Published online Aug 28, 2016. doi: 10.3748/wjg.v22.i32.7275
Peer-review started: April 5, 2016
First decision: May 12, 2016
Revised: June 20, 2016
Accepted: July 21, 2016
Article in press: July 21, 2016
Published online: August 28, 2016
Processing time: 147 Days and 17.3 Hours
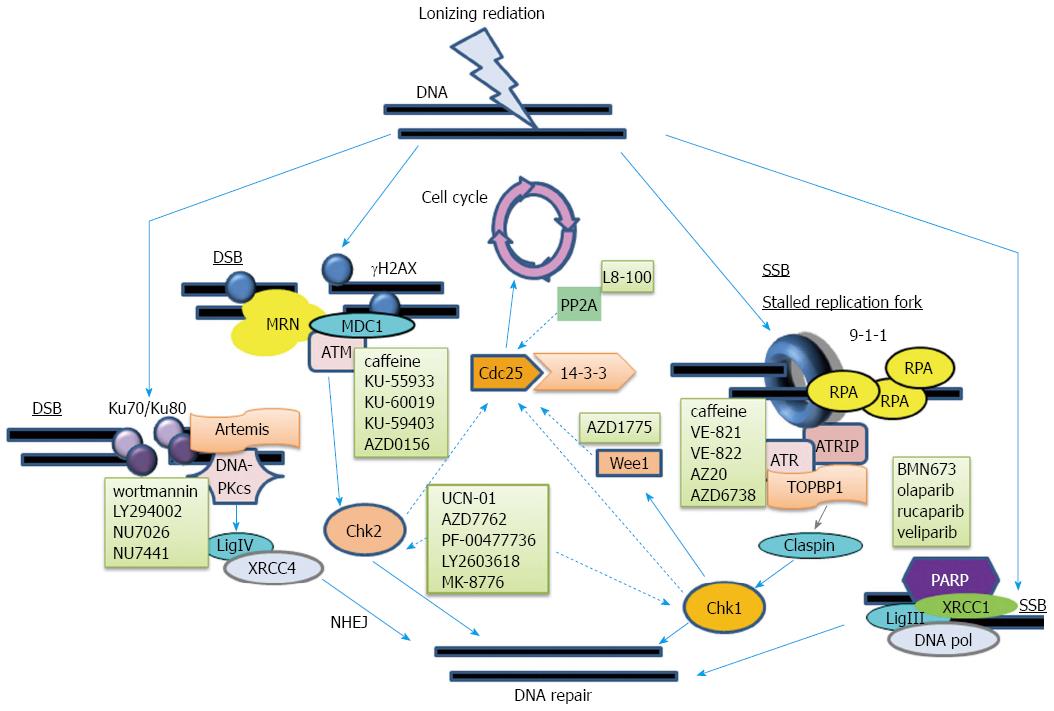
Pancreatic cancer is highly lethal. Current research that combines radiation with targeted therapy may dramatically improve prognosis. Cancerous cells are characterized by unstable genomes and activation of DNA repair pathways, which are indicated by increased phosphorylation of numerous factors, including H2AX, ATM, ATR, Chk1, Chk2, DNA-PKcs, Rad51, and Ku70/Ku80 heterodimers. Radiotherapy causes DNA damage. Cancer cells can be made more sensitive to the effects of radiation (radiosensitization) through inhibition of DNA repair pathways. The synergistic effects, of two or more combined non-lethal treatments, led to co-administration of chemotherapy and radiosensitization in BRCA-defective cells and patients, with promising results. ATM/Chk2 and ATR/Chk1 pathways are principal regulators of cell cycle arrest, following DNA double-strand or single-strand breaks. DNA double-stranded breaks activate DNA-dependent protein kinase, catalytic subunit (DNA-PKcs). It forms a holoenzyme with Ku70/Ku80 heterodimers, called DNA-PK, which catalyzes the joining of nonhomologous ends. This is the primary repair pathway utilized in human cells after exposure to ionizing radiation. Radiosensitization, induced by inhibitors of ATM, ATR, Chk1, Chk2, Wee1, PP2A, or DNA-PK, has been demonstrated in preclinical pancreatic cancer studies. Clinical trials are underway. Development of agents that inhibit DNA repair pathways to be clinically used in combination with radiotherapy is warranted for the treatment of pancreatic cancer.
Core tip: Radiotherapy causes DNA damage, including double-strand breaks, which is more readily repaired in normal cells than in cancerous cells. Radiosensitization, using DNA repair pathway inhibitors, has been well documented in various cancer types, including pancreatic cancer. Further development of optimal protocols, for the combined use of these inhibitors with radiotherapy, with/without chemotherapy, is warranted for the clinical treatment of pancreatic cancer.
- Citation: Yang SH, Kuo TC, Wu H, Guo JC, Hsu C, Hsu CH, Tien YW, Yeh KH, Cheng AL, Kuo SH. Perspectives on the combination of radiotherapy and targeted therapy with DNA repair inhibitors in the treatment of pancreatic cancer. World J Gastroenterol 2016; 22(32): 7275-7288
- URL: https://www.wjgnet.com/1007-9327/full/v22/i32/7275.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i32.7275
Pancreatic cancer is not a common disease; there are approximately 330000 cases a year worldwide. However, it is highly lethal, with nearly equal numbers of new cases and deaths. The majority (> 80%) of pancreatic cancers are ductal adenocarcinoma, for which the prognosis remains poor, even with recent advances in detection, supportive care, and therapeutics[1]. It remains challenging to make an early diagnosis for sporadic pancreatic cancer, because of the low lifetime risk of developing pancreatic cancer and the lack of adequate screening methods[2]. Endoscopic ultrasonography and MRI screening tools may play a limited detection role in patients with high risks, such as family history or known germline mutations[3,4].
Only 20% of pancreatic cancer patients are good candidates for curative resection at diagnosis. The 5-year survival rate doubled from 10.4% to 20.7%, after 6-mo of treatment with adjuvant gemcitabine, in the CONKO-001 study[5]. This randomized trial revealed that application of adjuvant gemcitabine significantly improved median disease-free survival (13.4 mo vs 6.9 mo), compared with that by surgery alone[6]. However, at least 50% of the patients eventually developed distant metastases[6]. Systemic dissemination occurs early in the disease process, in a mouse model of pancreatic cancer[7]. Clinical trials, in the past decade, have attempted to administer modern adjuvant radiotherapy, alone or combined with chemotherapy, to decrease the local recurrence and eventual metastasis that remain significant issues for operable pancreatic cancer[6]. However, the local recurrence rate is still more than 30%[8]. In addition, the survival benefit with adjuvant radiotherapy is controversial and may be outweighed by the toxicity of the treatments[9].
Patients with advanced pancreatic cancer frequently suffer from local symptoms. Local control of the main tumor is paramount to palliate these complaints, in addition to surgical bypass, and biliary/intestinal stenting or drainage[10]. The local control rate with chemotherapy alone varies over a wide range, which is probably due to the use of a single agent versus combined chemotherapy[10,11]. It is questionable if local control can translate into a survival benefit. Bolus 5-FU-based chemoradiotherapy (CCRT) concurrent with maintenance chemotherapy was shown, in the 1980s, to double overall survival from 22.9 wk to more than 40 wk compared to that by radiotherapy alone[12]. However, a comparison of CCRT to chemotherapy alone did not show a consistent survival benefit[13,14]. Moreover, the use of modern radiotherapy techniques, to obtain a survival benefit in locally advanced pancreatic cancer, is of great debate[10,15,16].
The underlying reasons for inconsistent benefits in adding radiotherapy to chemotherapy, in the adjuvant or palliative setting, are multifactorial. Potential explanations are poor quality control of the delivery of radiotherapy, the use of old techniques with high radiation-induced toxicity, breaks with divided radiotherapy courses, and the use of agents with poor radiosensitization and high toxicity. However, pancreatic cancer metastasizes early[7]. The choice of the most appropriate medicine added to the radiotherapy, rather than radiotherapy itself, may be the most important answer. The most common current daily practice combines radiosensitizing agents, 5-FU and gemcitabine, with radiotherapy in the adjuvant or advanced setting. However, the single-agent activity of gemcitabine or 5-FU in advanced disease is poor[17]. In addition, significant toxicities of CCRT are always of concern[9]. The aim of this review is to present an overview of the types of DNA damage in pancreatic cancer, summarize new evidence in non-chemotherapy agents, with the focus on DNA repair-related targeted therapy (Table 1). Additionally, we will provide direction for further development of use of these agents combined with radiotherapy in pancreatic cancer.
| Compound | Target | RT | Clinical trial |
| Rucaparib | PARP | - | A Study of Rucaparib in Patients With Pancreatic Cancer and a Known Deleterious BRCA Mutation (NCT02042378) |
| Olaparib (AZD2281) | PARP | - | Ph II Olaparib for BRCAness Phenotype in Pancreatic Cancer (NCT02677038) |
| Olaparib in gBRCA Mutated Pancreatic Cancer Whose Disease Has Not Progressed on First Line Platinum-Based Chemotherapy (POLO)(NCT02184195) | |||
| Trial of ICM With or Without AZD2281 (Olaparib) in Patients With Advanced Pancreatic Cancer (NCT01296763) | |||
| Efficacy and Safety of PARPi to Treat Pancreatic Cancer (NCT02511223) | |||
| Study to Assess the Safety and Tolerability of a PARP Inhibitor in Combination With Gemcitabine in Pancreatic Cancer (NCT00515866) | |||
| + | Olaparib Dose Escalating Trial + Concurrent RT With or Without Cisplatin in Locally Advanced NSCLC (olaparib) (NCT01562210) Olaparib and Radiotherapy in Inoperable Breast Cancer (NCT02227082) | ||
| Olaparib and Radiotherapy in Head and Neck Cancer (NCT02229656) | |||
| Phase I Study of Olaparib Combined With Cisplatin-based Chemoradiotherapy to Treat Locally Advanced Head and Neck Cancer (ORCA-2) (NCT02308072) | |||
| BMN673 (Tazaloparib) | PARP | - | Study of Talazoparib, a PARP Inhibitor, in Patients With Advanced or Recurrent Solid Tumors |
| (NCT01286987) | |||
| Veliparib (ABT-888) | PARP | - | Gemcitabine Hydrochloride and Cisplatin With or Without Veliparib or Veliparib Alone in Treating Patients With Locally Advanced or Metastatic Pancreatic Cancer (NCT01585805) |
| Veliparib, Oxaliplatin, and Capecitabine in Treating Patients With Advanced Solid Tumors (NCT01233505) | |||
| Veliparib, Cisplatin, and Gemcitabine Hydrochloride in Treating Patients With Advanced Biliary, Pancreatic, Urothelial, or Non-Small Cell Lung Cancer (NCT01282333) | |||
| Veliparib in Treating Patients With Malignant Solid Tumors That Did Not Respond to Previous Therapy (NCT00892736) | |||
| Veliparib and Irinotecan Hydrochloride in Treating Patients With Cancer That Is Metastatic or Cannot Be Removed by Surgery (NCT00576654) | |||
| ABT-888 With Modified FOLFOX6 in Patients With Metastatic Pancreatic Cancer (NCT01489865) | |||
| + | A Phase I Study of Veliparib (ABT-888) in Combination With Gemcitabine and Intensity Modulated Radiation Therapy in Patients With Locally Advanced, Unresectable Pancreatic Cancer (VelGemRad) (NCT01908478) | ||
| A Study Evaluating the Efficacy and Tolerability of Veliparib in Combination With Paclitaxel/Carboplatin-Based Chemoradiotherapy Followed by Veliparib and Paclitaxel/Carboplatin Consolidation in Subjects With Stage III Non-Small Cell Lung Cancer (NCT02412371) | |||
| Veliparib With or Without Radiation Therapy, Carboplatin, and Paclitaxel in Patients With Stage III Non-small Cell Lung Cancer That Cannot Be Removed by Surgery (NCT01386385) | |||
| A Clinical Study Conducted in Multiple Centers Comparing Veliparib and Whole Brain Radiation Therapy (WBRT) Versus Placebo and WBRT in Subjects With Brain Metastases From Non Small Cell Lung Cancer (NSCLC) (NCT01657799) | |||
| A Phase I Study of ABT-888 in Combination With Conventional Whole Brain Radiation Therapy (WBRT) in Cancer Patients With Brain Metastases (NCT00649207) | |||
| ABT-888, Radiation Therapy, and Temozolomide in Treating Patients With Newly Diagnosed Glioblastoma Multiforme (NCT00770471) | |||
| Pre-Operative Radiation and Veliparib for Breast Cancer (NCT01618357) | |||
| Iniparib (BSI-201) | PARP | + | A Trial Evaluating Concurrent Whole Brain Radiotherapy and Iniparib in Multiple Non Operable Brain Metastases (RAPIBE) (NCT01551680) |
| VX-970 (VE-822) | ATR | + | VX-970, Cisplatin, and Radiation Therapy in Treating Patients With Locally Advanced HPV-Negative Head and Neck Squamous Cell Carcinoma (NCT02567422) |
| VX-970 and Whole Brain Radiation Therapy in Treating Patients With Brain Metastases From Non-Small Cell Lung Cancer (NCT02589522) | |||
| AZD6738 | ATR | +/- | Phase I Study to Assess Safety of AZD6738 Alone and in Combination With Radiotherapy in Patients With Solid Tumours (Patriot) (NCT02223923) |
| UCN-01 | Chk1 | - | UCN-01 and Gemcitabine in Treating Patients With Unresectable or Metastatic Pancreatic Cancer (NCT00039403) |
| UCN-01 and Fluorouracil in Treating Patients With Metastatic Pancreatic Cancer (NCT00045747) | |||
| 7-Hydroxystaurosporine and Irinotecan Hydrochloride in Treating Patients With Metastatic or Unresectable Solid Tumors or Triple Negative Breast Cancer (NCT00031681) | |||
| LY2603618 | Chk1 | - | A Study for Patients With Pancreatic Cancer (NCT00839332) |
| MK-1775 (AZD1775) | Wee1 | - | Paclitaxel Albumin-Stabilized Nanoparticle Formulation and Gemcitabine Hydrochloride With or Without WEE1 Inhibitor MK-1775 in Treating Patients With Previously Untreated Pancreatic Cancer That Is Metastatic or Cannot Be Removed by Surgery (NCT02194829) |
| + | Dose Escalation Trial of MK1775 and Gemcitabine (+Radiation) for Unresectable Adenocarcinoma of the Pancreas (NCT02037230) | ||
| LB-100 | PP2A | - | Phase I Study of LB-100 With Docetaxel in Solid Tumors (NCT01837667) |
| MSC2490484A | DNA-PK | + | Phase 1 Trial of MSC2490484A, an Inhibitor of a DNA-dependent Protein Kinase, in Combination With Radiotherapy (NCT02516813) |
Radiotherapy has a local therapeutic role for pancreatic cancer, however, it is much less frequently used than systemic therapy[18,19]. The theoretical mechanism of cytotoxicity, induced directly or indirectly by radiotherapy, is DNA damage, regardless of whether it is caused by photons, charged particles with protons or carbon ions, or any emerging technique. The types of DNA damage induced by ionizing radiation (IR) include single-strand break (SSB), double-strand break (DSB), base modifications, and DNA-protein cross-linking. The damage can be repaired, in normal mammalian cells, through several mechanisms. The repair mechanism can be homologous recombination (HR), nonhomologous end joining (NHEJ), nucleotide excision repair (NER), base excision repair (BER), and mismatch repair (MMR), regardless of whether the damage was induced by IR or occurred spontaneously (Figure 1).
The pancreatic cancer genome is unstable. Telomere shortening was obvious in pancreatic intraepithelial neoplasia (PanIN) lesions, even in the earliest PanIN-1A lesions. However, this phenomenon was not found in atrophic or inflammatory pancreatic lesions[20]. The telomeres were much shorter in cancer cells than in PanIN-1 or PanIN-2 lesions[21]. The activation of telomeres expression seen in the majority of pancreatic cancers may be resulted from the protective mechanism of telomeres against catastrophic DNA damage[22]. Previous studies also demonstrated that telomere shortening was closely associated with the DNA repair impairment[23,24]. In addition, widespread DNA damage was found in PanIN lesions. Increased γH2AXSer139, phospho-ataxia-telangiectasia mutated (ATM)Ser1981, and phospho-cell cycle checkpoint kinase 2 (Chk2)Thr68 signals were noted in PanIN lesions, compared to that in the normal pancreatic epithelium[25]. Intraductal papillary mucinous neoplasm, another type of pancreatic cancer precursor, was also shown to have an increased phospho-Chk2Thr68 nuclear signal, compared to that in the normal pancreatic epithelium[26]. γH2AXSer139, phospho-ATMSer1981, phospho-Chk1Ser345, phospho-Chk2Thr68, phospho-DNA-PKcsSer2056, Rad51, and Ku70 expression levels are increased in invasive pancreatic cancer tissues compared to that in normal pancreatic tissues[27]. Therefore, DNA damage lesions, induced by exogenous or endogenous reagents, must accumulate early in the carcinogenic process. These lesions induce universal activation of DNA damage responses; however, the repair machinery does not work perfectly and may itself be the victim of mutation. This hypothesis is supported by the observation that some familial pancreatic cancers are associated with genetic defects in DNA damage responses and repair machinery, such as TP53, BRCA2, ATM, PALB2, and MMR-related genes (e.g., hMLH1, hMSH2, and hMSH6)[28].
Notably, a recent study, which applied whole-genome sequencing and copy number variation analysis, demonstrated that four subtypes of structural variation could be identified in pancreatic cancer[29]. Among them, the “unstable” subtype was characteristic of defects in genomic stability with considerable structural variations. Ten of 14 patients in this subgroup were in the top quintile of the BRCA signature, with deleterious mutations in BRCA1, BRCA2, or PALB2 genes. Most importantly, five patients in this subtype responded very well to platinum-based therapy[29]. In fact, the DNA repair mechanisms implicated in platinum or IR treatment are overlapping, including DSB repair, SSB repair, NER, BER, and MMR. This study provides a strong rationale for radiosensitization, using agents to inhibit the DNA repair machinery in pancreatic cancer cells treated with IR, so that lethal DNA lesions will go unrepaired. We present a comprehensive review of the mechanism and clinical histories of these agents.
Poly (ADP-ribose) polymerases (PARPs) are nuclear proteins that play important roles in SSB repair. DNA breaks induce PARP to bind to the lesions, through its N-terminal zinc finger motifs, which causes massive ADP-ribose polymerization. PARP hydrolyzes nicotinamide adenine dinucleotide to generate ADP-ribose units. It covalently adds the units to the side chains of aspartate, arginine, lysine, and glutamate amino acids on the surfaces of nearby protein substrates and PARP itself. Then, DNA repair machinery, which has a high affinity for ADP-ribose polymers, is recruited to the DNA nicks and performs DNA repair[30]. Preclinical and clinical studies demonstrated that cancers, with mutated BRCA1 and/or BRCA2, were highly sensitive to PARP inhibitors[31-37]; this confirms the “synthetic lethal” hypothesis[38]. BRCA1 binds to CtBP-interacting protein and the MRE11-RAD50-NBS1 (MRN) complex, when double strand DNA breaks occur. This forms a functional unit that senses and resects the damaged DNA. Then, BRCA1, BRCA2, and PALB2 mediate RAD51 recombinase-dependent HR[39]. However, cancer cells with defective BRCA1, BRCA2, or PALB2 have high genomic instability[29]. Therefore, these HR-defective cancer cells are vulnerable to PARP inhibitors that interfere with SSB repair. They suffer from error-prone DNA repair, cell cycle arrest, and ultimately cell death.
Pancreatic cancer, with defective HR, is highly sensitive to PARP inhibitors[34,37,40-42]. Capan-1, a prototypical pancreatic cancer cell line with defective BRCA2 (6174delT), has in vitro sensitivity to molecular targeted agents, including rucaparib, olaparib, and BMN 673[37,40,41]. Increased formation of nuclear γH2AX foci was found[37,41] after treatment of Capan-1 with rucaparib or BMN 673, which indicated an increased number of DNA breaks. In contrast, nuclear RAD51 foci did not increase[37,41]. A study, in the xenograft model of Capan-1, combined rucaparib with carboplatin, a DNA-damaging agent. The results showed better efficacy than that observed with either agent alone[37]. A patient-derived xenograft model, with mutated BRCA2, received BMN 673 treatment, which decreased cancer cell mitosis and increased cell apoptosis[41]. A phase II clinical trial of olaparib enrolling 23 pancreatic cancer patients with germline BRCA1/2 mutations, who were heavily pretreated; the response rate and stable disease were 21.7% and 35%, respectively[34]. Hematological toxicities became a matter of concern, in a phase II study that had enrolled patients without enrichment of BRCA mutations, despite clinical responses to the combination of gemcitabine and olaparib that seemed to be promising[43].
IR can induce SSB and DSB and may be synergistic with PARP inhibitors, especially in cancer cells with defective DNA repair abilities[44]. In fact, preclinical studies demonstrated that PARP inhibitors had radiosensitizing effects in various cancer types[37,45-52], including pancreatic cancer[53-57], regardless of the DNA repair machinery integrity. Increased apoptosis and DNA breaks, accompanied by decreased proliferation of cancer cells, were observed in a lung cancer model using veliparib[45]. Importantly, veliparib caused comparable radiosensitization in oxic and hypoxic conditions[46]. Diminished angiogenesis was also observed in the lung cancer model that used veliparib[45]; however, increased vascular perfusion was noted in another lung cancer model using olaparib[52]. The discrepancy, in the effects of different PARP inhibitors on blood vessels, may be an epiphenomenon that is not truly associated with radiosensitization.
A synergistic effect was also shown when MiaPaCa-2, a BRCA-intact pancreatic cancer cell line, was treated with IR, veliparib, or both. The combination increased apoptosis in vitro and inhibited tumor growth in an animal model compared to that by either treatment alone[56]. S phase arrest and then G2/M arrest were induced in MiaPaCa-2, by combining olaparib with either γ-irradiation or carbon-ion irradiation[54]. Rad51 foci were increased after rucaparib, IR, or combined treatment, which indicated the presence of functional HR[55]. Rucaparib induced more γH2AX foci in Capan-1 than in MiaPaCa-2; however, the magnitude of γH2AX foci induction after IR, or IR combined with rucaparib, was similar in the two cell lines[55]. Differences in DNA repair machinery, other than PARP-related SSB repair and BER, between Capan-1 and MiaPaCa-2 may partially explain the finding.
Gemcitabine, oxaliplatin, irinotecan, and 5-FU are all radiosensitizing agents and are current standards for advanced pancreatic cancer[11,17]. Platinum drugs, such as cisplatin, oxaliplatin, and carboplatin, have the potential to enhance the radiosensitizing effects of PARP inhibitors in patients with defective HR[29]. Synergistic effects between PARP inhibitors and oxaliplatin have been observed already in colon cancer models[58,59]. In addition, IR combined with oxaliplatin and veliparib showed further enhanced synergistic effects in vitro and in vivo[59]. Chemoradiosensitization with PARP inhibitors was also noted with irinotecan[48,59], 5-FU[59], and gemcitabine[55], in different cancer models. However, the underlying mechanisms for these agents are not clear.
Increased ATM activation was observed in premalignant and invasive lesions of pancreatic cancer[25,27]. In addition, oncogenic Ras can lead to increased oxidative DNA damage[60] and DNA replication stress-induced DNA damage. It eventually activates ataxia-telangiectasia and Rad3-related (ATR)/Chk1-related DDR[61,62]. ATM and ATR belong to the phosphatidylinositol 3-kinase-related kinase (PIKK) family of serine/threonine protein kinases; they share a number of substrates. The MRN complex is recruited upon DNA DSB, induced by IR, chemicals, or endogenous processes. It processes damaged DNA ends and initiates NHEJ through all cell cycle phases or HR in late S/G2 phase only[63]. The MRN complex aids the conversion of inactive ATM homodimers to active monomers, after autophosphorylation at serine1981[64,65]. Then, ATM and DNA-PK phosphorylate H2AX at serine139, which forms γH2AX at sites close to the DNA DSB[66,67]. The association of the MRN complex, MDC1, and γH2AX enhances the accumulation of phosphorylated ATM and further phosphorylation of H2AX at DNA DSB sites[68]. Next, the DSB repair machinery is recruited and p53 and Chk2 are phosphorylated[69-71]. The replication protein A (RPA) coated ssDNA structure recruits ATR and ATR-interacting protein (ATRIP) to bind with RPA, at sites of damaged DNA or stalled replication forks[72,73]. The RAD9-HUS1-RAD1 (9-1-1) clamp complex[74] localizes to the damaged DNA sites, with the aid of RAD17 clamp loader. This event brings the ATR/ATRIP complex activator topoisomerase-binding protein-1 (TOPBP1) to the complex[75]. This step is essential for ATR/ATRIP activation and further signaling. Claspin functions as the adaptor that brings Chk1 to the ATR/ATRIP complex[76]. Phosphorylation of the ATRIP, 9-1-1 complex, TOPBP1, the minichromosome maintenance protein (MCM) complex, and RPA also follow ATR activation.
Inhibitors of ATM or ATR are under active development for the treatment of various cancer types. Caffeine, a methylxanthine alkaloid, inhibited the kinase activities of ATM and ATR with an IC50 in millimolar ranges. It subsequently induced Ser15 phosphorylation of p53, 2 effects that can contribute to radiosensitization[77]. Notably, caffeine also induced radiosensitization in p53-deficient cells, through the activation of Cdk1[78]. However, the clinical use of caffeine as a radiosensitizer is limited, due to its low serum level and high systemic toxicity. KU-55933, the first potent and selective ATM inhibitor, was shown to induce radiosensitization and inhibit IR-induced ATM-mediated phosphorylation of p53, H2AX, and Chk1. However, the radiosensitizing dose of KU-55933 was much higher than the dose required to inhibit ATM[79]. KU-60019, an analog of KU-55933 with better pharmacokinetics, bioavailability, and selective potency for ATM, had a higher radiation dose to enhancement ratio in glioma cells than KU-55933 did. The radiosensitizing effect of KU-55933 was attributed to the indirect inhibition of AKT phosphorylation[80]; the aforementioned effect was more pronounced in xenograft tumors with mutant p53[81]. However, the oral bioavailability of KU-60019 was still poor[81]. KU59403, another analog of KU-55933 with higher potency and oral bioavailability had plasma and intra-tumor concentrations in therapeutic ranges in the xenograft model compared with those of KU-55933. However, its radiosensitizing effects were not addressed[82]. A few ATM inhibitors are entering clinical trials; an example is a phase I trial for AZD0156 (ClinicalTrials.gov: NCT02588105), which was developed by AstraZeneca.
Unlike ATM, the loss of ATR results in early embryonic lethality. ATR is essential for proliferating cells to ensure proper DNA replication and genomic integrity. Schisandrin B, a herbal ingredient isolated from Fructus schisandrae, is the first selective ATR inhibitor with an IC50 in the micromolar range. Schisandrin B inhibited phosphorylation of p53 and Chk1 following UV irradiation; thereby, providing radiosensitization in A549 lung adenocarcinoma cells[83]. VE-821, developed by Vertex Pharmaceuticals, was the first selective and potent ATR inhibitor[84]. It conferred radiosensitization among all 12 cell lines that were tested. Notably, it could induce radiosensitization and reduce Chk1 phosphorylation in hypoxic conditions[85]. Radiosensitization was observed, in pancreatic cancer cell lines with defective p53, when VE-821 was used concurrently with IR or 24 h after IR; it occurred under normoxic and hypoxic conditions. G2/M phase was delayed and reduced in this study, which indicated that IR-induced checkpoint activation was inhibited by VE-821[86]. Foci of 53BP1 and γH2AX increased following IR and VE-821 treatment. Interestingly, Rad51 foci were reduced, which suggested inhibition of HR repair[86]. VE-822, also known as VX-970, is an analog of VE-821. It is the first selective ATR inhibitor to enter clinical trials. In a pancreatic cancer cell line model, VE-822 induced radiosensitization, by downregulating Chk1 phosphorylation and Rad51 foci and upregulating 53BP1 and γH2AX foci[87]. VE-822 did not have an antitumor effect in vivo; however, it enhanced the efficacy of IR, without significant weight loss in animals[87]. Moreover, tumor growth delay was more significant with gemcitabine-VE-822 plus IR, compared with that by either agent used singly with IR[87]. AZD6738, derived from ATR and mTOR inhibitor AZ20[88], is an orally available, selective, and potent ATR inhibitor; it is under phase I clinical trial development in combination with radiotherapy (ClinicalTrials.gov: NCT02223923). AZD6738 was shown to inhibit Chk1 phosphorylation and in vitro and in vivo radiosensitization[89].
Chk1 and Chk2 are functionally overlapping serine/threonine protein kinases. Chk1 or Chk2, activated by phosphorylation (Ser317 and Ser345 on Chk1, Thr68 on Chk2), binds to, and phosphorylates Cdc25 phosphatases. Then, 14-3-3 proteins bind to, sequester, and inhibit Cdc25 phosphatases[90,91]. In addition, Chk1 activates (never in mitosis gene A)-related kinase-11 (Nek11), which phosphorylates Cdc25A and mediates its polyubiquitination and degradation[92]. Human cells have 3 isoforms of Cdc25, all of which can dephosphorylate and activate Cdks. Cdc25s are rapidly degraded when DNA is damaged and the activities of Cdk1 and Cdk2 are inhibited; this results in cell cycle arrest[93].
UCN-01 (7-hydroxystaurosporine) is the first Chk1 inhibitor that has a non-specific inhibitory spectrum, low volumes of distribution, and systemic clearance. Unexpectedly, UCN-01 strongly binds to α1-acid glycoprotein[94]. The long half-life, decreased bioavailability, and pharmacokinetics that are highly variable among patients, may be attributed to α1-acid glycoprotein; this precluded UCN-01 from more advanced clinical development[95]. In addition, the activity of UCN-01 in pancreatic cancer was poor[96]. AZD7762, an ATP competitive and non-selective inhibitor of Chk1 and Chk2, was shown to have in vitro and in vivo chemosensitization, through stabilization of Cdc25A, following gemcitabine treatment[97]. IR plus AZD7762, in the HT-29 colon cancer cell model, delayed tumor growth more than IR alone, due to impairment of DNA repair by AZD7762[98]. AZD7762 showed better radiosensitization, with or without concurrent treatment with olaparib, in pancreatic cell lines with defective P53, including MiaPaCa-2[53]. A combination of IR and AZD7762, in the same model, resulted in Ser345 phosphorylation of Chk1, Cdc25A stabilization, decreased Rad51 foci, and delayed in vivo tumor growth[99]. However, cardiac toxicities, including increased troponin I, myocardial ischemia, abnormal electrocardiogram, and decreased ejection fraction, precluded AZD7762 from further clinical development[100,101].
PF-00477736, a selective and potent ATP competitive Chk1 inhibitor, was shown to inhibit Chk2. It abrogated gemcitabine-induced S-phase arrest, increased γH2AX expression, and induced apoptosis in a HT-29 cell line[102]. In addition, the sequential administration of gemcitabine and PF-00477736, in an in vivo model, resulted in more inhibition of tumor growth than gemcitabine alone[103]. Remarkably, three-component chemoradiation, with PF-00477736, gemcitabine, and Lutetium-177 Lu–labeled anti-EGFR antibody, completely eradicated pancreatic cancer xenografts[102]. However, the phase I clinical trial was prematurely terminated, because of business-related reasons (ClinicalTrials.gov: NCT00437203).
LY2603618 and MK-8776 (SCH 900776) are other Chk1 and/or Chk2 inhibitors entering clinical trials. Studies showed that both agents cause chemosensitization with gemcitabine[104-106]. Expanded studies showed that a combination of MK-8776, gemcitabine, and radiotherapy was the most promising treatment for inhibition of tumor growth, in animal models of pancreatic cancer[105]. The most common grade 3 or more toxicity, encountered with the use of gemcitabine or LY2603618, was hematological[107]. Grade 3 or higher hematological toxicities and fatigue were the most common negative effects in response to gemcitabine and MK-8776 treatment; however, such occurrences were rare with MK-8776 alone[108]. A variety of Chk1 and/or Chk2 inhibitors are under active preclinical development, including EXEL-9844 (also called XL-844), CEP-3891, PD-321852, Chir-124, CCT241533, LY2606368, CCT245737, SAR-020106, and GNE-900[109-118].
Chk1 activates Wee1 kinase1 at the G2-M checkpoint, upon DNA damage. Activated Wee1 phosphorylates CDC2 (Cdk1)Tyr15, which enables CDC2/Cdk1 inactivation; this process contributes to G2-M arrest[119]. At the same time, activated Chk1 phosphorylates and inactivates Cdc25 to prevent the dephosphorylation and inactivation of CDC2/Cdk1. In contrast, protein phosphatase 2A (PP2A) is able to dephosphorylate and inhibit Cdc25, through 14-3-3 protein[120]. Therefore, inhibitors of Wee1 or PP2A can be used to maintain the activity of Cdc25; thus, they theoretically allow cell cycle progression, without adequate time for DNA repair.
In vitro studies, in p53-defective MCF-7 cancer cells derived from breast cancer cell lines, showed that compared to p53-intact cells, these cells were much more sensitive to Wee1 inhibition by MK-1775 (AZD1775)[121]. In addition, radiosensitization was observed in the p53-defective MCF-7 cells in a clonogenic assay. Cells pretreated with MK-1775 (AZD1775) had a reduction in Cdk1Tyr15 phosphorylation and 53BP1 foci; however, they had an increase in γ-H2AX after IR[121]. The defective DNA repair was through inhibition of HR, but not NHEJ[121]. MK-1775 (AZD1775) monotherapy, in patient-derived pancreatic cancer xenografts, was ineffective[122]. However, a combination of gemcitabine and MK-1775 (AZD1775) abrogated G2-M checkpoint arrest, which was accompanied by pancreatic tumor regression, increased mitotic entry and apoptosis in pancreatic cancer cells[122]. MK-1775 (AZD1775) increased gemcitabine-induced radiosensitization, in MiaPaCa-2 pancreatic cancer cell lines, through inhibition of Cdk1Tyr15 phosphorylation and upregulation of γ-H2AX expression[123]. However, the radiosensitization phenomenon was not observed in HR and BRCA2-defective Capan-1 cells. A combination of AZD1775, gemcitabine, and radiotherapy enhanced a delay in tumor growth and impaired RAD51 focus formation, in xenografts derived from patients with pancreatic cancer[124]. In fact, MK-1775 (AZD1775) is the first-in-class Wee1 inhibitor, with high specificity and potency, to enter clinical trial development. A phase I study, which used single agent MK-1775 (AZD1775) to treat refractory solid tumors, had activities in patients with a BRCA mutation; however, myelosuppression and supraventricular tachycardia were dose-limiting toxicities[124]. Clinical trials combining MK-1775 (AZD1775) and radiotherapy in various cancer types are underway.
Knockdown of the PP2A and PPP2R1A subunit, in MiaPaCa-2 and Panc-1 cell lines, resulted in significant radiosensitization and persistent γ-H2AX expression. The main mechanisms, of radiosensitization by PP2A inhibition, are through the activation of CDC25C/Cdk1Tyr15 and inhibition of HR[125]. The aforementioned phenomenon was reproduced using the PP2A inhibitor, LB-100, which increased CDC25CThr130, but decreased Cdk1Tyr15 phosphorylation[126]. The synergistic effects of LB-100 and radiotherapy on delayed tumor growth were also observed in the MiaPaCa-2 xenograft model[126]. At present, a phase I clinical trial, in which LB-100 is administered alone or in combination with docetaxel, is ongoing. Initial outcomes show that one patient, with stage IV disease, had a long, stable disease[125].
A member of the PIKK family of serine/threonine protein kinases, along with ATM and ATR, DNA-PK, is essential for NHEJ, the major repair mechanism for IR-induced DSB in human cells. A catalytic subunit, DNA-PKcs, and a regulatory heterodimer (Ku70 and Ku80 subunits) combine to form active DNA-PK, which is an ATM and ATR target. It can phosphorylate Ku70/Ku80, RPA, γH2AX, Chk2, Artemis, DNA ligase IV, XRCC4, p53, and itself. The Ku heterodimer binds to the ends of dsDNA, which become available because of DNA DSB, and recruits DNA-PKcs[127]. DNA ligase IV and XRCC4 are recruited to join the DNA ends, after the blunt DNA ends are processed and in place[120].
Wortmannin is the first identified DNA-PK inhibitor; it is equipotent to PI3K, therefore, it is non-selective. Radiosensitization has been observed with Wortmannin[128]; however, its lack of specificity and in vivo toxicity precluded its clinical use. Another radiosensitizer[129], LY294002 (structurally unrelated to Wortmannin), is a reversible kinase domain inhibitor with non-selective in vivo toxicity. Repair of IR-induced DNA DSB, in pancreatic cancer cell lines, was delayed by Wortmannin. Its effect was comparable between cell lines, with or without defective BRCA2, which indicated that NHEJ, but not HR, was successfully inhibited[130]. Wortmannin and LY294002 have demonstrated activities, as single agents, in a pancreatic cancer cell line. In addition, chemosensitization of gemcitabine by LY294002 was shown in xenograft models of pancreatic cancer. However, the involvement of DNA-PK inhibition was not addressed[131]. NU7026, which is structurally related to LY294002, was shown to have better potency and selectivity for the PIKK family kinases. It chemosensitized cells for gemcitabine[132] and impaired NHEJ repair of DNA DSB, following IR in pancreatic cancer cell lines; however, HR repair was inefficiently increased and cells showed prolonged γH2AX expression. These data indicated that radiosensitization occurred through inhibition of DNA-PK[133]. NU7441, developed from the LY294002 backbone, sensitized cells to gemcitabine in PANC-1 cells[132]. In addition, radiosensitization was only demonstrated in V3-YAC cells, with proficient DNA-PKcs, but not in V3 cells without it; this confirmed the mechanism of NU7441[134]. However, the poor pharmacokinetics of NU7026 and NU7441 precluded them from further clinical development[135]. Other DNA-PK inhibitors, including IC86621, IC87102, IC87361, OK-1035, SU11752, and KU-00600648, are currently in preclinical development[135,136].
In general, the clinical development of PARP, ATM, ATR, Chk1, CHk2, Wee1, PP2A, and DNA-PK inhibitors is being pursued actively (Table 1). DNA damage is a universal characteristic of pancreatic cancer cells from the premalignant to invasive stages; therefore, the use of DNA repair inhibitors, either singly or in combinations, is of great potential. The concept of synthetic lethality has been supported by the impressive clinical success of PARP inhibitors in BRCA-defective cancers. The optimal combination of each of these agents with radiotherapy has yet to be determined for pancreatic cancer, because of limited clinical data. Reliable biomarkers for these agents, with or without radiotherapy, are largely unknown. Chemosensitization, between these agents and genotoxic chemotherapy drugs, has been well defined in pancreatic cancer preclinical studies. However, the best regimen and administration sequence, of a combination of chemotherapy, radiotherapy, and these agents, remain to be elucidated. Finally, immune checkpoint inhibitors have the potential for creating neoantigens, through the combined action of radiation, inhibitors of DNA repair enzymes, and genotoxic chemotherapeutic agents. This approach may open a new field of therapeutics in cancers without high mutation loads, such as pancreatic cancer[137].
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Taiwan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chen YC, Tang Y S- Editor: Yu J L- Editor: A E- Editor: Ma S
| 1. | Yang SH, Kuo YH, Tien YW, Hsu C, Hsu CH, Kuo SH, Cheng AL. Inferior survival of advanced pancreatic cancer patients who received gemcitabine-based chemotherapy but did not participate in clinical trials. Oncology. 2011;81:143-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Herreros-Villanueva M, Bujanda L. Non-invasive biomarkers in pancreatic cancer diagnosis: what we need versus what we have. Ann Transl Med. 2016;4:134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 3. | Vasen H, Ibrahim I, Ponce CG, Slater EP, Matthäi E, Carrato A, Earl J, Robbers K, van Mil AM, Potjer T. Benefit of Surveillance for Pancreatic Cancer in High-Risk Individuals: Outcome of Long-Term Prospective Follow-Up Studies From Three European Expert Centers. J Clin Oncol. 2016;34:2010-2019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 269] [Article Influence: 29.9] [Reference Citation Analysis (0)] |
| 4. | Harinck F, Konings IC, Kluijt I, Poley JW, van Hooft JE, van Dullemen HM, Nio CY, Krak NC, Hermans JJ, Aalfs CM. A multicentre comparative prospective blinded analysis of EUS and MRI for screening of pancreatic cancer in high-risk individuals. Gut. 2015; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 132] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 5. | Oettle H, Neuhaus P, Hochhaus A, Hartmann JT, Gellert K, Ridwelski K, Niedergethmann M, Zülke C, Fahlke J, Arning MB. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA. 2013;310:1473-1481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1180] [Cited by in RCA: 1361] [Article Influence: 113.4] [Reference Citation Analysis (0)] |
| 6. | Oettle H, Post S, Neuhaus P, Gellert K, Langrehr J, Ridwelski K, Schramm H, Fahlke J, Zuelke C, Burkart C. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA. 2007;297:267-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1779] [Cited by in RCA: 1763] [Article Influence: 97.9] [Reference Citation Analysis (0)] |
| 7. | Rhim AD, Mirek ET, Aiello NM, Maitra A, Bailey JM, McAllister F, Reichert M, Beatty GL, Rustgi AK, Vonderheide RH. EMT and dissemination precede pancreatic tumor formation. Cell. 2012;148:349-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1400] [Cited by in RCA: 1667] [Article Influence: 128.2] [Reference Citation Analysis (0)] |
| 8. | Regine WF, Winter KA, Abrams RA, Safran H, Hoffman JP, Konski A, Benson AB, Macdonald JS, Kudrimoti MR, Fromm ML. Fluorouracil vs gemcitabine chemotherapy before and after fluorouracil-based chemoradiation following resection of pancreatic adenocarcinoma: a randomized controlled trial. JAMA. 2008;299:1019-1026. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 576] [Cited by in RCA: 543] [Article Influence: 31.9] [Reference Citation Analysis (0)] |
| 9. | Liao WC, Chien KL, Lin YL, Wu MS, Lin JT, Wang HP, Tu YK. Adjuvant treatments for resected pancreatic adenocarcinoma: a systematic review and network meta-analysis. Lancet Oncol. 2013;14:1095-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 164] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 10. | Loehrer PJ, Feng Y, Cardenes H, Wagner L, Brell JM, Cella D, Flynn P, Ramanathan RK, Crane CH, Alberts SR. Gemcitabine alone versus gemcitabine plus radiotherapy in patients with locally advanced pancreatic cancer: an Eastern Cooperative Oncology Group trial. J Clin Oncol. 2011;29:4105-4112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 578] [Cited by in RCA: 621] [Article Influence: 44.4] [Reference Citation Analysis (0)] |
| 11. | Conroy T, Desseigne F, Ychou M, Bouché O, Guimbaud R, Bécouarn Y, Adenis A, Raoul JL, Gourgou-Bourgade S, de la Fouchardière C. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364:1817-1825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4838] [Cited by in RCA: 5637] [Article Influence: 402.6] [Reference Citation Analysis (1)] |
| 12. | Moertel CG, Frytak S, Hahn RG, O’Connell MJ, Reitemeier RJ, Rubin J, Schutt AJ, Weiland LH, Childs DS, Holbrook MA. Therapy of locally unresectable pancreatic carcinoma: a randomized comparison of high dose (6000 rads) radiation alone, moderate dose radiation (4000 rads + 5-fluorouracil), and high dose radiation + 5-fluorouracil: The Gastrointestinal Tumor Study Group. Cancer. 1981;48:1705-1710. [PubMed] |
| 13. | Klaassen DJ, MacIntyre JM, Catton GE, Engstrom PF, Moertel CG. Treatment of locally unresectable cancer of the stomach and pancreas: a randomized comparison of 5-fluorouracil alone with radiation plus concurrent and maintenance 5-fluorouracil--an Eastern Cooperative Oncology Group study. J Clin Oncol. 1985;3:373-378. [PubMed] |
| 14. | Treatment of locally unresectable carcinoma of the pancreas: comparison of combined-modality therapy (chemotherapy plus radiotherapy) to chemotherapy alone. Gastrointestinal Tumor Study Group. J Natl Cancer Inst. 1988;80:751-755. [PubMed] |
| 15. | Chauffert B, Mornex F, Bonnetain F, Rougier P, Mariette C, Bouché O, Bosset JF, Aparicio T, Mineur L, Azzedine A. Phase III trial comparing intensive induction chemoradiotherapy (60 Gy, infusional 5-FU and intermittent cisplatin) followed by maintenance gemcitabine with gemcitabine alone for locally advanced unresectable pancreatic cancer. Definitive results of the 2000-01 FFCD/SFRO study. Ann Oncol. 2008;19:1592-1599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 494] [Cited by in RCA: 535] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 16. | Huguet F, Hammel P, Vernerey D, Goldstein D, Van Laethem JL, Glimelius B, Spry N, Paget-Bailly S, Bonnetain F, Louvet C. Impact of chemoradiotherapy (CRT) on local control and time without treatment in patients with locally advanced pancreatic cancer (LAPC) included in the international phase III LAP 07 study. J Clin Oncol. 2014;32 Suppl 15:4001. |
| 17. | Burris HA, Moore MJ, Andersen J, Green MR, Rothenberg ML, Modiano MR, Cripps MC, Portenoy RK, Storniolo AM, Tarassoff P. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J Clin Oncol. 1997;15:2403-2413. [PubMed] |
| 18. | Singal V, Singal AK, Kuo YF. Racial disparities in treatment for pancreatic cancer and impact on survival: a population-based analysis. J Cancer Res Clin Oncol. 2012;138:715-722. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 19. | Matsuno S, Egawa S, Fukuyama S, Motoi F, Sunamura M, Isaji S, Imaizumi T, Okada S, Kato H, Suda K. Pancreatic Cancer Registry in Japan: 20 years of experience. Pancreas. 2004;28:219-230. [PubMed] |
| 20. | van Heek NT, Meeker AK, Kern SE, Yeo CJ, Lillemoe KD, Cameron JL, Offerhaus GJ, Hicks JL, Wilentz RE, Goggins MG. Telomere shortening is nearly universal in pancreatic intraepithelial neoplasia. Am J Pathol. 2002;161:1541-1547. [PubMed] |
| 21. | Matsuda Y, Ishiwata T, Izumiyama-Shimomura N, Hamayasu H, Fujiwara M, Tomita K, Hiraishi N, Nakamura K, Ishikawa N, Aida J. Gradual telomere shortening and increasing chromosomal instability among PanIN grades and normal ductal epithelia with and without cancer in the pancreas. PLoS One. 2015;10:e0117575. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 22. | Seki K, Suda T, Aoyagi Y, Sugawara S, Natsui M, Motoyama H, Shirai Y, Sekine T, Kawai H, Mita Y. Diagnosis of pancreatic adenocarcinoma by detection of human telomerase reverse transcriptase messenger RNA in pancreatic juice with sample qualification. Clin Cancer Res. 2001;7:1976-1981. [PubMed] |
| 23. | Uziel O, Beery E, Dronichev V, Samocha K, Gryaznov S, Weiss L, Slavin S, Kushnir M, Nordenberg Y, Rabinowitz C. Telomere shortening sensitizes cancer cells to selected cytotoxic agents: in vitro and in vivo studies and putative mechanisms. PLoS One. 2010;5:e9132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 24. | Frías C, García-Aranda C, De Juan C, Morán A, Ortega P, Gómez A, Hernando F, López-Asenjo JA, Torres AJ, Benito M. Telomere shortening is associated with poor prognosis and telomerase activity correlates with DNA repair impairment in non-small cell lung cancer. Lung Cancer. 2008;60:416-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 64] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 25. | Koorstra JB, Hong SM, Shi C, Meeker AK, Ryu JK, Offerhaus GJ, Goggins MG, Hruban RH, Maitra A. Widespread activation of the DNA damage response in human pancreatic intraepithelial neoplasia. Mod Pathol. 2009;22:1439-1445. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 26. | Miyasaka Y, Nagai E, Yamaguchi H, Fujii K, Inoue T, Ohuchida K, Yamada T, Mizumoto K, Tanaka M, Tsuneyoshi M. The role of the DNA damage checkpoint pathway in intraductal papillary mucinous neoplasms of the pancreas. Clin Cancer Res. 2007;13:4371-4377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 27. | Osterman M, Kathawa D, Liu D, Guo H, Zhang C, Li M, Yu X, Li F. Elevated DNA damage response in pancreatic cancer. Histochem Cell Biol. 2014;142:713-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Rustgi AK. Familial pancreatic cancer: genetic advances. Genes Dev. 2014;28:1-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 29. | Waddell N, Pajic M, Patch AM, Chang DK, Kassahn KS, Bailey P, Johns AL, Miller D, Nones K, Quek K. Whole genomes redefine the mutational landscape of pancreatic cancer. Nature. 2015;518:495-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2130] [Cited by in RCA: 1991] [Article Influence: 199.1] [Reference Citation Analysis (1)] |
| 30. | Schreiber V, Dantzer F, Ame JC, de Murcia G. Poly(ADP-ribose): novel functions for an old molecule. Nat Rev Mol Cell Biol. 2006;7:517-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1444] [Cited by in RCA: 1512] [Article Influence: 79.6] [Reference Citation Analysis (0)] |
| 31. | Fong PC, Boss DS, Yap TA, Tutt A, Wu P, Mergui-Roelvink M, Mortimer P, Swaisland H, Lau A, O’Connor MJ. Inhibition of poly(ADP-ribose) polymerase in tumors from BRCA mutation carriers. N Engl J Med. 2009;361:123-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3070] [Cited by in RCA: 2863] [Article Influence: 178.9] [Reference Citation Analysis (0)] |
| 32. | Tutt A, Robson M, Garber JE, Domchek SM, Audeh MW, Weitzel JN, Friedlander M, Arun B, Loman N, Schmutzler RK. Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and advanced breast cancer: a proof-of-concept trial. Lancet. 2010;376:235-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1352] [Cited by in RCA: 1365] [Article Influence: 91.0] [Reference Citation Analysis (0)] |
| 33. | Audeh MW, Carmichael J, Penson RT, Friedlander M, Powell B, Bell-McGuinn KM, Scott C, Weitzel JN, Oaknin A, Loman N. Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and recurrent ovarian cancer: a proof-of-concept trial. Lancet. 2010;376:245-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1055] [Cited by in RCA: 1077] [Article Influence: 71.8] [Reference Citation Analysis (0)] |
| 34. | Kaufman B, Shapira-Frommer R, Schmutzler RK, Audeh MW, Friedlander M, Balmaña J, Mitchell G, Fried G, Stemmer SM, Hubert A. Olaparib monotherapy in patients with advanced cancer and a germline BRCA1/2 mutation. J Clin Oncol. 2015;33:244-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1153] [Cited by in RCA: 1328] [Article Influence: 120.7] [Reference Citation Analysis (0)] |
| 35. | Bryant HE, Schultz N, Thomas HD, Parker KM, Flower D, Lopez E, Kyle S, Meuth M, Curtin NJ, Helleday T. Specific killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) polymerase. Nature. 2005;434:913-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3368] [Cited by in RCA: 3839] [Article Influence: 192.0] [Reference Citation Analysis (0)] |
| 36. | Farmer H, McCabe N, Lord CJ, Tutt AN, Johnson DA, Richardson TB, Santarosa M, Dillon KJ, Hickson I, Knights C. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature. 2005;434:917-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4316] [Cited by in RCA: 4884] [Article Influence: 244.2] [Reference Citation Analysis (0)] |
| 37. | Drew Y, Mulligan EA, Vong WT, Thomas HD, Kahn S, Kyle S, Mukhopadhyay A, Los G, Hostomsky Z, Plummer ER. Therapeutic potential of poly(ADP-ribose) polymerase inhibitor AG014699 in human cancers with mutated or methylated BRCA1 or BRCA2. J Natl Cancer Inst. 2011;103:334-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 200] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 38. | Hartwell LH, Szankasi P, Roberts CJ, Murray AW, Friend SH. Integrating genetic approaches into the discovery of anticancer drugs. Science. 1997;278:1064-1068. [PubMed] |
| 39. | Roy R, Chun J, Powell SN. BRCA1 and BRCA2: different roles in a common pathway of genome protection. Nat Rev Cancer. 2012;12:68-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 898] [Cited by in RCA: 1061] [Article Influence: 75.8] [Reference Citation Analysis (0)] |
| 40. | Shen Y, Rehman FL, Feng Y, Boshuizen J, Bajrami I, Elliott R, Wang B, Lord CJ, Post LE, Ashworth A. BMN 673, a novel and highly potent PARP1/2 inhibitor for the treatment of human cancers with DNA repair deficiency. Clin Cancer Res. 2013;19:5003-5015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 382] [Cited by in RCA: 399] [Article Influence: 33.3] [Reference Citation Analysis (0)] |
| 41. | Andrei AZ, Hall A, Smith AL, Bascuñana C, Malina A, Connor A, Altinel-Omeroglu G, Huang S, Pelletier J, Huntsman D. Increased in vitro and in vivo sensitivity of BRCA2-associated pancreatic cancer to the poly(ADP-ribose) polymerase-1/2 inhibitor BMN 673. Cancer Lett. 2015;364:8-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 42. | Fogelman DR, Wolff RA, Kopetz S, Javle M, Bradley C, Mok I, Cabanillas F, Abbruzzese JL. Evidence for the efficacy of Iniparib, a PARP-1 inhibitor, in BRCA2-associated pancreatic cancer. Anticancer Res. 2011;31:1417-1420. [PubMed] |
| 43. | Bendell J, O’Reilly EM, Middleton MR, Chau I, Hochster H, Fielding A, Burke W, Burris H. Phase I study of olaparib plus gemcitabine in patients with advanced solid tumours and comparison with gemcitabine alone in patients with locally advanced/metastatic pancreatic cancer. Ann Oncol. 2015;26:804-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 83] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 44. | Shen SX, Weaver Z, Xu X, Li C, Weinstein M, Chen L, Guan XY, Ried T, Deng CX. A targeted disruption of the murine Brca1 gene causes gamma-irradiation hypersensitivity and genetic instability. Oncogene. 1998;17:3115-3124. [PubMed] |
| 45. | Albert JM, Cao C, Kim KW, Willey CD, Geng L, Xiao D, Wang H, Sandler A, Johnson DH, Colevas AD. Inhibition of poly(ADP-ribose) polymerase enhances cell death and improves tumor growth delay in irradiated lung cancer models. Clin Cancer Res. 2007;13:3033-3042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 208] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 46. | Liu SK, Coackley C, Krause M, Jalali F, Chan N, Bristow RG. A novel poly(ADP-ribose) polymerase inhibitor, ABT-888, radiosensitizes malignant human cell lines under hypoxia. Radiother Oncol. 2008;88:258-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 98] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 47. | Dungey FA, Löser DA, Chalmers AJ. Replication-dependent radiosensitization of human glioma cells by inhibition of poly(ADP-Ribose) polymerase: mechanisms and therapeutic potential. Int J Radiat Oncol Biol Phys. 2008;72:1188-1197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 174] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 48. | Miura K, Sakata K, Someya M, Matsumoto Y, Matsumoto H, Takahashi A, Hareyama M. The combination of olaparib and camptothecin for effective radiosensitization. Radiat Oncol. 2012;7:62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 49. | Chow JP, Man WY, Mao M, Chen H, Cheung F, Nicholls J, Tsao SW, Li Lung M, Poon RY. PARP1 is overexpressed in nasopharyngeal carcinoma and its inhibition enhances radiotherapy. Mol Cancer Ther. 2013;12:2517-2528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 58] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 50. | Lee HJ, Yoon C, Schmidt B, Park do J, Zhang AY, Erkizan HV, Toretsky JA, Kirsch DG, Yoon SS. Combining PARP-1 inhibition and radiation in Ewing sarcoma results in lethal DNA damage. Mol Cancer Ther. 2013;12:2591-2600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 51. | Guillot C, Favaudon V, Herceg Z, Sagne C, Sauvaigo S, Merle P, Hall J, Chemin I. PARP inhibition and the radiosensitizing effects of the PARP inhibitor ABT-888 in in vitro hepatocellular carcinoma models. BMC Cancer. 2014;14:603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 52. | Senra JM, Telfer BA, Cherry KE, McCrudden CM, Hirst DG, O’Connor MJ, Wedge SR, Stratford IJ. Inhibition of PARP-1 by olaparib (AZD2281) increases the radiosensitivity of a lung tumor xenograft. Mol Cancer Ther. 2011;10:1949-1958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 152] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 53. | Vance S, Liu E, Zhao L, Parsels JD, Parsels LA, Brown JL, Maybaum J, Lawrence TS, Morgan MA. Selective radiosensitization of p53 mutant pancreatic cancer cells by combined inhibition of Chk1 and PARP1. Cell Cycle. 2011;10:4321-4329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 75] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 54. | Hirai T, Shirai H, Fujimori H, Okayasu R, Sasai K, Masutani M. Radiosensitization effect of poly(ADP-ribose) polymerase inhibition in cells exposed to low and high liner energy transfer radiation. Cancer Sci. 2012;103:1045-1050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 55. | Porcelli L, Quatrale AE, Mantuano P, Leo MG, Silvestris N, Rolland JF, Carioggia E, Lioce M, Paradiso A, Azzariti A. Optimize radiochemotherapy in pancreatic cancer: PARP inhibitors a new therapeutic opportunity. Mol Oncol. 2013;7:308-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 56. | Tuli R, Surmak AJ, Reyes J, Armour M, Hacker-Prietz A, Wong J, DeWeese TL, Herman JM. Radiosensitization of Pancreatic Cancer Cells In Vitro and In Vivo through Poly (ADP-ribose) Polymerase Inhibition with ABT-888. Transl Oncol. 2014; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 57. | Karnak D, Engelke CG, Parsels LA, Kausar T, Wei D, Robertson JR, Marsh KB, Davis MA, Zhao L, Maybaum J. Combined inhibition of Wee1 and PARP1/2 for radiosensitization in pancreatic cancer. Clin Cancer Res. 2014;20:5085-5096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 129] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 58. | McPherson LA, Shen Y, Ford JM. Poly (ADP-ribose) polymerase inhibitor LT-626: Sensitivity correlates with MRE11 mutations and synergizes with platinums and irinotecan in colorectal cancer cells. Cancer Lett. 2014;343:217-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 59. | Shelton JW, Waxweiler TV, Landry J, Gao H, Xu Y, Wang L, El-Rayes B, Shu HK. In vitro and in vivo enhancement of chemoradiation using the oral PARP inhibitor ABT-888 in colorectal cancer cells. Int J Radiat Oncol Biol Phys. 2013;86:469-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 60. | Ogrunc M, Di Micco R, Liontos M, Bombardelli L, Mione M, Fumagalli M, Gorgoulis VG, d’Adda di Fagagna F. Oncogene-induced reactive oxygen species fuel hyperproliferation and DNA damage response activation. Cell Death Differ. 2014;21:998-1012. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 205] [Cited by in RCA: 240] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 61. | Gilad O, Nabet BY, Ragland RL, Schoppy DW, Smith KD, Durham AC, Brown EJ. Combining ATR suppression with oncogenic Ras synergistically increases genomic instability, causing synthetic lethality or tumorigenesis in a dosage-dependent manner. Cancer Res. 2010;70:9693-9702. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 201] [Cited by in RCA: 186] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 62. | Schoppy DW, Ragland RL, Gilad O, Shastri N, Peters AA, Murga M, Fernandez-Capetillo O, Diehl JA, Brown EJ. Oncogenic stress sensitizes murine cancers to hypomorphic suppression of ATR. J Clin Invest. 2012;122:241-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 153] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 63. | Shibata A, Moiani D, Arvai AS, Perry J, Harding SM, Genois MM, Maity R, van Rossum-Fikkert S, Kertokalio A, Romoli F. DNA double-strand break repair pathway choice is directed by distinct MRE11 nuclease activities. Mol Cell. 2014;53:7-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 449] [Cited by in RCA: 449] [Article Influence: 40.8] [Reference Citation Analysis (0)] |
| 64. | Bakkenist CJ, Kastan MB. DNA damage activates ATM through intermolecular autophosphorylation and dimer dissociation. Nature. 2003;421:499-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2489] [Cited by in RCA: 2562] [Article Influence: 116.5] [Reference Citation Analysis (0)] |
| 65. | Lee JH, Paull TT. ATM activation by DNA double-strand breaks through the Mre11-Rad50-Nbs1 complex. Science. 2005;308:551-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1067] [Cited by in RCA: 1061] [Article Influence: 53.1] [Reference Citation Analysis (0)] |
| 66. | Burma S, Chen BP, Murphy M, Kurimasa A, Chen DJ. ATM phosphorylates histone H2AX in response to DNA double-strand breaks. J Biol Chem. 2001;276:42462-42467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1379] [Cited by in RCA: 1460] [Article Influence: 60.8] [Reference Citation Analysis (0)] |
| 67. | Stiff T, O’Driscoll M, Rief N, Iwabuchi K, Löbrich M, Jeggo PA. ATM and DNA-PK function redundantly to phosphorylate H2AX after exposure to ionizing radiation. Cancer Res. 2004;64:2390-2396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 761] [Cited by in RCA: 779] [Article Influence: 37.1] [Reference Citation Analysis (0)] |
| 68. | Stucki M, Clapperton JA, Mohammad D, Yaffe MB, Smerdon SJ, Jackson SP. MDC1 directly binds phosphorylated histone H2AX to regulate cellular responses to DNA double-strand breaks. Cell. 2005;123:1213-1226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 765] [Cited by in RCA: 833] [Article Influence: 43.8] [Reference Citation Analysis (0)] |
| 69. | Banin S, Moyal L, Shieh S, Taya Y, Anderson CW, Chessa L, Smorodinsky NI, Prives C, Reiss Y, Shiloh Y. Enhanced phosphorylation of p53 by ATM in response to DNA damage. Science. 1998;281:1674-1677. [PubMed] |
| 70. | Canman CE, Lim DS, Cimprich KA, Taya Y, Tamai K, Sakaguchi K, Appella E, Kastan MB, Siliciano JD. Activation of the ATM kinase by ionizing radiation and phosphorylation of p53. Science. 1998;281:1677-1679. [PubMed] |
| 71. | Matsuoka S, Rotman G, Ogawa A, Shiloh Y, Tamai K, Elledge SJ. Ataxia telangiectasia-mutated phosphorylates Chk2 in vivo and in vitro. Proc Natl Acad Sci USA. 2000;97:10389-10394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 638] [Cited by in RCA: 649] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 72. | Cortez D, Guntuku S, Qin J, Elledge SJ. ATR and ATRIP: partners in checkpoint signaling. Science. 2001;294:1713-1716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 705] [Cited by in RCA: 772] [Article Influence: 32.2] [Reference Citation Analysis (0)] |
| 73. | Zou L, Elledge SJ. Sensing DNA damage through ATRIP recognition of RPA-ssDNA complexes. Science. 2003;300:1542-1548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1971] [Cited by in RCA: 2125] [Article Influence: 96.6] [Reference Citation Analysis (0)] |
| 74. | Burtelow MA, Roos-Mattjus PM, Rauen M, Babendure JR, Karnitz LM. Reconstitution and molecular analysis of the hRad9-hHus1-hRad1 (9-1-1) DNA damage responsive checkpoint complex. J Biol Chem. 2001;276:25903-25909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 107] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 75. | Kumagai A, Lee J, Yoo HY, Dunphy WG. TopBP1 activates the ATR-ATRIP complex. Cell. 2006;124:943-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 541] [Cited by in RCA: 573] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 76. | Chini CC, Chen J. Human claspin is required for replication checkpoint control. J Biol Chem. 2003;278:30057-30062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 191] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 77. | Sarkaria JN, Busby EC, Tibbetts RS, Roos P, Taya Y, Karnitz LM, Abraham RT. Inhibition of ATM and ATR kinase activities by the radiosensitizing agent, caffeine. Cancer Res. 1999;59:4375-4382. [PubMed] |
| 78. | Yao SL, Akhtar AJ, McKenna KA, Bedi GC, Sidransky D, Mabry M, Ravi R, Collector MI, Jones RJ, Sharkis SJ. Selective radiosensitization of p53-deficient cells by caffeine-mediated activation of p34cdc2 kinase. Nat Med. 1996;2:1140-1143. [PubMed] |
| 79. | Hickson I, Zhao Y, Richardson CJ, Green SJ, Martin NM, Orr AI, Reaper PM, Jackson SP, Curtin NJ, Smith GC. Identification and characterization of a novel and specific inhibitor of the ataxia-telangiectasia mutated kinase ATM. Cancer Res. 2004;64:9152-9159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 935] [Cited by in RCA: 983] [Article Influence: 49.2] [Reference Citation Analysis (0)] |
| 80. | Golding SE, Rosenberg E, Valerie N, Hussaini I, Frigerio M, Cockcroft XF, Chong WY, Hummersone M, Rigoreau L, Menear KA. Improved ATM kinase inhibitor KU-60019 radiosensitizes glioma cells, compromises insulin, AKT and ERK prosurvival signaling, and inhibits migration and invasion. Mol Cancer Ther. 2009;8:2894-2902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 296] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 81. | Biddlestone-Thorpe L, Sajjad M, Rosenberg E, Beckta JM, Valerie NC, Tokarz M, Adams BR, Wagner AF, Khalil A, Gilfor D. ATM kinase inhibition preferentially sensitizes p53-mutant glioma to ionizing radiation. Clin Cancer Res. 2013;19:3189-3200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 162] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 82. | Batey MA, Zhao Y, Kyle S, Richardson C, Slade A, Martin NM, Lau A, Newell DR, Curtin NJ. Preclinical evaluation of a novel ATM inhibitor, KU59403, in vitro and in vivo in p53 functional and dysfunctional models of human cancer. Mol Cancer Ther. 2013;12:959-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 83. | Nishida H, Tatewaki N, Nakajima Y, Magara T, Ko KM, Hamamori Y, Konishi T. Inhibition of ATR protein kinase activity by schisandrin B in DNA damage response. Nucleic Acids Res. 2009;37:5678-5689. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 101] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 84. | Reaper PM, Griffiths MR, Long JM, Charrier JD, Maccormick S, Charlton PA, Golec JM, Pollard JR. Selective killing of ATM- or p53-deficient cancer cells through inhibition of ATR. Nat Chem Biol. 2011;7:428-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 448] [Cited by in RCA: 499] [Article Influence: 35.6] [Reference Citation Analysis (0)] |
| 85. | Pires IM, Olcina MM, Anbalagan S, Pollard JR, Reaper PM, Charlton PA, McKenna WG, Hammond EM. Targeting radiation-resistant hypoxic tumour cells through ATR inhibition. Br J Cancer. 2012;107:291-299. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 117] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 86. | Prevo R, Fokas E, Reaper PM, Charlton PA, Pollard JR, McKenna WG, Muschel RJ, Brunner TB. The novel ATR inhibitor VE-821 increases sensitivity of pancreatic cancer cells to radiation and chemotherapy. Cancer Biol Ther. 2012;13:1072-1081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 187] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 87. | Fokas E, Prevo R, Pollard JR, Reaper PM, Charlton PA, Cornelissen B, Vallis KA, Hammond EM, Olcina MM, Gillies McKenna W. Targeting ATR in vivo using the novel inhibitor VE-822 results in selective sensitization of pancreatic tumors to radiation. Cell Death Dis. 2012;3:e441. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 278] [Cited by in RCA: 276] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 88. | Foote KM, Blades K, Cronin A, Fillery S, Guichard SS, Hassall L, Hickson I, Jacq X, Jewsbury PJ, McGuire TM. Discovery of 4-{4-[(3R)-3-Methylmorpholin-4-yl]-6-[1-(methylsulfonyl)cyclopropyl]pyrimidin-2-yl}-1H-indole (AZ20): a potent and selective inhibitor of ATR protein kinase with monotherapy in vivo antitumor activity. J Med Chem. 2013;56:2125-2138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 176] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 89. | Guichard SM, Brown E, Odedra R, Hughes A, Heathcote D, Barnes J, Lau A, Powell S, Jones CD, Nissink W. The pre-clinical in vitro and in vivo activity of AZD6738: A potent and selective inhibitor of ATR kinase. Cancer Res. 2013;73:3343. [DOI] [Full Text] |
| 90. | Sanchez Y, Wong C, Thoma RS, Richman R, Wu Z, Piwnica-Worms H, Elledge SJ. Conservation of the Chk1 checkpoint pathway in mammals: linkage of DNA damage to Cdk regulation through Cdc25. Science. 1997;277:1497-1501. [PubMed] |
| 91. | Zeng Y, Forbes KC, Wu Z, Moreno S, Piwnica-Worms H, Enoch T. Replication checkpoint requires phosphorylation of the phosphatase Cdc25 by Cds1 or Chk1. Nature. 1998;395:507-510. [PubMed] |
| 92. | Melixetian M, Klein DK, Sørensen CS, Helin K. NEK11 regulates CDC25A degradation and the IR-induced G2/M checkpoint. Nat Cell Biol. 2009;11:1247-1253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 98] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 93. | Mailand N, Falck J, Lukas C, Syljuâsen RG, Welcker M, Bartek J, Lukas J. Rapid destruction of human Cdc25A in response to DNA damage. Science. 2000;288:1425-1429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 585] [Cited by in RCA: 572] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 94. | Fuse E, Tanii H, Kurata N, Kobayashi H, Shimada Y, Tamura T, Sasaki Y, Tanigawara Y, Lush RD, Headlee D. Unpredicted clinical pharmacology of UCN-01 caused by specific binding to human alpha1-acid glycoprotein. Cancer Res. 1998;58:3248-3253. [PubMed] |
| 95. | Sausville EA, Arbuck SG, Messmann R, Headlee D, Bauer KS, Lush RM, Murgo A, Figg WD, Lahusen T, Jaken S. Phase I trial of 72-hour continuous infusion UCN-01 in patients with refractory neoplasms. J Clin Oncol. 2001;19:2319-2333. [PubMed] |
| 96. | Hattori H, Skoulidis F, Russell P, Venkitaraman AR. Context dependence of checkpoint kinase 1 as a therapeutic target for pancreatic cancers deficient in the BRCA2 tumor suppressor. Mol Cancer Ther. 2011;10:670-678. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 97. | Zabludoff SD, Deng C, Grondine MR, Sheehy AM, Ashwell S, Caleb BL, Green S, Haye HR, Horn CL, Janetka JW. AZD7762, a novel checkpoint kinase inhibitor, drives checkpoint abrogation and potentiates DNA-targeted therapies. Mol Cancer Ther. 2008;7:2955-2966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 334] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 98. | Mitchell JB, Choudhuri R, Fabre K, Sowers AL, Citrin D, Zabludoff SD, Cook JA. In vitro and in vivo radiation sensitization of human tumor cells by a novel checkpoint kinase inhibitor, AZD7762. Clin Cancer Res. 2010;16:2076-2084. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 107] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 99. | Morgan MA, Parsels LA, Zhao L, Parsels JD, Davis MA, Hassan MC, Arumugarajah S, Hylander-Gans L, Morosini D, Simeone DM. Mechanism of radiosensitization by the Chk1/2 inhibitor AZD7762 involves abrogation of the G2 checkpoint and inhibition of homologous recombinational DNA repair. Cancer Res. 2010;70:4972-4981. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 251] [Cited by in RCA: 240] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 100. | Seto T, Esaki T, Hirai F, Arita S, Nosaki K, Makiyama A, Kometani T, Fujimoto C, Hamatake M, Takeoka H. Phase I, dose-escalation study of AZD7762 alone and in combination with gemcitabine in Japanese patients with advanced solid tumours. Cancer Chemother Pharmacol. 2013;72:619-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 76] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 101. | Sausville E, Lorusso P, Carducci M, Carter J, Quinn MF, Malburg L, Azad N, Cosgrove D, Knight R, Barker P. Phase I dose-escalation study of AZD7762, a checkpoint kinase inhibitor, in combination with gemcitabine in US patients with advanced solid tumors. Cancer Chemother Pharmacol. 2014;73:539-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 145] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 102. | Al-Ejeh F, Pajic M, Shi W, Kalimutho M, Miranda M, Nagrial AM, Chou A, Biankin AV, Grimmond SM, Brown MP. Gemcitabine and CHK1 inhibition potentiate EGFR-directed radioimmunotherapy against pancreatic ductal adenocarcinoma. Clin Cancer Res. 2014;20:3187-3197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 103. | Blasina A, Hallin J, Chen E, Arango ME, Kraynov E, Register J, Grant S, Ninkovic S, Chen P, Nichols T. Breaching the DNA damage checkpoint via PF-00477736, a novel small-molecule inhibitor of checkpoint kinase 1. Mol Cancer Ther. 2008;7:2394-2404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 175] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 104. | Barnard D, Diaz HB, Burke T, Donoho G, Beckmann R, Jones B, Barda D, King C, Marshall M. LY2603618, a selective CHK1 inhibitor, enhances the anti-tumor effect of gemcitabine in xenograft tumor models. Invest New Drugs. 2016;34:49-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 105. | Engelke CG, Parsels LA, Qian Y, Zhang Q, Karnak D, Robertson JR, Tanska DM, Wei D, Davis MA, Parsels JD. Sensitization of pancreatic cancer to chemoradiation by the Chk1 inhibitor MK8776. Clin Cancer Res. 2013;19:4412-4421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 91] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 106. | Montano R, Chung I, Garner KM, Parry D, Eastman A. Preclinical development of the novel Chk1 inhibitor SCH900776 in combination with DNA-damaging agents and antimetabolites. Mol Cancer Ther. 2012;11:427-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 102] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 107. | Doi T, Yoshino T, Shitara K, Matsubara N, Fuse N, Naito Y, Uenaka K, Nakamura T, Hynes SM, Lin AB. Phase I study of LY2603618, a CHK1 inhibitor, in combination with gemcitabine in Japanese patients with solid tumors. Anticancer Drugs. 2015;26:1043-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 108. | Daud AI, Ashworth MT, Strosberg J, Goldman JW, Mendelson D, Springett G, Venook AP, Loechner S, Rosen LS, Shanahan F. Phase I dose-escalation trial of checkpoint kinase 1 inhibitor MK-8776 as monotherapy and in combination with gemcitabine in patients with advanced solid tumors. J Clin Oncol. 2015;33:1060-1066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 154] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 109. | Matthews DJ, Yakes FM, Chen J, Tadano M, Bornheim L, Clary DO, Tai A, Wagner JM, Miller N, Kim YD. Pharmacological abrogation of S-phase checkpoint enhances the anti-tumor activity of gemcitabine in vivo. Cell Cycle. 2007;6:104-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 100] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 110. | Syljuåsen RG, Sørensen CS, Nylandsted J, Lukas C, Lukas J, Bartek J. Inhibition of Chk1 by CEP-3891 accelerates mitotic nuclear fragmentation in response to ionizing Radiation. Cancer Res. 2004;64:9035-9040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 76] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 111. | Parsels LA, Morgan MA, Tanska DM, Parsels JD, Palmer BD, Booth RJ, Denny WA, Canman CE, Kraker AJ, Lawrence TS. Gemcitabine sensitization by checkpoint kinase 1 inhibition correlates with inhibition of a Rad51 DNA damage response in pancreatic cancer cells. Mol Cancer Ther. 2009;8:45-54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 125] [Cited by in RCA: 125] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 112. | Tao Y, Leteur C, Yang C, Zhang P, Castedo M, Pierré A, Golsteyn RM, Bourhis J, Kroemer G, Deutsch E. Radiosensitization by Chir-124, a selective CHK1 inhibitor: effects of p53 and cell cycle checkpoints. Cell Cycle. 2009;8:1196-1205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 113. | Anderson VE, Walton MI, Eve PD, Boxall KJ, Antoni L, Caldwell JJ, Aherne W, Pearl LH, Oliver AW, Collins I. CCT241533 is a potent and selective inhibitor of CHK2 that potentiates the cytotoxicity of PARP inhibitors. Cancer Res. 2011;71:463-472. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 81] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 114. | Walton MI, Eve PD, Hayes A, Valenti MR, De Haven Brandon AK, Box G, Hallsworth A, Smith EL, Boxall KJ, Lainchbury M. CCT244747 is a novel potent and selective CHK1 inhibitor with oral efficacy alone and in combination with genotoxic anticancer drugs. Clin Cancer Res. 2012;18:5650-5661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 69] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 115. | King C, Diaz HB, McNeely S, Barnard D, Dempsey J, Blosser W, Beckmann R, Barda D, Marshall MS. LY2606368 Causes Replication Catastrophe and Antitumor Effects through CHK1-Dependent Mechanisms. Mol Cancer Ther. 2015;14:2004-2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 139] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 116. | Walton MI, Eve PD, Hayes A, Henley AT, Valenti MR, De Haven Brandon AK, Box G, Boxall KJ, Tall M, Swales K. The clinical development candidate CCT245737 is an orally active CHK1 inhibitor with preclinical activity in RAS mutant NSCLC and Eµ-MYC driven B-cell lymphoma. Oncotarget. 2016;7:2329-2342. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 117. | Walton MI, Eve PD, Hayes A, Valenti M, De Haven Brandon A, Box G, Boxall KJ, Aherne GW, Eccles SA, Raynaud FI. The preclinical pharmacology and therapeutic activity of the novel CHK1 inhibitor SAR-020106. Mol Cancer Ther. 2010;9:89-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 118. | Blackwood E, Epler J, Yen I, Flagella M, O’Brien T, Evangelista M, Schmidt S, Xiao Y, Choi J, Kowanetz K. Combination drug scheduling defines a “window of opportunity” for chemopotentiation of gemcitabine by an orally bioavailable, selective ChK1 inhibitor, GNE-900. Mol Cancer Ther. 2013;12:1968-1980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 119. | Kharbanda S, Saleem A, Datta R, Yuan ZM, Weichselbaum R, Kufe D. Ionizing radiation induces rapid tyrosine phosphorylation of p34cdc2. Cancer Res. 1994;54:1412-1414. [PubMed] |
| 120. | Margolis SS, Perry JA, Forester CM, Nutt LK, Guo Y, Jardim MJ, Thomenius MJ, Freel CD, Darbandi R, Ahn JH. Role for the PP2A/B56delta phosphatase in regulating 14-3-3 release from Cdc25 to control mitosis. Cell. 2006;127:759-773. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 160] [Cited by in RCA: 160] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 121. | Krajewska M, Heijink AM, Bisselink YJ, Seinstra RI, Silljé HH, de Vries EG, van Vugt MA. Forced activation of Cdk1 via wee1 inhibition impairs homologous recombination. Oncogene. 2013;32:3001-3008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 110] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 122. | Rajeshkumar NV, De Oliveira E, Ottenhof N, Watters J, Brooks D, Demuth T, Shumway SD, Mizuarai S, Hirai H, Maitra A. MK-1775, a potent Wee1 inhibitor, synergizes with gemcitabine to achieve tumor regressions, selectively in p53-deficient pancreatic cancer xenografts. Clin Cancer Res. 2011;17:2799-2806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 232] [Cited by in RCA: 218] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 123. | Kausar T, Schreiber JS, Karnak D, Parsels LA, Parsels JD, Davis MA, Zhao L, Maybaum J, Lawrence TS, Morgan MA. Sensitization of Pancreatic Cancers to Gemcitabine Chemoradiation by WEE1 Kinase Inhibition Depends on Homologous Recombination Repair. Neoplasia. 2015;17:757-766. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 124. | Do K, Wilsker D, Ji J, Zlott J, Freshwater T, Kinders RJ, Collins J, Chen AP, Doroshow JH, Kummar S. Phase I Study of Single-Agent AZD1775 (MK-1775), a Wee1 Kinase Inhibitor, in Patients With Refractory Solid Tumors. J Clin Oncol. 2015;33:3409-3415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 272] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 125. | Chung V, Richards D, Braiteh F, Kovach JS, Mansfield AS. A phase 1 study of a novel inhibitor of protein phosphatase 2A alone or in combination with docetaxel. [abstract]. In: Proceedings of the AACR-NCI-EORTC International Conference: Molecular Targets and Cancer Therapeutics; 2015 Nov 5-9; Boston, MA. Philadelphia (PA): AACR. Mol Cancer Ther. 2015;14 Suppl 2:Abstract nr A175. [DOI] [Full Text] |
| 126. | Wei D, Parsels LA, Karnak D, Davis MA, Parsels JD, Marsh AC, Zhao L, Maybaum J, Lawrence TS, Sun Y. Inhibition of protein phosphatase 2A radiosensitizes pancreatic cancers by modulating CDC25C/CDK1 and homologous recombination repair. Clin Cancer Res. 2013;19:4422-4432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 81] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 127. | Gottlieb TM, Jackson SP. The DNA-dependent protein kinase: requirement for DNA ends and association with Ku antigen. Cell. 1993;72:131-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 854] [Cited by in RCA: 894] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 128. | Critchlow SE, Bowater RP, Jackson SP. Mammalian DNA double-strand break repair protein XRCC4 interacts with DNA ligase IV. Curr Biol. 1997;7:588-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 320] [Cited by in RCA: 334] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 129. | Rosenzweig KE, Youmell MB, Palayoor ST, Price BD. Radiosensitization of human tumor cells by the phosphatidylinositol3-kinase inhibitors wortmannin and LY294002 correlates with inhibition of DNA-dependent protein kinase and prolonged G2-M delay. Clin Cancer Res. 1997;3:1149-1156. [PubMed] |
| 130. | Wang H, Zeng ZC, Bui TA, DiBiase SJ, Qin W, Xia F, Powell SN, Iliakis G. Nonhomologous end-joining of ionizing radiation-induced DNA double-stranded breaks in human tumor cells deficient in BRCA1 or BRCA2. Cancer Res. 2001;61:270-277. [PubMed] |
| 131. | Bondar VM, Sweeney-Gotsch B, Andreeff M, Mills GB, McConkey DJ. Inhibition of the phosphatidylinositol 3’-kinase-AKT pathway induces apoptosis in pancreatic carcinoma cells in vitro and in vivo. Mol Cancer Ther. 2002;1:989-997. [PubMed] |
| 132. | Hu H, Gu Y, Qian Y, Hu B, Zhu C, Wang G, Li J. DNA-PKcs is important for Akt activation and gemcitabine resistance in PANC-1 pancreatic cancer cells. Biochem Biophys Res Commun. 2014;452:106-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 133. | Li YH, Wang X, Pan Y, Lee DH, Chowdhury D, Kimmelman AC. Inhibition of non-homologous end joining repair impairs pancreatic cancer growth and enhances radiation response. PLoS One. 2012;7:e39588. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 60] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 134. | Zhao Y, Thomas HD, Batey MA, Cowell IG, Richardson CJ, Griffin RJ, Calvert AH, Newell DR, Smith GC, Curtin NJ. Preclinical evaluation of a potent novel DNA-dependent protein kinase inhibitor NU7441. Cancer Res. 2006;66:5354-5362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 354] [Cited by in RCA: 336] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 135. | Davidson D, Amrein L, Panasci L, Aloyz R. Small Molecules, Inhibitors of DNA-PK, Targeting DNA Repair, and Beyond. Front Pharmacol. 2013;4:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 111] [Cited by in RCA: 124] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 136. | Munck JM, Batey MA, Zhao Y, Jenkins H, Richardson CJ, Cano C, Tavecchio M, Barbeau J, Bardos J, Cornell L. Chemosensitization of cancer cells by KU-0060648, a dual inhibitor of DNA-PK and PI-3K. Mol Cancer Ther. 2012;11:1789-1798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 98] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 137. | Alexandrov LB, Nik-Zainal S, Wedge DC, Aparicio SA, Behjati S, Biankin AV, Bignell GR, Bolli N, Borg A, Børresen-Dale AL. Signatures of mutational processes in human cancer. Nature. 2013;500:415-421. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7533] [Cited by in RCA: 7310] [Article Influence: 609.2] [Reference Citation Analysis (1)] |