Copyright
©The Author(s) 2022.
World J Clin Cases. Aug 6, 2022; 10(22): 7950-7959
Published online Aug 6, 2022. doi: 10.12998/wjcc.v10.i22.7950
Published online Aug 6, 2022. doi: 10.12998/wjcc.v10.i22.7950
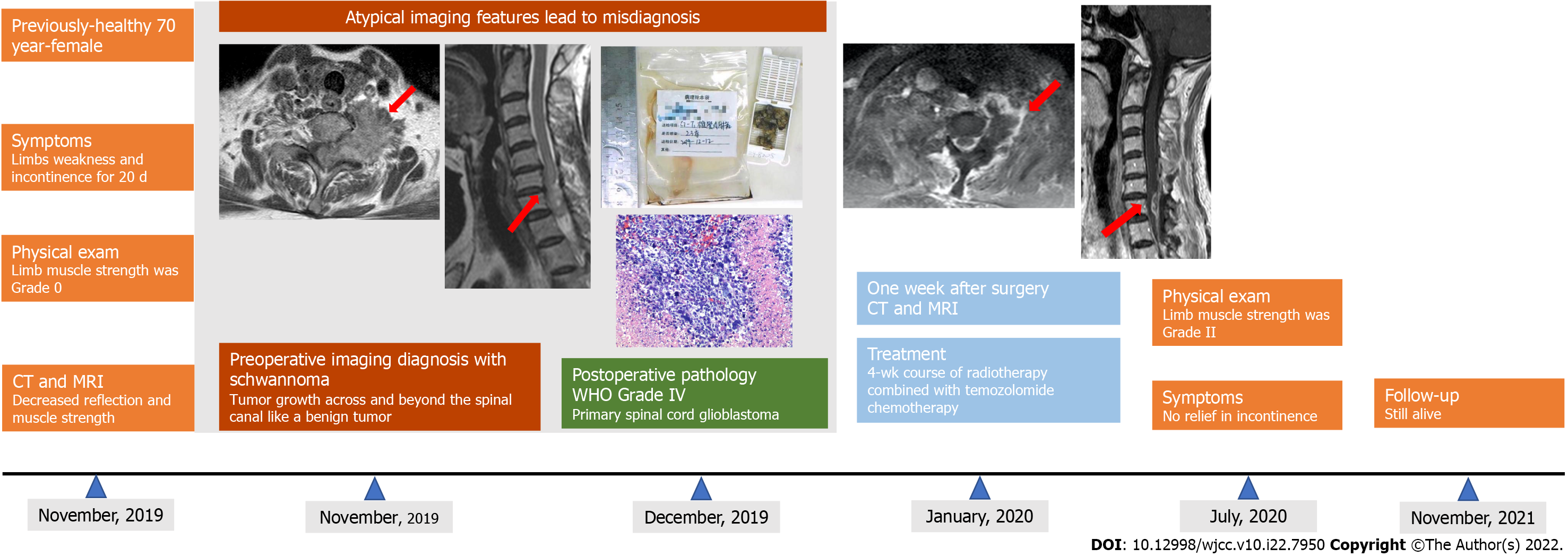
Figure 1 Timeline of this case report.
CT: Computed tomography; MRI: Magnetic resonance imaging; WHO: World Health Organization.
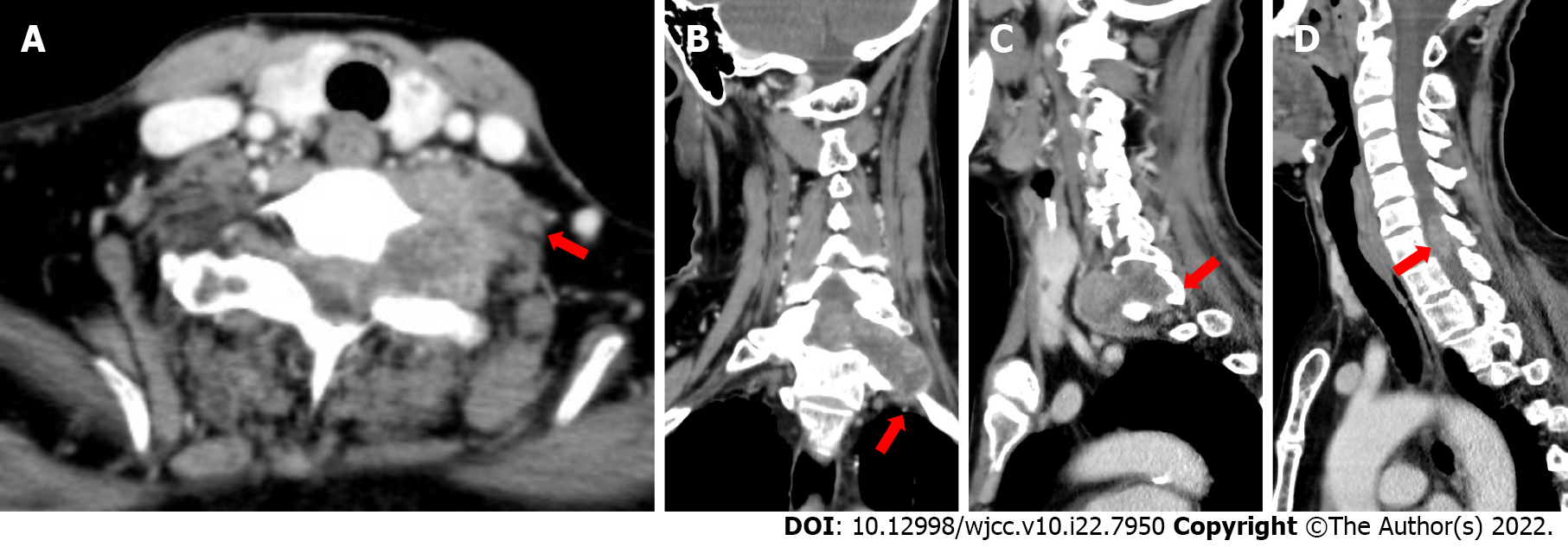
Figure 2 Computed tomography images of lesions of the present case.
A and B: The tumor was irregular in shape, growing across and beyond the left foramina; C: The left intervertebral foramina was enlarged with inhomogeneous enhancement; D: The lesion was intramedullary and indistinctly demarcated from the surrounding spinal cord.
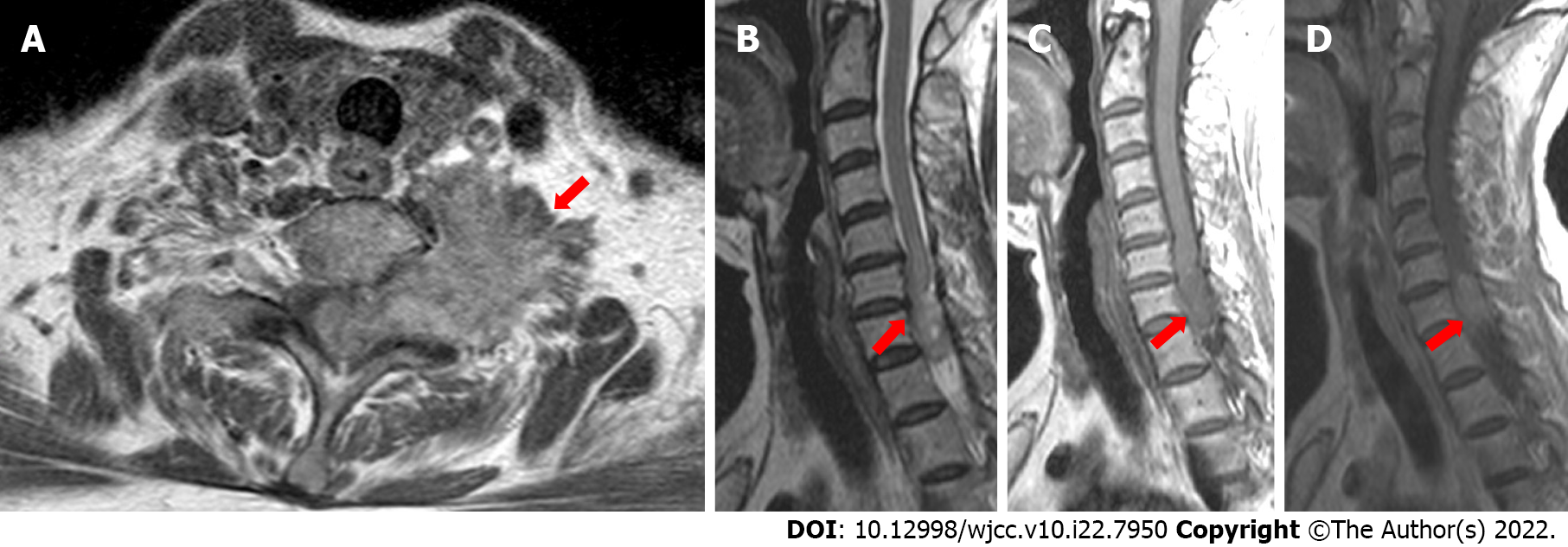
Figure 3 Magnetic resonance images of the present case.
A-C: The tumor was irregular in shape with a rough margin, and having slightly lower signal intensity on T1-weighted imaging and slightly higher signal intensity on T2-weighted imaging; D: The mass had heterogeneous enhancement.
Figure 4 Diagnosis of World Health Organization Grade IV primary spinal cord glioblastoma was made.
A: Resected gross tissue; B and C: Histopathology imaging (magnification × 200). Pleomorphic astrocytic cells with marked nuclear atypia and brisk mitotic activity were observed along with necrosis and microvascular proliferation. Immunohistochemically, the cells were slightly positive for glial fibrillary acidic protein, p53, and vimentin and negative for S-100, isocitrate dehydrogenase, and H3K27M. The proliferation index (measured by Ki67) was found to be at 30%.
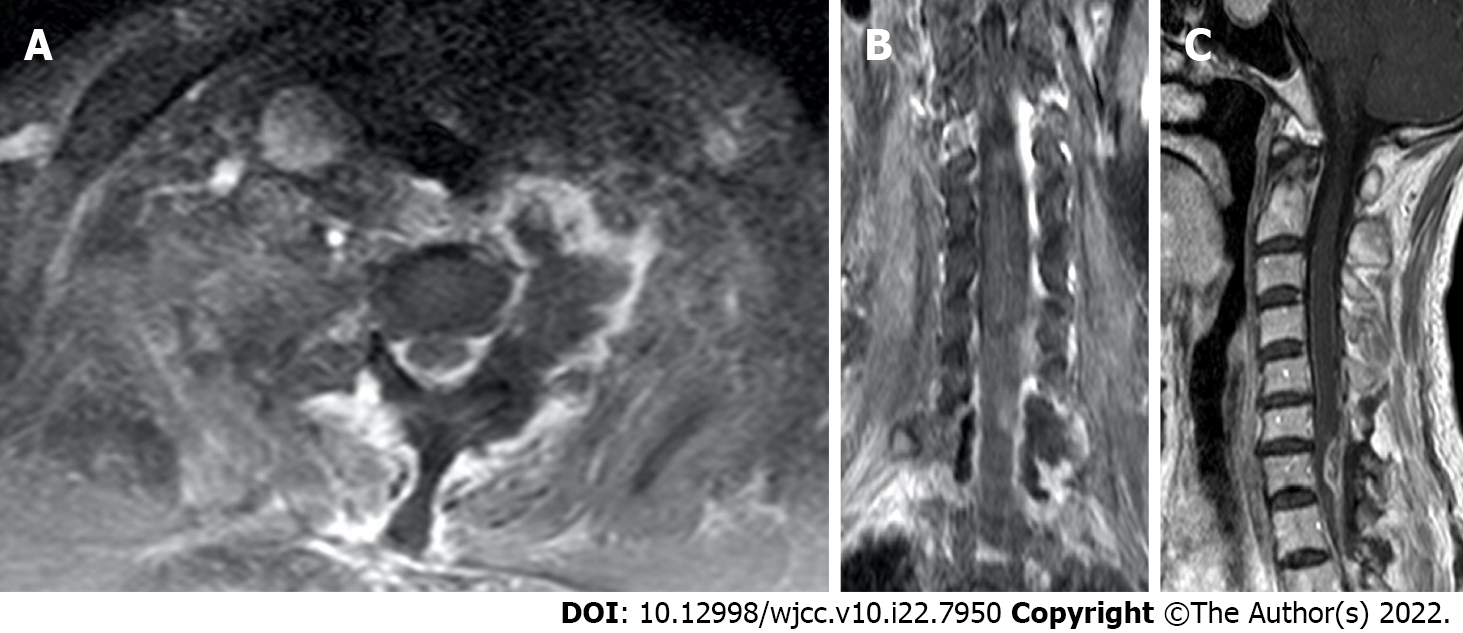
Figure 5 Magnetic resonance imaging re-examination 1 wk after tumor resection.
A: Axial view; B: Coronal view; C: Sagittal view.
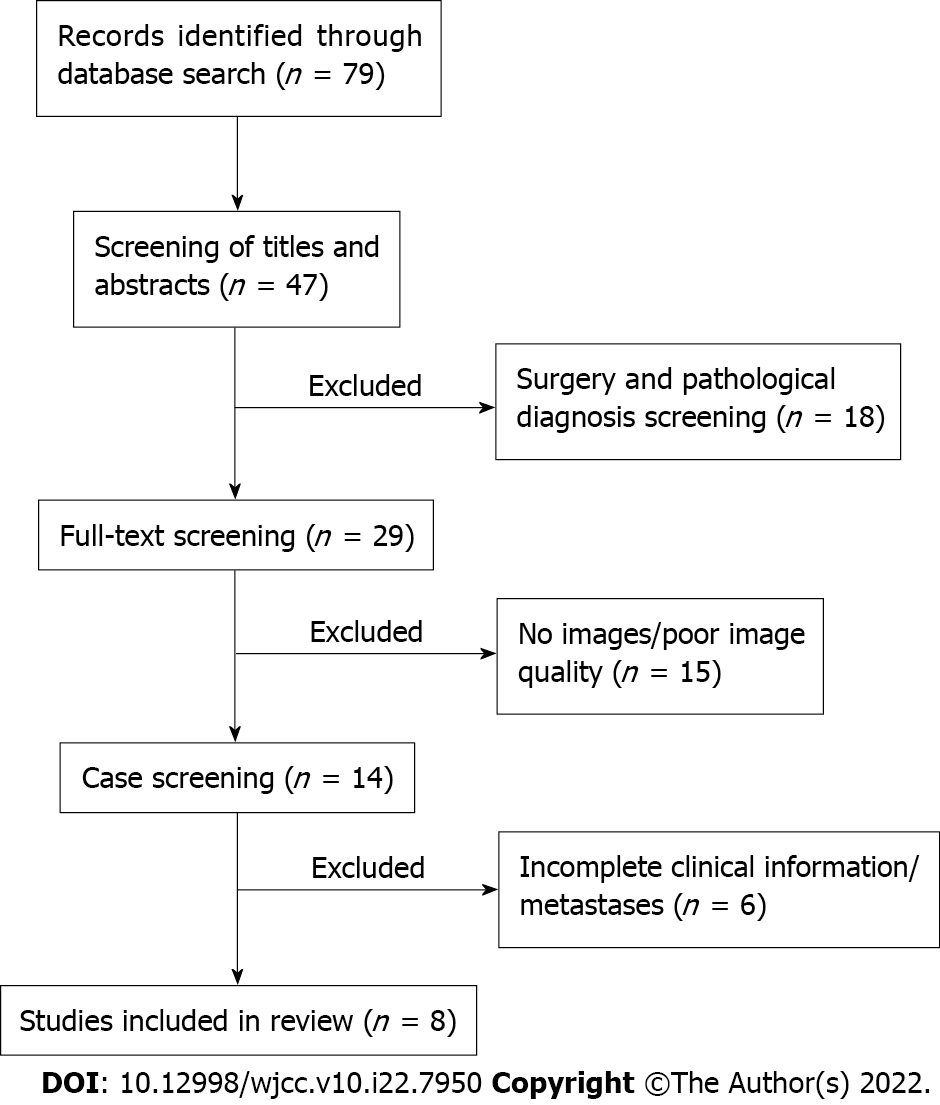
Figure 6 Detailed flow of screening of publications for review of the literature.
- Citation: Liang XY, Chen YP, Li Q, Zhou ZW. Atypical imaging features of the primary spinal cord glioblastoma: A case report. World J Clin Cases 2022; 10(22): 7950-7959
- URL: https://www.wjgnet.com/2307-8960/full/v10/i22/7950.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i22.7950