Copyright
©2005 Baishideng Publishing Group Inc.
World J Gastroenterol. Feb 7, 2005; 11(5): 676-680
Published online Feb 7, 2005. doi: 10.3748/wjg.v11.i5.676
Published online Feb 7, 2005. doi: 10.3748/wjg.v11.i5.676
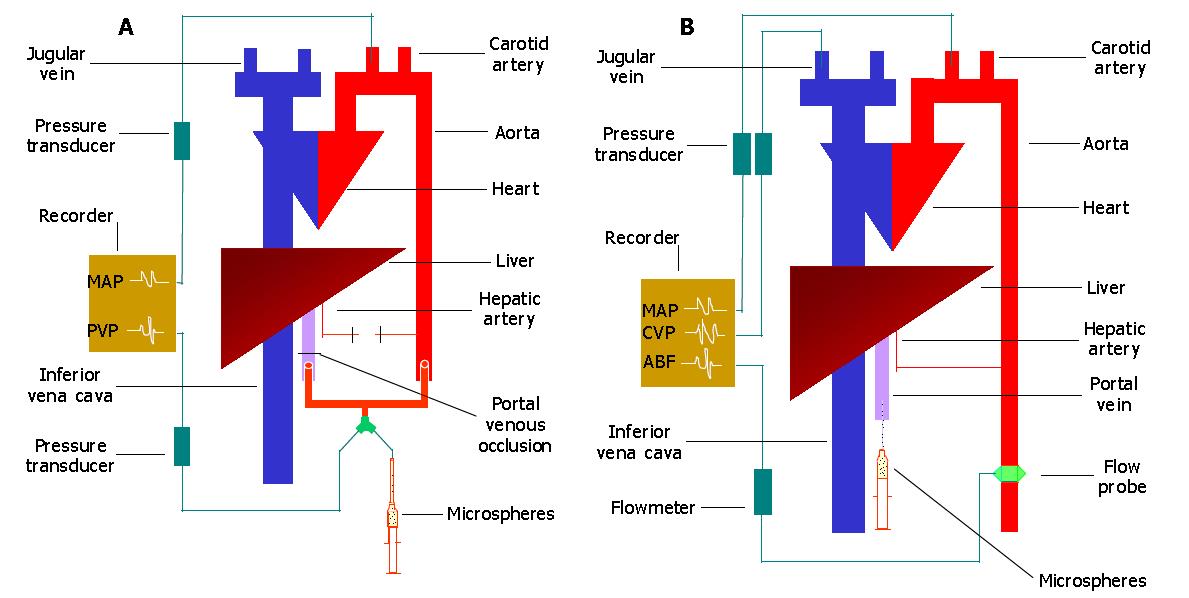
Figure 1 Diagram of experimental models.
Rats in both models were eviscerated. In model 1, the hepatic artery was divided and the liver was then perfused only by aortic blood via the portal vein (A). In model 2, the liver was perfused only by the hepatic artery (B). Latex microspheres were injected intraportally and the resultant changes in mean arterial pressure (MAP), central venous pressure (CVP) and portal venous pressure (PVP) were monitored by the cannulae in the carotid artery, jugular vein and portal vein, respectively. Aortic blood flow (ABF) was measured by an electric magnetic flow probe placed around the abdominal aorta.
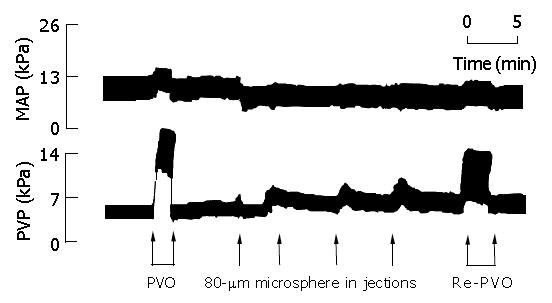
Figure 2 Mean arterial pressure (MAP) and portal venous pressure (PVP) recordings from a rat in group 2 of experiment 1 during portal venous occlusion (PVO), intraportal injection of 80-µm diameter microspheres and re-PVO after microsphere injection.
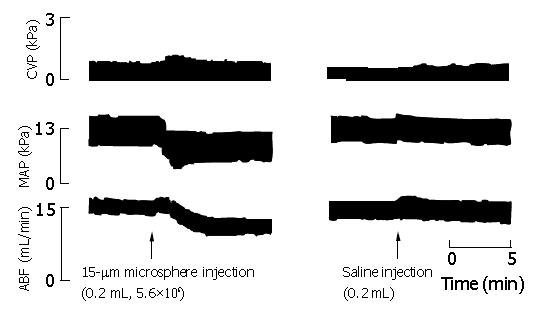
Figure 3 Central venous pressure (CVP), mean arterial pressure (MAP) and aortic blood flow (ABF) recordings from experiment 2 after intraportal injection of 15-µm diameter microspheres in a liver-innervated rat (group 1) and saline injection in a control rat (group 3).
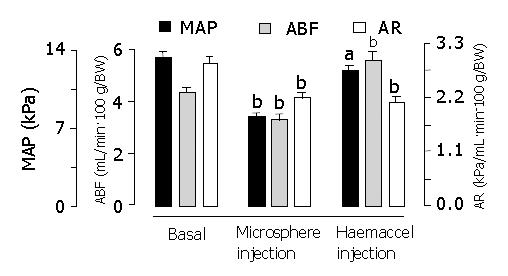
Figure 4 Mean arterial pressure (MAP), aortic blood flow (ABF) and aortic resistance (AR) after intraportal injection of 15-µm diameter microspheres and subsequent Haemaccel injection in group 5 of experiment 2.
aP<0.05, bP<0.01 vs Basal.
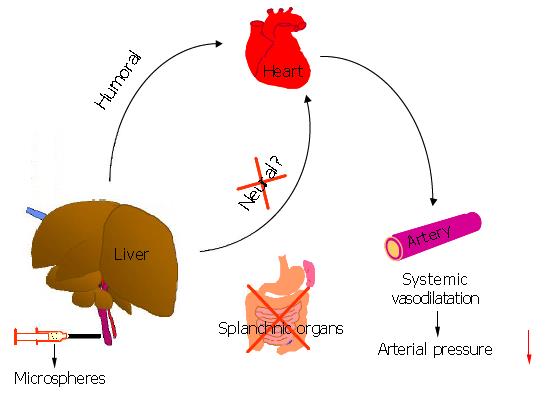
Figure 5 Illustration of the hepato-cardiovascular response and its regulatory mechanism.
Intrahepatic stimulation induced by microspheres led to release of humoral mediator (s) from the liver, which, in turn, caused systemic vasodilatation and subsequently the reduction in arterial blood pressure.
- Citation: Li XN, Benjamin IS, Alexander B. Hepato-cardiovascular response and its regulation. World J Gastroenterol 2005; 11(5): 676-680
- URL: https://www.wjgnet.com/1007-9327/full/v11/i5/676.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i5.676