Published online Apr 7, 2016. doi: 10.3748/wjg.v22.i13.3558
Peer-review started: October 12, 2015
First decision: November 5, 2015
Revised: November 9, 2015
Accepted: December 14, 2015
Article in press: December 14, 2015
Published online: April 7, 2016
Processing time: 168 Days and 15.2 Hours
AIM: To apply the laparoscopic and endoscopic cooperative surgery concept, we investigated whether endoscopic cholecystectomy could be performed more safely and rapidly via only 1 port or not.
METHODS: Two dogs (11 and 13-mo-old female Beagle) were used in this study. Only 1 blunt port was created, and a flexible endoscope with a tip attachment was inserted between the fundus of gallbladder and liver. After local injection of saline to the gallbladder bed, resection of the gallbladder bed from the liver was performed. After complete resection of the gallbladder bed, the gallbladder was pulled up to resect its neck using the Ring-shaped thread technique. The neck of the gallbladder was cut using scissor forceps. Resected gallbladder was retrieved using endoscopic net forceps via a port.
RESULTS: The operation times from general anesthetizing with sevoflurane to finishing the closure of the blunt port site were about 50 min and 60 min respectively. The resection times of gallbladder bed were about 15 min and 13 min respectively without liver injury and bleeding at all. Feed were given just after next day of operation, and they had a good appetite. Two dogs are in good health now and no complications for 1 mo after endoscopic cholecystectomy using only a flexible endoscope via one port.
CONCLUSION: We are sure of great feasibility of endoscopic cholecystectomy via single port for human.
Core tip: Endoscopic cholecystectomy via single port is a safety and reliable new flexible endoscopic surgery. Local injection of saline to the gallbladder bed makes it easier to resect the gallbladder bed from the liver. After complete dissection of the gallbladder bed, the neck of the gallbladder was clipped and cut safer and easier using ring-shaped thread method.
- Citation: Mori H, Kobayashi N, Kobara H, Nishiyama N, Fujihara S, Chiyo T, Ayaki M, Nagase T, Masaki T. Novel and safer endoscopic cholecystectomy using only a flexible endoscope via single port. World J Gastroenterol 2016; 22(13): 3558-3563
- URL: https://www.wjgnet.com/1007-9327/full/v22/i13/3558.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i13.3558
In 2004, since Kalloo et al reported a study on the observation of abdominal cavity through stomach using oral flexible endoscope following incision of the stomach, natural orifice translumenal endoscopic surgery (NOTES) using flexible endoscope has attracted attention as a minimally invasive surgical method[1-4]. It was impossible to suddenly succeed in developing a surgical method equivalent to laparoscopic surgery from the viewpoint of safety. On the other hand, laparoscopy and endoscopy cooperative surgery (LECS) was rapidly developed in Japan for the partial gastrectomy of gastric and duodenal tumors[5-9]. LECS is based on excellent concept of the combination and collaboration with endoscopist and surgeon, in other words, taking advantages of both flexible and rigid endoscopes to achieve super minimal invasive surgery.
By using the LECS concept and the technique of endoscopic submucosal dissection (ESD), we investigated whether endoscopic cholecystectomy could be performed more safely and rapidly via only single port or not.
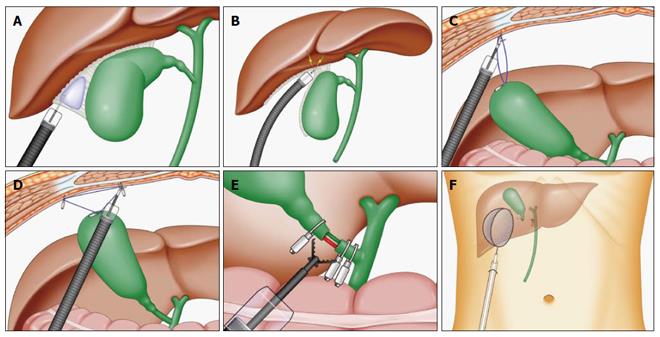
Only 1 blunt port was created, and a flexible endoscope with a tip attachment was inserted between the fundus of gallbladder and liver easily. Local injection of saline to the gallbladder bed enabled us to easily obtain sufficient space (Figure 1A). Resection of the gallbladder from the liver was performed without any damage or bleeding (Figure 1B). After complete resection of the gallbladder bed, the gallbladder was pulled up to resect its neck. A ring-shaped thread was placed via an endoscopic channel using grasping forceps. One side of the ring was clipped to the fundus of the gallbladder and the other to the abdominal wall (Figure 1C). The third clip was hooked to 1 side of the ring-shaped thread. The thread was hooked crosswise to the 2 supporting points of the gallbladder and abdominal wall and clipped (Figure 1D). The neck of the gallbladder was cut using scissor forceps (Figure 1E). Resected gallbladder was retrieved using endoscopic net forceps via a port (Figure 1F).
Two dogs (11 and 13-mo-old female Beagle) were used in this study (Hokuzan Rabesu Co., Nagano, Japan). Animal experiments were performed in the Preclinical Animal Laboratory of Kagawa University, Japan. A dog was maintained in a pathogen-free facility under controlled temperature (24 ± 2 °C) and humidity (55% ± 5%), with a 12-h light/dark cycle. All experimental procedures were performed according to the guidelines for the care and use of animals as established by Kagawa University.
The items examined were as follows: (1) The operation success rate with long survival; (2) The operation times from general anesthetizing to finishing the closure of the blunt port site; and (3) The resection times of gallbladder bed.
Endoscopes: OLYMPUS GIF TYPE Q260J (Olympus Co. Tokyo, Japan). CO2 insufflation device: OLYMPUS UCR (Olympus Co. Tokyo, Japan); Endoscopic knives: Dual knife (KD-650L, Olympus Co. Tokyo, Japan); Generator device: ERBE VIO300D (Elektromedizin, Tübingen, Germany).
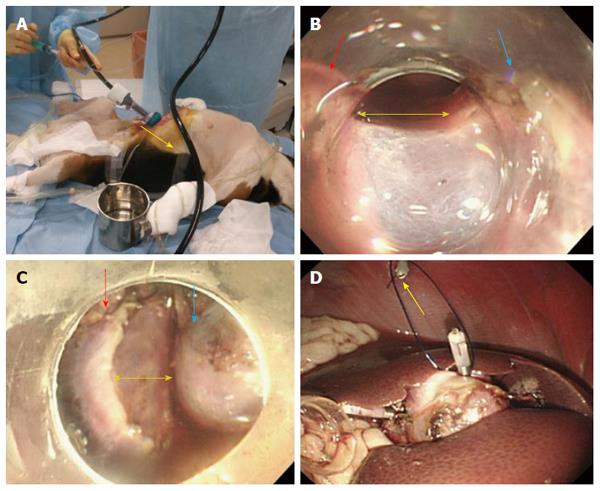
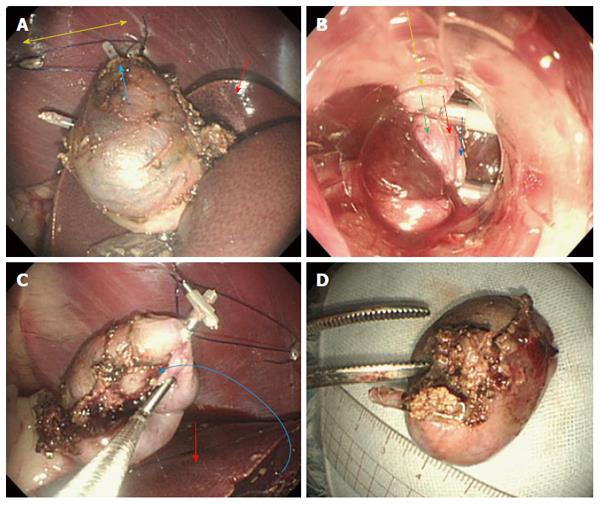
Under general anesthesia, only 1 port (12 mm in diameter) was inserted using an open technique (Figure 2A). A flexible endoscope with a tip attachment was inserted between the fundus of gallbladder and liver, and a layer of loose connective tissue was opened. Local injection of saline to the loose layer enabled us to easily obtain sufficient space and dissect the gallbladder from the liver without any damage or bleeding (Figure 2B). After complete dissection of the gallbladder bed (Figure 2C), the gallbladder was pulled up to dissect its neck. A 3-0 absorbable ring-shaped thread was placed via an endoscopic channel using grasping forceps. One side of the ring was clipped to the fundus of the gallbladder and the other to the abdominal wall (Figure 2D). The third clip was hooked to 1 side of the ring-shaped thread. The thread was hooked crosswise to the 2 supporting points of the gallbladder and abdominal wall and clipped (Figure 3A). After the neck of the gallbladder was cut using scissor forceps extending it and placing 2 clips on the central side and 1 clip on the peripheral side (Figure 3B), successful resection of the gallbladder was completed (Figure 3C). Resected gallbladder bed was very smooth without blood (Figure 3D).
The operation times from general anesthetizing with sevoflurane to finishing the closure of the blunt port site were about 50 min and 60 min respectively. The resection times of gallbladder bed were about 15 min and 13 min respectively without liver injury and bleeding at all. Feed were given just after next day of operation, and they had a good appetite.
Two dogs are in good health now and no complications for 1 mo after endoscopic cholecystectomy using only a flexible endoscope via one port.
Laparoscopic cholecystectomy (LC) has been established and performed safely all over the world[10,11]. As LC is safe and well-established surgical procedure, it needs to create 4 ports (5 mm-3 ports in right hypochondriac region, 12 mm-1 blunt (camera) port in the umbilical portion). Although high volume centers are able to perform single port laparoscopic cholecystectomy (SP-LC) safely, it is still challenging, limited and risky for surgeon to perform SP-LC in the city hospital[12]. In this experiment, to create 12 mm-1 ports in right hypochondriac region made it possible to complete flexible endoscopic cholecystectomy very easy and safety. When a flexible endoscope with a tip attachment was inserted between the gallbladder and liver, a layer of loose connective tissue was opened very easily. Moreover, local injection of saline to the loose layer to obtain sufficient space and dissect the gallbladder bed more safely. After complete dissection of the gallbladder bed, the neck of the gallbladder was clipped and cut using scissor forceps easily. The Ring-shaped thread technique was very useful to pull up the gallbladder and resect its neck. Endoscopic cholecystectomy using only one flexible endoscope via single port was as safe and feasible as laparoscopic cholecystectomy.
There are 3 advantageous points in this procedure (EC). We described these advantages as follows: (1) Reduction of port: In general, we perform laparoscopic cholecystectomy creating 4 ports by open technique (1 blunt port 12 mm in diameter in umbilical portion which is used to insert a rigid endoscopic camera and make pneumoperitoneum to keep stable pressure, 1 port 12 mm in diameter in epigastric region, 2 port 5 mm in diameter in Rt. hypochondriac regions to assist pulling up the fundus of the GB). In this technique (EC), the most innovative points are not only to approach to the GB via single blunt port in Rt. hypochondriac region and make pneumoperitoneum keeping stable pressure, but also to use functional advantages of flexible endoscope such as cleaning its lens function, water jet function and manual insufflation/deflation function under stable pressure by pneumoperitoneum system of the blunt port. The concept of this technique (EC) isn’t similar to the NOTES at all, but LECS concept which approached via port created at the abdominal wall. This procedure (EC) requires only 1 port via abdominal wall without perforation of the gut wall to approach the abdominal cavity and GB bed; (2) Direction of approach to the GB: Single incision laparoscopic surgery (SILS) needs higher surgical technique than this technique using a flexible endoscope. This is because the approach direction by SILS is from the perpendicular direction to the GB bed, and this makes it difficult to resect GB without minor injury and bleeding of the liver. On the other hand, in the EC procedure, we can approach the GB bed from the parallel direction. It is very easy to inject the natural saline to the GB bed and dissect it using attachment from parallel direction by a flexible endoscope using endoscopic submucosal dissection (ESD) method; and (3) The Ring-shaped thread technique: After dissected GB bed, it is difficult to obtain clear surgical view at the Calot triangle. However, the ring thread is inserted into the GB through the endoscopic channel using grasping forceps. After clipped at 2 points, the third clip hooks 1 side of the ring thread and slides the thread crosswise to pull up the GB and is then clipped.
In this study, there are several limitations as follows and needed more animal experiments to confirm safety of EC: (1) Small number experiments; and (2) EC requires endoscopist to learn the anatomy of only the Calot triangle and its anomaly.
We are sure of the feasibility of this surgical procedure “endoscopic cholecystectomy via single port’’ for human.
We would like to thank Dr. Makoto Oryu for technical and editorial assistance.
As natural orifice translumenal endoscopic surgery (NOTES) using flexible endoscope has been expected as a minimally invasive surgery, it was difficult to perform NOTES equivalent to laparoscopic surgery from the viewpoint of safety. Recently, laparoscopic and endoscopic cooperative surgery (LECS) was rapidly developed in Japan for the partial gastrectomy, which is based on excellent concept of the combination and collaboration with endoscopist and surgeon.
As the LECS was an excellent surgical concept, the authors applied the LECS concept for endoscopic cholecystectomy using only one flexible endoscope via single port.
Local injection of saline to the gallbladder bed made it possible to resect the gallbladder bed more rapidly and safely. The Ring-shaped thread technique was very useful to pull up the gallbladder and resect its neck.
Endoscopic cholecystectomy using only one flexible endoscope via single port was as safe and feasible as laparoscopic cholecystectomy.
Quite sure that the feasibility of this surgical procedure “endoscopic cholecystectomy via single port’’ for human.
P- Reviewer: Iizuka T, Neri V S- Editor: Yu J L- Editor: A E- Editor: Wang CH
| 1. | Fuchs KH, Meining A, von Renteln D, Fernandez-Esparrach G, Breithaupt W, Zornig C, Lacy A. Euro-NOTES Status Paper: from the concept to clinical practice. Surg Endosc. 2013;27:1456-1467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Autorino R, Yakoubi R, White WM, Gettman M, De Sio M, Quattrone C, Di Palma C, Izzo A, Correia-Pinto J, Kaouk JH. Natural orifice transluminal endoscopic surgery (NOTES): where are we going? A bibliometric assessment. BJU Int. 2013;111:11-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Mori H, Kobara H, Kobayashi M, Muramatsu A, Nomura T, Hagiike M, Izuishi K, Suzuki Y, Masaki T. Establishment of pure NOTES procedure using a conventional flexible endoscope: review of six cases of gastric gastrointestinal stromal tumors. Endoscopy. 2011;43:631-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Mori H, Kobara H, Nishiyama N, Fujihara S, Masaki T. Review of Pure Endoscopic Full-Thickness Resection of the Upper Gastrointestinal Tract. Gut Liver. 2015;9:590-600. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Imamura T, Komatsu S, Ichikawa D, Kobayashi H, Miyamae M, Hirajima S, Kawaguchi T, Kubota T, Kosuga T, Okamoto K. Gastric carcinoma originating from the heterotopic submucosal gastric gland treated by laparoscopy and endoscopy cooperative surgery. World J Gastrointest Oncol. 2015;7:118-122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Irino T, Nunobe S, Hiki N, Yamamoto Y, Hirasawa T, Ohashi M, Fujisaki J, Sano T, Yamaguchi T. Laparoscopic-endoscopic cooperative surgery for duodenal tumors: a unique procedure that helps ensure the safety of endoscopic submucosal dissection. Endoscopy. 2015;47:349-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Mori H, Kobara H, Tsushimi T, Fujihara S, Nishiyama N, Matsunaga T, Ayaki M, Yachida T, Tani J, Miyoshi H. Reduction effect of bacterial counts by preoperative saline lavage of the stomach in performing laparoscopic and endoscopic cooperative surgery. World J Gastroenterol. 2014;20:15763-15770. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Tsushimi T, Mori H, Harada T, Nagase T, Iked Y, Ohnishi H. Laparoscopic and endoscopic cooperative surgery for duodenal neuroendocrine tumor (NET) G1: Report of a case. Int J Surg Case Rep. 2014;5:1021-1024. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Hirokawa F, Hayashi M, Miyamoto Y, Asakuma M, Shimizu T, Komeda K, Inoue Y, Umegaki E, Uchiyama K. Laparoscopic and endoscopic cooperative surgery for duodenal tumor resection. Endoscopy. 2014;46 Suppl 1 UCTN:E26-E27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Wolfe BM, Gardiner B, Frey CF. Laparoscopic Cholecystectomy: A Remarkable Development. JAMA. 2015;314:1406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Wells KM, Lee YJ, Erdene S, Erdene S, Sanchin U, Sergelen O, Presson A, Zhang C, Rodriguez B, deVries C. Expansion of laparoscopic cholecystectomy in a resource limited setting, Mongolia: a 9-year cross-sectional retrospective review. Lancet. 2015;385 Suppl 2:S38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Chuang SH, Yang WJ, Chang CM, Lin CS, Yeh MC. Is routine single-incision laparoscopic cholecystectomy feasible? A retrospective observational study. Am J Surg. 2015;210:315-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |