Immunohistochemistry sections of TNF-α with different CPT; B: Immunohistochemical staining of IL-1β with different CPT; C: Analysis of TNF-α and IL-1β levels. The results were expressed as absorbance unit (A). aP < 0.05 vs sham group; bP < 0.05 vs 45-min group; cP < 0.05 vs PDTC group. PDTC: Pyrrolidinedithiocarbamate; CPT: Cold preservation time; TNF: Tumor necrosis factor; IL: Interleukin.
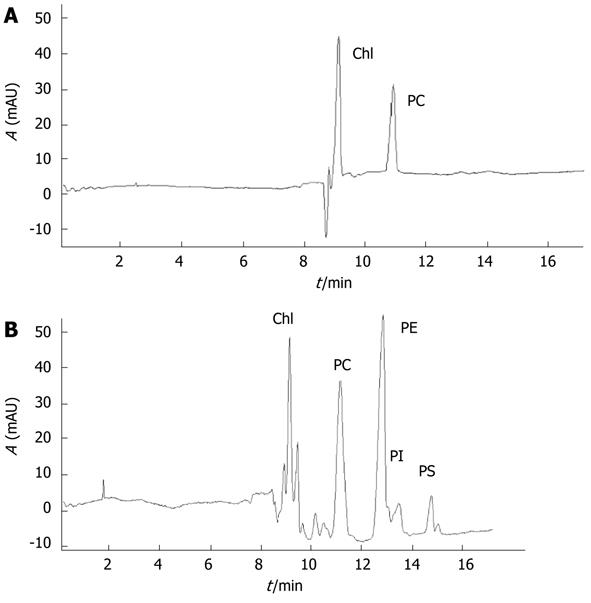
Figure 4 Pulmonary phospholipids separated by micellar electrokinetic capillary chromatography.
A: Standard PC electropherogram; B: Pulmonary phospholipid extracts electropherogram. Chl: Chloroform. AUC of different chromatographic peaks represent the relative quantities of different pulmonary phospholipid components. PC: Phosphatidylcholine; AUC: Area under curve; PE: Phosphatidylethanolamine; PI: Phosphatidylinositol; PS: Phosphatidylserine.
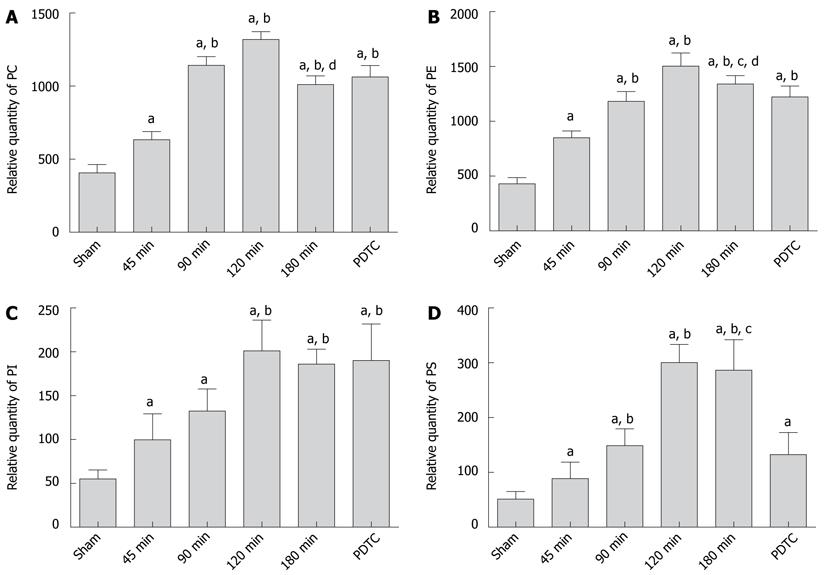
Figure 5 Relative quantities of pulmonary phospholipids.
A: Relative quantity of PC; B: Relative quantity of PE; C: Relative quantity of PI; D: Relative quantity of PS. With CPT prolonged, the levels of pulmonary phospholipids increased significantly, reaching a peak in the 120-min group, and then declined in the 180-min group. The use of PDTC could inhibit the expression of PE and PS, but could not observe significant effect in PC and PI. aP < 0.05 vs sham group; bP < 0.05 vs 45-min group; cP < 0.05 vs PDTC group; dP < 0.05 vs 120-min group. PDTC: Pyrrolidinedithiocarbamate; CPT: Cold preservation time; PC: Phosphatidylcholine; PE: Phosphatidylethanolamine; PI: Phosphatidylinositol; PS: Phosphatidylserine.
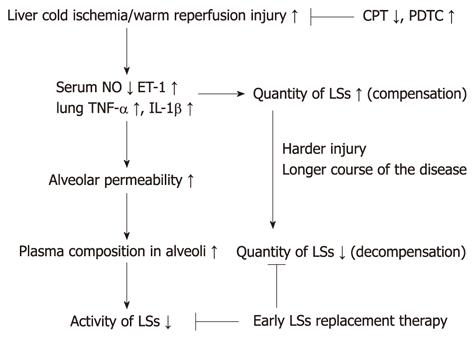
Figure 6 A schematic diagram for the mechanism of lung surfactants in liver-transplantation-related acute lung injury.
With prolonged CPT of donor liver, the cold ischemia/warm reperfusion injury increased, inducing an imbalance of serum NO/ET-1 levels and production of TNF-α and IL-1β in lungs. Consequently, alveolar permeability increased, and the plasma composition in the alveoli inactivated the lung surfactants (LSs). In the early stage of ALI, LSs increased in compensation, but in the decompensation stage, the level of LSs decreased, and ALI was aggravated. Shorter CPT or using PDTC may reduce ALI, and surfactant replacement therapy at an earlier stage may be useful in the treatment of ALI. PDTC: Pyrrolidinedithiocarbamate; CPT: Cold preservation time; TNF: Tumor necrosis factor; IL: Interleukin; ALI: Acute lung injury; NO: Nitric oxide; ET: Endothelin.
- Citation: Jiang A, Liu C, Liu F, Song YL, Li QY, Yu L, Lv Y. Liver cold preservation induce lung surfactant changes and acute lung injury in rat liver transplantation. World J Gastroenterol 2012; 18(4): 323-330
- URL: https://www.wjgnet.com/1007-9327/full/v18/i4/323.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i4.323