Published online Jul 28, 2016. doi: 10.3748/wjg.v22.i28.6539
Peer-review started: March 5, 2015
First decision: April 24, 2015
Revised: August 24, 2015
Accepted: September 30, 2015
Article in press: September 30, 2015
Published online: July 28, 2016
Processing time: 506 Days and 2.5 Hours
AIM: To study the accuracy of using high definition (HD) scope with narrow band imaging (NBI) vs standard white light colonoscope without NBI (ST), to predict the histology of the colon polyps, particularly those < 1 cm.
METHODS: A total of 147 African Americans patients who were referred to Howard University Hospital for screening or, diagnostic or follow up colonoscopy, during a 12-mo period in 2012 were prospectively recruited. Some patients had multiple polyps and total number of polyps was 179. Their colonoscopies were performed by 3 experienced endoscopists who determined the size and stated whether the polyps being removed were hyperplastic or adenomatous polyps using standard colonoscopes or high definition colonoscopes with NBI. The histopathologic diagnosis was reported by pathologists as part of routine care.
RESULTS: Of participants in the study, 55 (37%) were male and median (interquartile range) of age was 56 (19-80). Demographic, clinical characteristics, past medical history of patients, and the data obtained by two instruments were not significantly different and two methods detected similar number of polyps. In ST scope 89% of polyps were < 1 cm vs 87% in HD scope (P = 0.7). The ST scope had a positive predictive value (PPV) and positive likelihood ratio (PLR) of 86% and 4.0 for adenoma compared to 74% and 2.6 for HD scope. There was a trend of higher sensitivity for HD scope (68%) compare to ST scope (53%) with almost the same specificity. The ST scope had a PPV and PLR of 38% and 1.8 for hyperplastic polyp (HPP) compared to 42% and 2.2 for HD scope. The sensitivity and specificity of two instruments for HPP diagnosis were similar.
CONCLUSION: Our results indicated that HD scope was more sensitive in diagnosis of adenoma than ST scope. Clinical diagnosis of HPP with either scope is less accurate compared to adenoma. Colonoscopy diagnosis is not yet fully matched with pathologic diagnosis of colon polyp. However with the advancement of both imaging and training, it may be possible to increase the sensitivity and specificity of the scopes and hence save money for eliminating time and the cost of Immunohistochemistry/pathology.
Core tip: This study analyzed the size of polyps and stated whether the polyps being removed were hyperplastic or adenomatous polyps using standard colonoscopes or high definition colonoscopes with narrow band imaging (NBI), suggests that high definition scope was more sensitive in diagnosis of adenoma than standard white light colonoscope without NBI scope. Hence we save money for eliminating time and the cost of immunohistochemistry/pathology.
- Citation: Ashktorab H, Etaati F, Rezaeean F, Nouraie M, Paydar M, Namin HH, Sanderson A, Begum R, Alkhalloufi K, Brim H, Laiyemo AO. Can optical diagnosis of small colon polyps be accurate? Comparing standard scope without narrow banding to high definition scope with narrow banding. World J Gastroenterol 2016; 22(28): 6539-6546
- URL: https://www.wjgnet.com/1007-9327/full/v22/i28/6539.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i28.6539
Colorectal cancer is one of the most common cancers in the United States[1]. Early detection of colon cancer by colonoscopy and polyp removal is likely to decrease mortality from the disease. Colonoscopy is now established as the gold standard for the identification of both colorectal cancer and polyps[2]. It is estimated that up to 15 million colonoscopies are performed annually in the United States[3,4].
On the other hand, most polyps, which are either biopsied or removed, are non-neoplastic in nature, which provide additional burden to the pathologist[5] as well as the cost associated with unnecessary biopsies and the risk with polypectomies[6]. Also the colonoscopic miss rate of adenomas, which are considered to be precursors of colorectal cancer, is as high as 24%[7]. Therefore, the distinction between non-neoplastic and neoplastic colorectal polyps in vivo with a suitable technique can improve the accuracy of colonoscopy, particularly as a higher adenoma detection rate, could be cost saving by eliminating the need for routine pathology on every polyp < 1 cm removed during colonoscopy.
Improvements in the resolution of imaging techniques in colonoscopy over the years have resulted in a substantial increase in the polyp detection rate in the colon. One of these new imaging techniques is narrow band imaging (NBI). NBI is a relatively new endoscopic technique that increases the accuracy of diagnosis using narrow-band width filters in a red-green-blue (RGB) sequential illumination system[6]. This results in enhancement of the surface mucosal morphology, so improves the detailed visualization of the micro vascular and micro structural pit patterns[7].
A number of randomized trials comparing narrow band imaging colonoscopy with white light colonoscopy for detection of colorectal polyps reported variable results. This discrepancy in results is related to inadequately powered studies due to difference in the number and experience of endoscopists involved in the studies, as well as small sample size[8].
The first study was from Japan[9]. They examined thirty four patients and they found statistically significant difference between NBI (sensitivity 100%, specificity 75%) compared to standard scope (sensitivity 83%, specificity 44%, P < 0.05 for specificity). In the current study, we present a comparison of polyp detection rate and accuracy, using standard scope without NBI and high definition scope with NBI.
A total of one hundred forty seven African Americans (AAs) patients who were referred to Howard University Hospital (HUH) for screening or, diagnostic or follow up colonoscopy, during a 12-mo period in 2012, were prospectively recruited. All patients were consented based on approved HUH IRB. Their colonoscopies were performed by 3 experienced endoscopists (more than 2000 colonoscopies each) at the same endoscopy center, who determined the size and stated whether the polyps being removed were hyperplasic or adenomatous polyps, using standard colonoscope or high definition colonoscope with NBI. Patients were assigned to undergo colonoscopy using either standard scope without NBI or high definition (HD) scope with NBI.
Data collected for this survey include: Date of procedure, patient’s date of birth, gender, and race, height (Ht), weight (Wt), education, associated condition, reason for colonoscopy, past history of colon polyps, family history of colon cancer, smoking, alcohol consumption, colon preparation quality, number of polyps, polyp size, polyp location, type of scope, endoscopist name, duration of colonoscopy, colonoscopy diagnosis, pathologist name and histology diagnosis. Adenomatous polyps with tubulovillous histology or size > 1 cm or with high grade dysplasia were define as advance adenoma.
Among 140 patients with recorded endoscopy type, 49% of patients had colonoscopy with standard scope. All three endoscopists performed procedure using both scopes at the same rate (9 min median normal withdraw time as quality standard). Data and the predicted diagnosis were collected from patients who had colonoscopy by the same three endoscopists. Bowel preparation was good and moderate in 95% and 5% of patients, respectively. The procedures were performed under a nurse administered standard sedation with Fentanyl and Midazolam. Colonoscopy withdrawal times were recorded by the nursing staff. Polyps were removed using forceps biopsy, and sent for histological analysis by the pathologist who was not aware of the endoscopic diagnosis.
We compared the demographic and clinical characteristics between a group of patients who underwent standard colonoscopy vs NBI by Student’s t-test to χ2 whichever was appropriate. For each method sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and, positive likelihood ratio (PLR) of colonoscopy diagnosis was calculated with comparison to pathologic diagnosis as gold standard. Calculation of 95% confidence interval and statistical comparison between two instruments was performed by established methods. All statistical analyses were performed using Stata 12.0 (Stata Corp., College park, TX, United States).
One hundred and forty seven adult patients were recruited and underwent colonoscopy during a one year period. Among them 55 (37%) were male and median (range) of age was 56 (19-80). Among the patients “screened with” underwent standard scope, 31 (46%) had high school or lower education, while 37 (54%) had higher education, compared to 38 (54%) and 34 (46%) who underwent HD scope, respectively. Among the patients who underwent standard scope, 25 (37%) had previous colonoscopy, which 6 of them (9%) had previous history of polyp, while these numbers for the patients underwent HD scope were 19 (26%) and 7 (10%) respectively. Also 22 patients (22%) underwent standard scope had a family history of colon cancer, while this number for HD scope with NBI was 12 (17%). The most common reason for colonoscopy with both scopes was screening, 50% of the patients underwent standard scope and 62% of the patients underwent HD scope. Table 1 compares the characteristics of patients underwent standard scope vs HD scope with NBI.
| Parameters | Standard scope (1) (n = 68) | HD scope (n = 72) | P value |
| Female | 41 (60) | 48 (67) | 0.40 |
| Age (yr), median (IQR) | 56 (52-61) | 57 (53-64) | 0.70 |
| Education | 0.40 | ||
| High school and lower | 31 (46) | 38 (54) | |
| > High school | 37 (54) | 34 (47) | |
| H/o previous colonoscopy | 25 (37) | 19 (26) | 0.20 |
| H/o previous colon polyp | 6 (9) | 7 (10) | 0.80 |
| Family h/o colon cancer | 22 (22) | 12 (17) | 0.40 |
| Indication | 0.20 | ||
| Screening | 34 (50) | 45 (63) | |
| Diagnostic | 18 (26) | 19 (26) | |
| Follow up | 16 (24) | 8 (11) | |
| Colon preparation | 0.08 | ||
| Good | 63 (93) | 71 (99) | |
| Moderate | 5 (7) | 1 (1) | |
| Number of patient with polyp diagnosis | 41 (60) | 49 (68) | 0.30 |
| Total number of polyps detected, median (IQR) | 1 (1-2)1 | 2 (1-3)2 | 0.20 |
| Adenoma detection rate | 23 (34) | 32 (44) | 0.20 |
| Advanced adenoma detection rate | 7 (10) | 8 (11) | 0.90 |
| Hyperplastic polyp detection rate | 19 (28) | 21 (29) | 0.90 |
| Proportion of patients with multiple polyps | 17 (41)1 | 28 (57)2 | 0.10 |
Colonoscopies were done by standard (49%) and HD (51%) scopes. Among 147 patients, 57 patients (39%) had normal colonoscopy. Number of patients diagnosed with any type of polyp were 41(60%) using standard scope and 49 (68%) using HD scope (P = 0.3). Among all 90 patients with polyps, 179 polyps were removed. The median (range) of polyp number in a patient was 2 (1-5) and was not significantly different between two scopes (P = 0.2). Among the polyps removed by standard scope, 89% were < 10 mm, compare to 87% for HD scope with NBI (P = 0.7). In lesions, the most frequent anatomic location was ascending colon (29%), followed by descending colon (18) and rectum (each 16%). This distribution was not different between both scopes (P = 0.5). The most frequent clinical diagnoses were hyper plastic polyp (HPP; 46%), adenoma (43%) and diminutive (11%). Tables 2 and 3 indicate the clinical value of colonoscopy diagnosis for adenoma and HPP when compared to the corresponding pathologic diagnosis.
| Sensitivity (%) | Specificity (%) | PPV (%)(true positive/all positive) | NPV (%)(true negative/all negative) | PLR (%)(true positive/false positive) | |
| ALL | 61 (51-70) | 79 (69-86) | 78 (68-86) | 62 (53-71) | 2.9 (1.8-4.5) |
| Scope 1 | 53 (39-67) | 87 (70-95) | 86 (69-94) | 55 (41-69) | 4.0 (1.5-10.4) |
| Scope 2 | 68 (55-79) | 74 (60-84) | 74 (60-84) | 69 (55-79) | 2.6 (1.6-4.3) |
| P value for two scopes | 0.1 | 0.2 | 0.2 | 0.1 |
| Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | PLR (%) | |
| All | 73 (59-84) | 63 (55-71) | 40 (30-51) | 88 (79-93) | 2.0 (1.5-2.6) |
| Scope 1 | 74 (51-88) | 59 (46-71) | 38 (24-54) | 87 (73-94) | 1.8 (1.2-2.7) |
| Scope 2 | 74 (54-86) | 66 (55-76) | 42 (29-57) | 88 (77-94) | 2.2 (1.5-3.2) |
| P value for two scopes | 0.9 | 0.4 | 0.7 | 0.9 |
Adenoma detection rate and advanced adenoma detection rate were not significantly different between two scopes (Table 1). Standard scope has a sensitivity of 53% and specificity of 87% in detecting adenoma, compared to 68%, 74% for HD scope with NBI, respectively. Standard scope has a higher specificity, but HD scope with NBI has a higher sensitivity in detecting adenoma. Positive likelihood ratio for standard scope is higher than HD scope with NBI (4 compare to 2.6; Table 2).
HPP detection rate for standard scope and HD was 28% and 21%, respectively (P = 0.9, Table 1). Standard scope has a sensitivity of 74% and specificity of 59% in detecting HPP, compared to 74% and 66% for HD scope, respectively. Both scopes don’t show significant difference in detecting HPP. Positive likelihood ratio for HD scope with NBI is slightly higher than standard scope (2.2 compare to 1.8; Table 4).
| Parameters | Standard scope (1) (n = 75) | HD scope (2) (n = 103) | P value |
| Polyps < 10 mm in size | 67 (89) | 89 (87) | 0.7 |
| Adenoma detection rate | 45 (60) | 53 (51) | 0.3 |
| Hyperplastic polyp detection rate | 19 (25) | 26 (25) | 0.9 |
Endoscopist 1 has a higher sensitivity in detecting adenoma (70%) followed by endoscopist 2 (60%) and endoscopoist 3 (52%) regardless of the type of scope. Endoscopist 1 also has a higher accuracy in detecting adenoma (PLR = 6.3%) compared to the other two endoscopists (2.8 and 1.8 for endoscopists 2 and 3 respectively) regardless of the type of scope (Table 5).
| Parameter | Sensitivity | Specificity | PPV | NPV | PLR |
| Endoscopist 1 | 75 (55-88) | 88 (70-96) | 86 (65-95) | 79 (61-90) | 6.3 (2.1-18.5) |
| Endoscopist 2 | 60 (46-74) | 78 (58-90) | 84 (67-93) | 51 (34-67) | 2.8 (1.2-6.3) |
| Endoscopist 3 | 52 (35-68) | 72 (55-84) | 64 (45-80) | 61 (45-74) | 1.8 (0.4-1.0) |
| P value for three endoscopists | 0.2 | 0.3 | 0.1 | 0.1 |
Endoscopist 1 has lower sensitivity (53%) but higher accuracy (PLR = 3.4%) in detecting HPP compared to the other two endoscopists, regardless of the type of scope. Endoscopist 2 has the highest sensitivity (91%) in detecting HPP, regardless of the type of scope (Table 6).
| Parameter | Sensitivity | Specificity | PPV | NPV | PLR |
| Endoscopist 1 | 53 (32-73) | 83 (66-93) | 67 (42-85) | 74 (57-85) | 3.2 (1.3-7.8) |
| Endoscopist 2 | 91 (62-98) | 56 (43-69) | 29 (17-46) | 97 (84-99) | 2.1 (1.5-3.0) |
| Endoscopist 3 | 87 (62-96) | 58 (44-71) | 39 (25-56) | 93 (79-98) | 2.1 (1.4-3.1) |
| P value for three endoscopists | 0.026 | 0.033 | 0.049 | 0.008 |
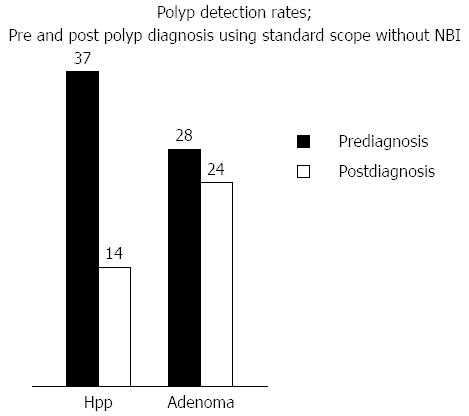
Out of 28 adenoma “diagnosed in real time” prediagnosis using standard scope without NBI, 24 were matched to the histology report (PPV = 86%). For HPP, these numbers were 37, with 14 matched to the histology report (PPV = 38%; Figure 1).
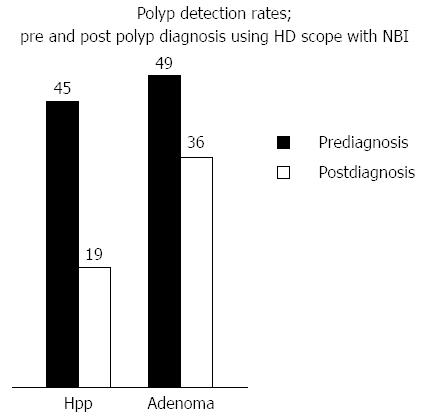
Out of 49 adenoma prediagnosis using HD scope with NBI, 36 were matched to the histology report (PPV = 74%). For HPP, these numbers were 45, with 19 matched to the histology report (PPV = 42%; Figure 2).
The standard white light colonoscopy does not have the ability to accurately distinguish between adenomatous and hyperplastic polyps[10]. This distinction has an important clinical impact as adenomatous polyps are considered neoplastic whereas hyperplastic polyps are benign and don’t have a malignant potential. Although the removal of adenomatous polyps is recommended since it disrupts the adenoma-carcinoma sequence and prevents from the development of colorectal cancer, hyperplastic polyps can safely be left behind without significant consequences[10]. The removal of hyperplastic polyps could be avoided with real-time identification of polyp type during colonoscopy, leading to a decrease of the procedure duration, costs and risk of complications[10]. Studies found a conflicting results comparing the accuracy of standard scope vs NBI scope in detection of polyps and prediction of histology in real time[8,11-13]. Some trials findings favored the standard scope, others the NBI scope whereas some studies did not reveal any difference between both scopes.
Sabbagh et al[11] conducted a randomized controlled trial and meta-analysis of published studies comparing the narrow-band imaging to conventional colonoscopy in detection of colorectal polyps. A total of 482 patients were included, 241 into the intervention (NBI) colonoscopy and 241 into the conventional colonoscopy group[11]. No significant difference was found in the mean number of polyps when comparing the conventional procedure to the NBI system (0.41 vs 0.29). The overall detection rate of lesions (n = 174) and polyps (n = 169) by histological examination per patient in the entire study group were 36.1% and 35.1% respectively, with adenomas and hyperplastic polyps found, respectively, in 55.0% (n = 93/169) and 37.9% (n = 64/169) of all patients. In this study[11], the overall rate of polyp detection was significantly higher in the conventional group compared to the NBI group (RR = 0.75, 95%CI: 0.60-0.96). The results of Sabbagh et al[11] are different than our results. In our study, there was no difference in the rate of polyps detection between the standard scope and NBI with 41 (60%) patients diagnosed with any type of polyp using standard scope and 49 (68%) using HD/NBI scope (P = 0.3). The median (range) of polyp number in a patient was 2 (1-5) and was not significantly different between two scopes (P = 0.2), this difference could be attributed to the sample size and study population. In our trial included a total of 147 patient and all were African Americans, also the white-light group, in Sabbagh et al[11]’s study, could have had better mucosal visualization during the withdrawal phase compared to that of the NBI group because of the darkening of the image associated with the use of NBI. This may have led to the finding of significantly greater number of polyps found in the white-light group. In addition, one third of patients had less than excellent colon preparation, which may have contributed to the poorer performance of the NBI visualization. Sabbagh et al[11] also performed a systemic review of the current evidence including 7 randomized control trials which showed no significant differences among groups in the mean number of polyps, the mean number of adenomas, and the rates of patients with at least one polyp or one adenoma. Two randomized control trials revealed a significant difference in the mean rate of adenomas detection in favor of the NBI group[14,15]. One trial reported a significantly higher detection in the mean number of flat adenomas in the NBI group[16], while other study demonstrated the opposite[17] and two other trials did not find any significant difference between the standard scope and the NBI[18,19].
Another metanalysis of 9 randomized control trials compared the yield and miss rate of narrow band imaging and white light endoscopy in patients undergoing screening or surveillance colonoscopy[8]. There was no significant difference between high-definition narrow-band imaging (HD-NBI) and high-definition white light endoscopy (HD-WLE) for the detection of adenomas (OR = 1.01, 95%CI: 0.74-1.37; Ι2 = 60%; six RCTs) or for the detection of patients with polyps, patients with adenomas, the detection of adenomas over 10 mm, flat adenomas and flat adenomas per patient[8]. There was no significant difference for HD-NBI vs HD-WLE in polyp miss rate (OR = 1.17, 95%CI: 0.80-1.71; Ι2 = 50%; three randomized control trials) or adenoma miss rate (OR = 0.65, 95%CI: 0.40-1.06; Ι2 = 10%; three randomized control trials)[8]. These results are consistent with ours, however, our study did not evaluate the miss rate.
A prospective trial of 302 patients compared standard broadband white light colonoscopy with narrow-band imaging for the differentiation of colorectal polyps during real-time colonoscopy by using a modified Kudo pit pattern classification and vascular color intensity grading[20]. Overall, NBI accuracy was 80% compared with 77% for white light alone[20]. NBI performed significantly better than white light in diagnosing adenomas (sensitivity 80% vs 69%), particularly for adenomas ≤ 5 mm (75% vs 60%)[20]. There was no difference between NBI and white light for nonadenomatous polyps[20]. These findings are consistent with our results (sensitivity 68% vs 53% for NBI and Standard scope respectively). The diagnostic accuracies in this study[20] were better for larger polyps. Compared with white light, however, NBI did not significantly improve accuracy in any size or shape category, nor for any segment of the colon. In our study the most frequent anatomic location of the lesions was ascending colon (29%), followed by descending colon (18%) and rectum (each 16%). This distribution was not different between two scopes as well (P = 0.5). The researchers in this study[20] repeated the trial after training the endoscopists in detection and differentiation between different types of polyps. An equal number of polyps were analyzed in each of the two study periods (133 and 132, respectively). NBI accuracies significantly improved from 74% to 87% between the two study periods however, white light accuracies did not change (78% first half and 79% second half). After the learning curve was reached, NBI was significantly more accurate than white light[20]. The studies demonstrated that there is a learning curve with regard to NBI assessment of colorectal polyps, and that NBI performs better than the ordinary broadband white light once this ‘’learning’’ is achieved[20].
A recent systematic review and meta-analysis on the real-time diagnostic operating characteristics of NBI colonoscopy included 28 studies with a total of 6280 polyps diagnosed in 4053 patients[13]. Endoscopic diagnosis of colorectal polyps with NBI showed highly accurate diagnostic performance, the area under the HSROC curve was 0.92 (95%CI: 0.90-0.94). The overall sensitivity of NBI diagnosis was 91.0% (95%CI: 87.6%-93.5%) and specificity was 82.6% (95%CI: 79.0%-85.7%) compared with histology[13]. The sensitivity and specificity of diagnosis of diminutive polyps, made with high confidence was 93.4% (95%CI: 87.4%-96.7%) and 84.0% (95%CI: 76.6%-89.3%), respectively[13]. The findings of this meta-analysis suggest that real-time endoscopic diagnosis of colorectal polyps performed using NBI has a high diagnostic performance[13]. Endoscopic diagnosis correctly characterized 91% of neoplasms and 83% of non-neoplastic polyps. This study addressed the standards set forth by the American Society of Gastrointestinal Endoscopy (ASGE) for the “resect and discard” strategy[12]. The summary agreement was 92.6% in this study[13], supporting the clinical use of such a strategy. In our study the sensitivity 68% and specificity 74% of the NBI were much lower as compared to the findings of McGill et al[13] meta analysis. This discrepancy could be related to the size of the population studied, however our project studied only a minority population African Americans.
The findings of our study have some limitations: the total number of polyps was relatively small 179 as compared to higher number in other studies. A sub group analysis for polyps ≤ 5 mm was not performed, the “resect and discard” strategy has been proposed by the ASGE for adenomas ≤ 5 mm in size without pathologic assessment when the endoscopic diagnosis provides a ≥ 90% agreement in assignment of postpolypectomy surveillance intervals compared with decisions based on pathology[12]. Interobserver variations were also noted, a possible training of the endoscopists prior to the use of the NBI could have improved the outcome. The cost saving for this approaches is substantial and was confirmed by Kessler et al[21]’s study. Based on the annual volume of colonoscopy in the United States, the annual up-front cost savings of forgoing the pathologic assessment would exceed a billion dollars[21].
Overall, the colonoscopy diagnosis is not yet fully matched with pathologic diagnosis of colon polyp. However with the advancement of both imaging and training, it may be possible to increase the sensitivity and specificity of the scopes and hence save money for eliminating time and the cost of Immunohistochemistry/pathology.
High definition colonoscopy (HD) with narrow band imaging (NBI) scope has advantage to detect vascular or mucosal characteristics so that any abnormal growth could be better visualized and diagnosed than standard colonoscopy.
Diagnostic accuracy using HD scope with NBI is cost saving as it eliminates and/or decreases the volume of specimens that need pathology assessment and diagnosis, especially for polyps < 1 cm.
The results of present study indicate that HD-NBI scope more sensitive for adenoma diagnosis than standard scope colonoscopy.
High definition with narrow band imaging scope correspond to improvements in the resolution of imaging techniques in colonoscopy, that increases the accuracy of diagnosis using narrow-band width filters in a red-green-blue sequential illumination system. It improves the detailed visualization of the micro vascular and micro structural colon pit in patterns.
The present study presents the differences between two advanced explorations with different levels of viewing the pathological target, which are colon polyps. The exposure mode, of the differences between the two techniques is in accordance with the standards of a well written article.
Manuscript Source: Invited manuscript
Specialty Type: Gastroenterology and Hepatology
Country of Origin: United States
Peer-Review Report Classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Porumb V S- Editor: Yu J L- Editor: A E- Editor: Ma S
| 1. | Jemal A, Simard EP, Dorell C, Noone AM, Markowitz LE, Kohler B, Eheman C, Saraiya M, Bandi P, Saslow D. Annual Report to the Nation on the Status of Cancer, 1975-2009, featuring the burden and trends in human papillomavirus(HPV)-associated cancers and HPV vaccination coverage levels. J Natl Cancer Inst. 2013;105:175-201. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 729] [Cited by in F6Publishing: 753] [Article Influence: 68.5] [Reference Citation Analysis (0)] |
| 2. | Schrock TR. Colonoscopy for colorectal cancer: too much, too little, just right. ASGE Distinguished Lecture 1993. Gastrointest Endosc. 1993;39:848-851. [PubMed] [Cited in This Article: ] |
| 3. | Seeff LC, Richards TB, Shapiro JA, Nadel MR, Manninen DL, Given LS, Dong FB, Winges LD, McKenna MT. How many endoscopies are performed for colorectal cancer screening? Results from CDC’s survey of endoscopic capacity. Gastroenterology. 2004;127:1670-1677. [PubMed] [Cited in This Article: ] |
| 4. | Seeff LC, Manninen DL, Dong FB, Chattopadhyay SK, Nadel MR, Tangka FK, Molinari NA. Is there endoscopic capacity to provide colorectal cancer screening to the unscreened population in the United States? Gastroenterology. 2004;127:1661-1669. [PubMed] [Cited in This Article: ] |
| 5. | Butterly LF, Chase MP, Pohl H, Fiarman GS. Prevalence of clinically important histology in small adenomas. Clin Gastroenterol Hepatol. 2006;4:343-348. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 200] [Cited by in F6Publishing: 188] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 6. | Singh R, Owen V, Shonde A, Kaye P, Hawkey C, Ragunath K. White light endoscopy, narrow band imaging and chromoendoscopy with magnification in diagnosing colorectal neoplasia. World J Gastrointest Endosc. 2009;1:45-50. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 20] [Cited by in F6Publishing: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Rex DK, Cutler CS, Lemmel GT, Rahmani EY, Clark DW, Helper DJ, Lehman GA, Mark DG. Colonoscopic miss rates of adenomas determined by back-to-back colonoscopies. Gastroenterology. 1997;112:24-28. [PubMed] [Cited in This Article: ] |
| 8. | Pasha SF, Leighton JA, Das A, Harrison ME, Gurudu SR, Ramirez FC, Fleischer DE, Sharma VK. Comparison of the yield and miss rate of narrow band imaging and white light endoscopy in patients undergoing screening or surveillance colonoscopy: a meta-analysis. Am J Gastroenterol. 2012;107:363-370; quiz 371. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 113] [Cited by in F6Publishing: 120] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 9. | Machida H, Sano Y, Hamamoto Y, Muto M, Kozu T, Tajiri H, Yoshida S. Narrow-band imaging in the diagnosis of colorectal mucosal lesions: a pilot study. Endoscopy. 2004;36:1094-1098. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 387] [Cited by in F6Publishing: 359] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 10. | Rastogi A, Keighley J, Singh V, Callahan P, Bansal A, Wani S, Sharma P. High accuracy of narrow band imaging without magnification for the real-time characterization of polyp histology and its comparison with high-definition white light colonoscopy: a prospective study. Am J Gastroenterol. 2009;104:2422-2430. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 136] [Cited by in F6Publishing: 125] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 11. | Sabbagh LC, Reveiz L, Aponte D, de Aguiar S. Narrow-band imaging does not improve detection of colorectal polyps when compared to conventional colonoscopy: a randomized controlled trial and meta-analysis of published studies. BMC Gastroenterol. 2011;11:100. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Rex DK, Kahi C, O’Brien M, Levin TR, Pohl H, Rastogi A, Burgart L, Imperiale T, Ladabaum U, Cohen J. The American Society for Gastrointestinal Endoscopy PIVI (Preservation and Incorporation of Valuable Endoscopic Innovations) on real-time endoscopic assessment of the histology of diminutive colorectal polyps. Gastrointest Endosc. 2011;73:419-422. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 406] [Cited by in F6Publishing: 428] [Article Influence: 32.9] [Reference Citation Analysis (0)] |
| 13. | McGill SK, Evangelou E, Ioannidis JP, Soetikno RM, Kaltenbach T. Narrow band imaging to differentiate neoplastic and non-neoplastic colorectal polyps in real time: a meta-analysis of diagnostic operating characteristics. Gut. 2013;62:1704-1713. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 123] [Cited by in F6Publishing: 124] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 14. | Kaltenbach T, Friedland S, Soetikno R. A randomised tandem colonoscopy trial of narrow band imaging versus white light examination to compare neoplasia miss rates. Gut. 2008;57:1406-1412. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 122] [Cited by in F6Publishing: 129] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 15. | Inoue T, Murano M, Murano N, Kuramoto T, Kawakami K, Abe Y, Morita E, Toshina K, Hoshiro H, Egashira Y. Comparative study of conventional colonoscopy and pan-colonic narrow-band imaging system in the detection of neoplastic colonic polyps: a randomized, controlled trial. J Gastroenterol. 2008;43:45-50. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 113] [Cited by in F6Publishing: 122] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 16. | East JE, Ignjatovic A, Suzuki N, Guenther T, Bassett P, Tekkis PP, Saunders BP. A randomized, controlled trial of narrow-band imaging vs high-definition white light for adenoma detection in patients at high risk of adenomas. Colorectal Dis. 2012;14:e771-e778. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | Adler A, Aschenbeck J, Yenerim T, Mayr M, Aminalai A, Drossel R, Schröder A, Scheel M, Wiedenmann B, Rösch T. Narrow-band versus white-light high definition television endoscopic imaging for screening colonoscopy: a prospective randomized trial. Gastroenterology. 2009;136:410-416.e1; quiz 715. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 137] [Cited by in F6Publishing: 157] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 18. | Paggi S, Radaelli F, Amato A, Meucci G, Mandelli G, Imperiali G, Spinzi G, Terreni N, Lenoci N, Terruzzi V. The impact of narrow band imaging in screening colonoscopy: a randomized controlled trial. Clin Gastroenterol Hepatol. 2009;7:1049-1054. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 78] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 19. | Rex DK, Helbig CC. High yields of small and flat adenomas with high-definition colonoscopes using either white light or narrow band imaging. Gastroenterology. 2007;133:42-47. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 291] [Cited by in F6Publishing: 310] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 20. | Rogart JN, Jain D, Siddiqui UD, Oren T, Lim J, Jamidar P, Aslanian H. Narrow-band imaging without high magnification to differentiate polyps during real-time colonoscopy: improvement with experience. Gastrointest Endosc. 2008;68:1136-1145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 92] [Cited by in F6Publishing: 92] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 21. | Kessler WR, Imperiale TF, Klein RW, Wielage RC, Rex DK. A quantitative assessment of the risks and cost savings of forgoing histologic examination of diminutive polyps. Endoscopy. 2011;43:683-691. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 110] [Cited by in F6Publishing: 116] [Article Influence: 8.9] [Reference Citation Analysis (0)] |