Copyright
©The Author(s) 2024.
World J Gastroenterol. Mar 28, 2024; 30(12): 1663-1669
Published online Mar 28, 2024. doi: 10.3748/wjg.v30.i12.1663
Published online Mar 28, 2024. doi: 10.3748/wjg.v30.i12.1663
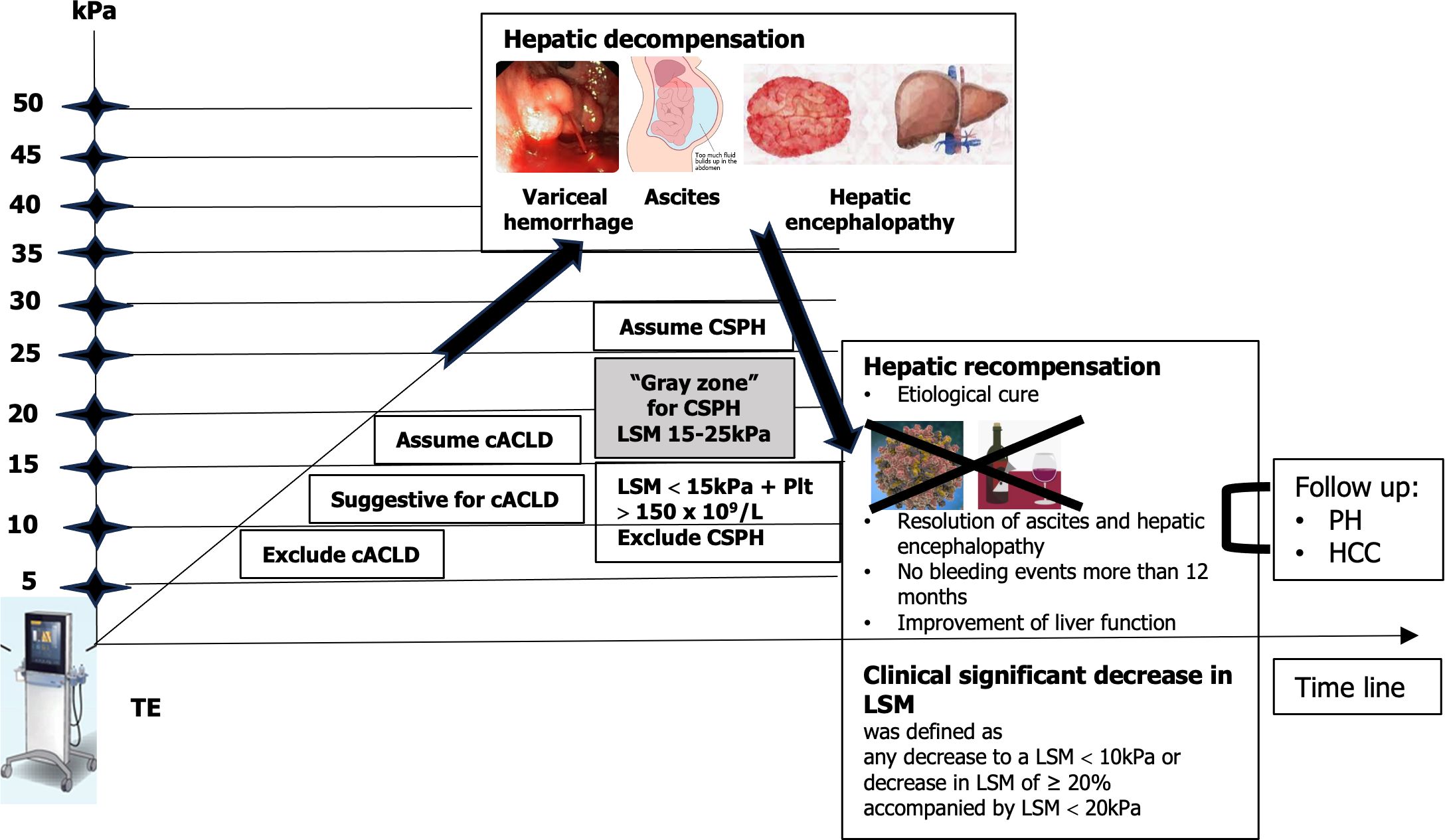
Figure 2 Use of noninvasive tests according to the rule of 5 to determine compensated advanced chronic liver disease and clinically significant portal hypertension.
Dynamic use of noninvasive tests for assessment of hepatic decompensation or recompensation. Patients having a liver stiffness measurement (LSM) < 10 kPa rules out compensated advanced chronic liver disease (cACLD) in the absence of other clinical/imaging signs. LSM values between 10 kPa and 15 kPa are suggestive of cACLD, and LSM ≤ 15 kPa plus platelets ≥ 150 × 109/L rule out clinically significant portal hypertension (CSPH) in the majority of etiologies. LSM measured by transient elastography (TE) > 15 kPa are considered as a high likelihood of cACLD in all etiologies. Patients with intermediate values of LSM between 15 kPa and 25 kPa are in a “gray zone” of CSPH. The best cutoff to determine the presence of CSPH was an LSM ≥ 25 kPa (specificity and positive predictive value > 90%) in alcoholic liver disease, chronic hepatitis B, chronic hepatitis C, and non-obese patients with nonalcoholic steatohepatitis. Hepatic recompensation includes all of the following criteria: Suppression or removal of the underlying etiology of cirrhosis; Resolution of ascites and hepatic encephalopathy after discontinuation of diuretics and prophylactic therapies; Absence of variceal bleeding for 12 months; Sustained improvement of biochemical liver function, assessed by serum albumin, bilirubin, and international normalized ratio[13]. LSM: Liver stiffness measurement; HCC: Hepatocellular carcinoma; PH: Portal hypertension; TE: Transient elastography.
- Citation: Peltec A, Sporea I. Multiparametric ultrasound as a new concept of assessment of liver tissue damage. World J Gastroenterol 2024; 30(12): 1663-1669
- URL: https://www.wjgnet.com/1007-9327/full/v30/i12/1663.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i12.1663