Published online May 14, 2017. doi: 10.3748/wjg.v23.i18.3374
Peer-review started: November 24, 2016
First decision: December 28, 2016
Revised: January 18, 2017
Accepted: February 7, 2017
Article in press: February 8, 2017
Published online: May 14, 2017
Various degrees of esophageal injury have been described after radiofrequency ablation performed for treatment of atrial fibrillation. The main mechanism of injury is thermal and may lead to a range of esophageal mucosal changes, some clinically insignificant, however when deep ulceration occurs, this may be further complicated by perforation and mediastinitis, a rare but life threatening sequelae. We present a case of a severe esophageal injury leading to mediastinitis, with interesting endoscopic findings.
Core tip: We report a case of esophageal perforation complicated by mediastinitis. Our report demonstrates the clinical course of a rare, yet deadly complication of radiofrequency ablation, with unique endoscopic findings. We believe that this report and brief review of the literature will serve an important reminder of this complication and its consequences, requiring a high index of suspicion for early diagnosis and treatment. Our report also serves as a reminder that a unified approach to treatment has yet to be established.
- Citation: Katz-Agranov N, Nevah Rubin MI. Severe esophageal injury after radiofrequency ablation - a deadly complication. World J Gastroenterol 2017; 23(18): 3374-3378
- URL: https://www.wjgnet.com/1007-9327/full/v23/i18/3374.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i18.3374
Radiofrequency ablation (RFA) is the electrical isolation of the pulmonary veins and the linear ablation of the left atrial roof, mitral isthmus and cavo-tricuspid isthmus to eliminate the focus causing atrial fibrillation (AF). This procedure has become the standard of care for drug-refractory symptomatic AF[1] and it is being increasingly performed as first line therapy in certain patient populations[1]. The extent of RFA varies from isolation of the pulmonary veins, to complex and extensive ablation in the left atrium, sometimes involving its entire posterior wall. Although the procedure is considered a safe one, the significant anatomical variability in the relationship between the esophagus and left atrium, places the esophagus in a vulnerable position, prone to injury. Various variables effecting heat transfer to the esophagus have been identified in recent years and new strategies to minimize the risk of esophageal injury are now utilized, however they have not eliminated its risk. The main mechanism of injury is thermal, resulting in esophageal dysmotility, ulceration or perforation, which may be further complicated by mediastinitis or left atrio-esophageal fistula formation, both rare but life threatening sequelae.
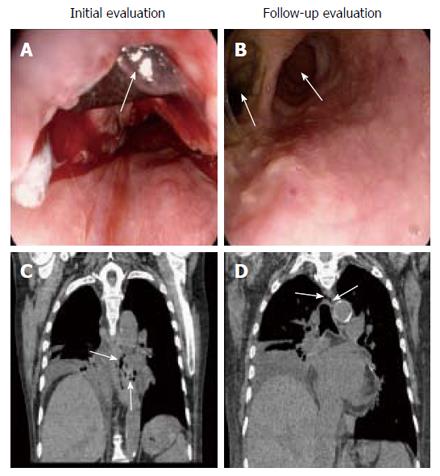
A 75-year-old man with past history significant for ischemic cardiomyopathy, biventricular congestive heart failure (ejection fraction of 20%-25%) and AF, was admitted to our institution for elective RFA for treatment of symptomatic atrial fibrillation, which was refractory to medical management. The procedure performed included complete pulmonary vein isolation, a mitral isthmus line and posterior wall ablation (aka: box lesion). A 7.5 French Johnson and Johnson EZ Steer Thermocool NAV Bi-Directional D-F curve irrigation catheter was used to produce catheter ablation, with a maximum power of 50 Watts and a total ablation time of 3401 s. Use of esophageal temperature probe was not documented. The RFA was successful and uneventful, however on day seven post procedure, the patient complained of retro-sternal chest pain, dysphagia and odynophagia followed by hematemesis, which resulted in a significant drop in hemoglobin and hematocrit and quickly led to hypovolemic shock. Immediate resuscitation was initiated and the patient was taken for emergent esophagogastroduodenoscopy (EGD) revealing a large clot extending along the entire length of the esophagus, and old blood in the stomach and duodenum. The esophageal blood clot was extracted, revealing a 2 cm ulcer in the mid-esophagus with active oozing (Figure 1A). No endoscopic intervention was performed at that time. A non-contrast chest CT was urgently performed, revealing esophageal perforation and mediastinitis at a level adjacent to the posterior aspect of the left atrium (LA) (Figure 1B). Treatment was initiated with antibiotics, total parenteral nutrition (TPN) and esophageal rest. A follow-up EGD one week later revealed ulceration measuring 4 cm in diameter with a walled-off false lumen (Figure 1C), no intervention was performed. The patient was not responding to aggressive medical management, he remained in shock, requiring vasopressors, developed acute kidney injury requiring dialysis and shock liver. Two days later, the patient was taken for endoscopic stent placement, which was unsuccessful, as the patient was in critical condition. At that time he and his family requested transition to comfort care measures and asked that no further invasive treatment be undertaken. The patient expired soon thereafter.
Major complications observed with RFA (radiofrequency ablation) for AF are cardiac in nature however, damage to neighboring structures may also occur. Surrounding intracardiac structures at risk for damage include the aorta, coronary sinus, left atrial appendage, valves, chordae tendineae and atrial appendage. Extracardiac structures at risk for damage include the upper gastrointestinal structures such as the esophagus and stomach[2], in which both structural and functional damage has been described[2,3], pulmonary bronchi[4], the adjacent nerves including the vagus nerve and right phrenic nerve[3,5], aorta and the thoracic spine[6]. The proximity of the esophagus to the posterior wall of the left atrium places it in a particularly vulnerable position[7], prone to various degrees of thermal injury[8-10].
Esophageal perforation is a rare but life-threatening complication of RFA for atrial fibrillation[11-15] as demonstrated by the case presented. Factors that determine heat transfer to the esophagus during catheter ablation include the magnitude and duration of local tissue heating, as well as atrial tissue thickness[16,17] and the thickness and character of intervening connective tissue, including adipose tissue between the heart and esophagus[7,8,16,18]. Catheter tip size, contact pressure and catheter orientation are also important variables that determine what percentage of applied radiofrequency energy is actually delivered to cardiac tissue. Several techniques have been utilized to minimize the risk of esophageal injury, including avoidance of ablation near the esophagus, titration of radiofrequency energy delivery at the posterior left atrial endocardium and the use of alternative ablation methods[18-20].
Recent studies using surveillance endoscopy after RFA for atrial fibrillation, report various degrees of esophageal mucosal damage in approximately 15% of patients post catheter ablation[18,20-22]. Prior to implementation of esophageal localization techniques, esophageal mucosal changes consistent with thermal injury were more prevalent, and in one single center study reported in up to 47% of patients, with necrotic or ulcer-like changes demonstrated in 18% of those patients[23]. Esophageal perforation and atrio-esophageal fistula formation are an extremely rare, yet detrimental sequela of the aforementioned esophageal injuries, which may lead to death in up to 80% of patients[12] and although utilization of various preventive measures have decreased the risk of severe esophageal injury, it has not been eliminated. The reasons for the high mortality rates are thought to be due to failure of early recognition as a result of lack of clinical awareness, delayed presentation, as exemplified by our case, and complex surgical repair that may be required for treatment[12,14]. Therefore, a high index of suspicion and early recognition and treatment are imperative for prevention of poor outcomes.
Treatment of RFA-induced esophageal complications varies and should be managed by a multidisciplinary approach. Esophageal lesions may be treated with acid suppression, esophageal rest, parenteral nutrition or stent placement[24]. Treatment options for more severe injuries, such as perforation, mediastinitis and atrio-esophageal fistulas, range from conservative management to invasive approaches including endoscopic stenting, thoracostomy, diversion, primary surgical repair or a combination of those[25]. There has been controversy in the literature regarding indications for surgical management of esophageal perforation[26-28] and its mortality benefit, especially when treatment is delayed and randomized controlled studies on this subject are lacking. Conservative management has been advocated for cases of iatrogenic perforation, postemetic esophageal perforation or intrathoracic perforation as well as the presence of severe comorbidities and medical contraindications to surgery. Some suggest that medical treatment can be implemented for contained perforation in the mediastinum and the visceral pleura without penetration to another body cavity or when the perforation drains back into the esophagus[26-30]. The use of endoscopic stents, has also been taking the front line in management of esophageal injuries[31]. Despite the controversies, all are agreed upon the fact that early recognition of esophageal perforation plays a major prognostic role[32], therefore it is pertinent to have a high index of suspicion in patients presenting with classic symptoms and even more so in those with recent history of an invasive procedure, such as RFA. The advancements in imaging technologies as well as endoscopic techniques may allow in the future for a broader range of minimally invasive treatment options, even in patients who are high risk candidates for surgical intervention, however a unified approach to treatment has yet to be established.
A 75-year-old patient with ischemic cardiomyopathy and refractory atrial fibrillation underwent radiofrequency ablation and developed retrosternal chest pain, dysphagia and odynophagia and hematemesis, seven days later.
The patient became hypotensive, tachycardic and oliguric and rapidly developed multiorgan failure, gross blood was extracted from his nasogastric tube.
Peptic ulcer disease, esophagitis, atrioesophageal fistula, atriobronchial fistula.
Significant drop in Hemoglobin and hematocrit, elevated creatinine and BUN and abnormally elevated liver enzymes.
Initial esophagogastroduodenoscopy (EGD) revealed a large clot extending along the entire length of the esophagus with an underlying 2 cm ulcer, actively oozing. A non-contrast chest CT subsequently demonstrated esophageal perforation and mediastinitis at a level adjacent to the posterior aspect of the left atrium. A follow-up EGD revealed ulceration measuring 4 cm in diameter with a walled-off false lumen.
Pathological diagnosis was not made in this case.
After initial resuscitation the patient was started on antibiotics, total parenteral nutrition and esophageal rest. At a later date an endoscopic esophageal stent placement was pursued, however it was unsuccessful.
Esophageal injury is a well reported complication of radiofrequency ablation however, perforation and mediastinitis are a rare, yet life threatening complication. Treatment options and outcomes have been variable and largely depend on time of diagnosis and treatment as well as patient comorbidities.
Radiofrequency ablation refers to the isolation of the pulmonary veins and other electric foci, commonly located along the posterior wall of the left atrium, to ablate unwanted electrical discharges resulting in atrial fibrillation.
Development of esophageal injury may complicate radiofrequency ablation. Prompt recognition is pertinent and management with a multidisciplinary approach is necessary.
This report demonstrates the clinical course of esophageal perforation, a devastating complication of radiofrequency ablation. Treatment options vary and remain a controversy and while many authors advocate for surgical management of patients with severe esophageal perforation, this approach is not feasible in high risk patients with multiple comorbidities.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Ciconte G, Facciorusso A S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
| 1. | January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC, Conti JB, Ellinor PT, Ezekowitz MD, Field ME. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64:e1-76. [PubMed] [DOI] [Cited in This Article: ] |
| 2. | Shah D, Dumonceau JM, Burri H, Sunthorn H, Schroft A, Gentil-Baron P, Yokoyama Y, Takahashi A. Acute pyloric spasm and gastric hypomotility: an extracardiac adverse effect of percutaneous radiofrequency ablation for atrial fibrillation. J Am Coll Cardiol. 2005;46:327-330. [PubMed] [DOI] [Cited in This Article: ] |
| 3. | Lakkireddy D, Reddy YM, Atkins D, Rajasingh J, Kanmanthareddy A, Olyaee M, Dusing R, Pimentel R, Bommana S, Dawn B. Effect of atrial fibrillation ablation on gastric motility: the atrial fibrillation gut study. Circ Arrhythm Electrophysiol. 2015;8:531-536. [PubMed] [DOI] [Cited in This Article: ] |
| 4. | Wu MH, Wongcharoen W, Tsao HM, Tai CT, Chang SL, Lin YJ, Sheu MH, Chang CY, Chen SA. Close relationship between the bronchi and pulmonary veins: implications for the prevention of atriobronchial fistula after atrial fibrillation ablation. J Cardiovasc Electrophysiol. 2007;18:1056-1059. [PubMed] [DOI] [Cited in This Article: ] |
| 5. | Sacher F, Monahan KH, Thomas SP, Davidson N, Adragao P, Sanders P, Hocini M, Takahashi Y, Rotter M, Rostock T. Phrenic nerve injury after atrial fibrillation catheter ablation: characterization and outcome in a multicenter study. J Am Coll Cardiol. 2006;47:2498-2503. [PubMed] [DOI] [Cited in This Article: ] |
| 6. | Hoffmeister PS, Chaudhry GM, Mendel J, Almasry I, Tahir S, Marchese T, Haffajee CI, Orlov MV. Evaluation of left atrial and posterior mediastinal anatomy by multidetector helical computed tomography imaging: relevance to ablation. J Interv Card Electrophysiol. 2007;18:217-223. [PubMed] [DOI] [Cited in This Article: ] |
| 7. | Lemola K, Sneider M, Desjardins B, Case I, Han J, Good E, Tamirisa K, Tsemo A, Chugh A, Bogun F. Computed tomographic analysis of the anatomy of the left atrium and the esophagus: implications for left atrial catheter ablation. Circulation. 2004;110:3655-3660. [PubMed] [DOI] [Cited in This Article: ] |
| 8. | Teplitsky L, Hegland DD, Bahnson TD. Catheter based cryoablation and radiofrequency ablation for atrial fibrillation results in conductive heat transfer from and to the esophagus. Heart Rhythm. 2006;3:S242-S242. [DOI] [Cited in This Article: ] |
| 9. | Berjano EJ, Hornero F. What affects esophageal injury during radiofrequency ablation of the left atrium? An engineering study based on finite-element analysis. Physiol Meas. 2005;26:837-848. [PubMed] [DOI] [Cited in This Article: ] |
| 10. | Ripley KL, Gage AA, Olsen DB, Van Vleet JF, Lau CP, Tse HF. Time course of esophageal lesions after catheter ablation with cryothermal and radiofrequency ablation: implication for atrio-esophageal fistula formation after catheter ablation for atrial fibrillation. J Cardiovasc Electrophysiol. 2007;18:642-646. [PubMed] [DOI] [Cited in This Article: ] |
| 11. | Doll N, Borger MA, Fabricius A, Stephan S, Gummert J, Mohr FW, Hauss J, Kottkamp H, Hindricks G. Esophageal perforation during left atrial radiofrequency ablation: Is the risk too high? J Thorac Cardiovasc Surg. 2003;125:836-842. [PubMed] [DOI] [Cited in This Article: ] |
| 12. | Ghia KK, Chugh A, Good E, Pelosi F, Jongnarangsin K, Bogun F, Morady F, Oral H. A nationwide survey on the prevalence of atrioesophageal fistula after left atrial radiofrequency catheter ablation. J Interv Card Electrophysiol. 2009;24:33-36. [PubMed] [DOI] [Cited in This Article: ] |
| 13. | Cummings JE, Schweikert RA, Saliba WI, Burkhardt JD, Kilikaslan F, Saad E, Natale A. Brief communication: atrial-esophageal fistulas after radiofrequency ablation. Ann Intern Med. 2006;144:572-574. [PubMed] [DOI] [Cited in This Article: ] |
| 14. | Dagres N, Kottkamp H, Piorkowski C, Doll N, Mohr F, Horlitz M, Kremastinos DT, Hindricks G. Rapid detection and successful treatment of esophageal perforation after radiofrequency ablation of atrial fibrillation: lessons from five cases. J Cardiovasc Electrophysiol. 2006;17:1213-1215. [PubMed] [DOI] [Cited in This Article: ] |
| 15. | Keshishian J, Young J, Hill E, Saloum Y, Brady PG. Esophageal injury following radiofrequency ablation for atrial fibrillation: injury classification. Gastroenterol Hepatol (N Y). 2012;8:411-414. [PubMed] [Cited in This Article: ] |
| 16. | Hornero F, Berjano EJ. Esophageal temperature during radiofrequency-catheter ablation of left atrium: a three-dimensional computer modeling study. J Cardiovasc Electrophysiol. 2006;17:405-410. [PubMed] [DOI] [Cited in This Article: ] |
| 17. | Zellerhoff S, Ullerich H, Lenze F, Meister T, Wasmer K, Mönnig G, Köbe J, Milberg P, Bittner A, Domschke W. Damage to the esophagus after atrial fibrillation ablation: Just the tip of the iceberg? High prevalence of mediastinal changes diagnosed by endosonography. Circ Arrhythm Electrophysiol. 2010;3:155-159. [PubMed] [DOI] [Cited in This Article: ] |
| 18. | Bahnson TD. Strategies to minimize the risk of esophageal injury during catheter ablation for atrial fibrillation. Pacing Clin Electrophysiol. 2009;32:248-260. [PubMed] [DOI] [Cited in This Article: ] |
| 19. | Nair KK, Danon A, Valaparambil A, Koruth JS, Singh SM. Atrioesophageal Fistula: A Review. J Atr Fibrillation. 2015;8:1331. [PubMed] [DOI] [Cited in This Article: ] |
| 20. | Dagres N, Anastasiou-Nana M. Prevention of atrial-esophageal fistula after catheter ablation of atrial fibrillation. Curr Opin Cardiol. 2011;26:1-5. [PubMed] [DOI] [Cited in This Article: ] |
| 21. | Singh SM, d’Avila A, Doshi SK, Brugge WR, Bedford RA, Mela T, Ruskin JN, Reddy VY. Esophageal injury and temperature monitoring during atrial fibrillation ablation. Circ Arrhythm Electrophysiol. 2008;1:162-168. [PubMed] [DOI] [Cited in This Article: ] |
| 22. | Halm U, Gaspar T, Zachäus M, Sack S, Arya A, Piorkowski C, Knigge I, Hindricks G, Husser D. Thermal esophageal lesions after radiofrequency catheter ablation of left atrial arrhythmias. Am J Gastroenterol. 2010;105:551-556. [PubMed] [DOI] [Cited in This Article: ] |
| 23. | Schmidt M, Nölker G, Marschang H, Gutleben KJ, Schibgilla V, Rittger H, Sinha AM, Ritscher G, Mayer D, Brachmann J. Incidence of oesophageal wall injury post-pulmonary vein antrum isolation for treatment of patients with atrial fibrillation. Europace. 2008;10:205-209. [PubMed] [DOI] [Cited in This Article: ] |
| 24. | Kiev J, Amendola M, Bouhaidar D, Sandhu BS, Zhao X, Maher J. A management algorithm for esophageal perforation. Am J Surg. 2007;194:103-106. [PubMed] [DOI] [Cited in This Article: ] |
| 25. | Brewer LA, Carter R, Mulder GA, Stiles QR. Options in the management of perforations of the esophagus. Am J Surg. 1986;152:62-69. [PubMed] [DOI] [Cited in This Article: ] |
| 26. | Shaffer HA, Valenzuela G, Mittal RK. Esophageal perforation. A reassessment of the criteria for choosing medical or surgical therapy. Arch Intern Med. 1992;152:757-761. [PubMed] [DOI] [Cited in This Article: ] |
| 27. | Lyons WS, Seremetis MG, deGuzman VC, Peabody JW. Ruptures and perforations of the esophagus: the case for conservative supportive management. Ann Thorac Surg. 1978;25:346-350. [PubMed] [DOI] [Cited in This Article: ] |
| 28. | Sabanathan S, Eng J, Richardson J. Surgical management of intrathoracic oesophageal rupture. Br J Surg. 1994;81:863-865. [PubMed] [DOI] [Cited in This Article: ] |
| 29. | Cameron JL, Kieffer RF, Hendrix TR, Mehigan DG, Baker RR. Selective nonoperative management of contained intrathoracic esophageal disruptions. Ann Thorac Surg. 1979;27:404-408. [PubMed] [DOI] [Cited in This Article: ] |
| 30. | Madanick RD. Medical management of iatrogenic esophageal perforations. Curr Treat Options Gastroenterol. 2008;11:54-63. [PubMed] [DOI] [Cited in This Article: ] |
| 31. | Sepesi B, Raymond DP, Peters JH. Esophageal perforation: surgical, endoscopic and medical management strategies. Curr Opin Gastroenterol. 2010;26:379-383. [PubMed] [DOI] [Cited in This Article: ] |