Copyright
©The Author(s) 2018.
World J Gastroenterol. Nov 14, 2018; 24(42): 4821-4834
Published online Nov 14, 2018. doi: 10.3748/wjg.v24.i42.4821
Published online Nov 14, 2018. doi: 10.3748/wjg.v24.i42.4821
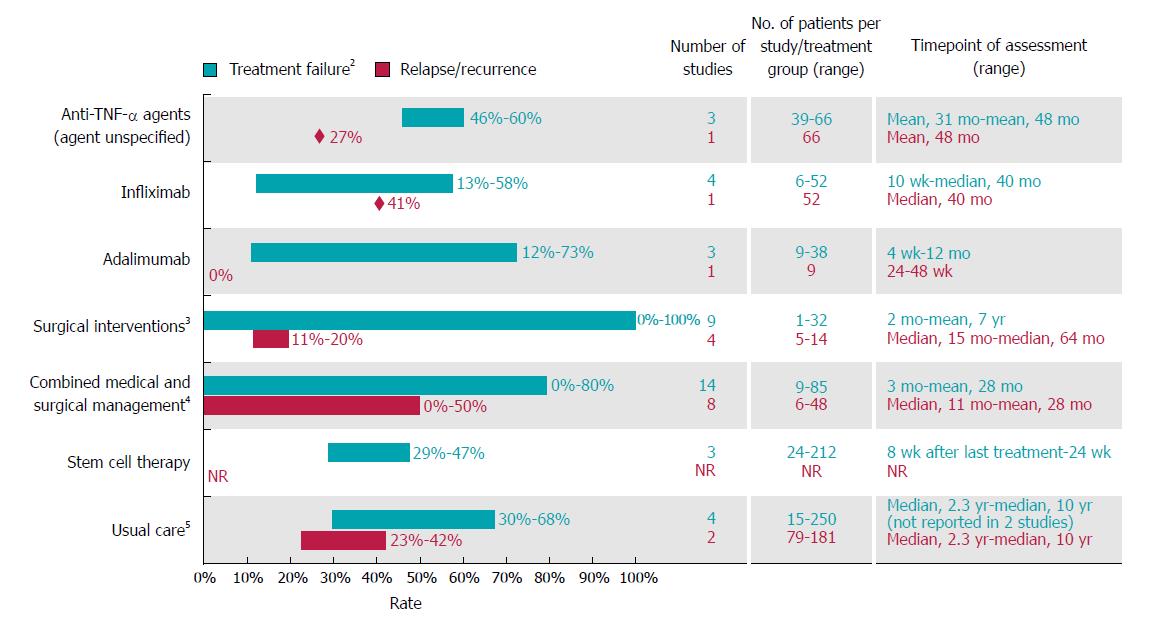
Figure 4 Rates of treatment failure and relapse or recurrence among Crohn’s disease patients with complex perianal fistula1.
1For studies with mixed populations (i.e., patients with any fistula and those with complex fistula), only results for patients with Crohn’s disease and complex perianal fistulas were considered; 2Defined as lack of or inadequate response to therapy (i.e., lack of complete response or lack of healing response); 3Most studies (10 of 12) reported outcomes for surgical procedures that were considered major procedures in this review, ligation of intersphincteric fistula tract, advancement flap repair, mucosal advancement flap with injection of platelet-rich plasma into the fistula tract, myocutaneous flaps and proctocolectomy with permanent ileostomy, gracilis muscle transposition, over-the-scope-clip proctology, fistula tract transposition or standard surgical management (including both major and minor procedures)[34-36,42,48-50,53,54,66]. One study reported outcomes with permanent seton (minor procedure; other minor procedures reported in studies mentioned above included biologic fistula plug, and fibrin glue)[52]. One study did not specify the type of surgery[11]; 4Most (12 of 15) studies assessed surgical procedures that are considered minor procedures (seton drainage (most frequently), abscess drainage, fistulotomy, fibrin glue)[10,29,38-41,43,67-71]. Two studies assessed surgical procedures that are considered major procedures (mucosal advancement flap, resection, stoma, proctectomy)[37,51]. Surgery type was not defined in one study[72]; 5Defined as usual care used at each centre [standard medical care (excluding anti-tumour necrosis factors) and surgery in two studies, and standard medical care (including anti-tumour necrosis factor alpha agents) and surgery in two studies]. TNF-α: Tumour necrosis factor alpha.
- Citation: Panes J, Reinisch W, Rupniewska E, Khan S, Forns J, Khalid JM, Bojic D, Patel H. Burden and outcomes for complex perianal fistulas in Crohn’s disease: Systematic review. World J Gastroenterol 2018; 24(42): 4821-4834
- URL: https://www.wjgnet.com/1007-9327/full/v24/i42/4821.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i42.4821