Published online Dec 14, 2015. doi: 10.3748/wjg.v21.i46.13201
Peer-review started: July 30, 2015
First decision: August 26, 2015
Revised: September 9, 2015
Accepted: October 17, 2015
Article in press: October 20, 2015
Published online: December 14, 2015
Processing time: 141 Days and 0.2 Hours
Behçet’s disease (BD) is a multisystem autoimmune disorder characterized by recurrent orogenital ulcers, uveitis, and skin lesions. The vascular manifestations include thrombophlebitis, stenosis, occlusion, and pseudoaneurysm. BD infrequently precipitates aortic pseudoaneurysm rupture into the sigmoid mesocolon and lumen of the adjacent colon. Here we report an extremely rare case of spontaneous abdominal aortic pseudoaneurysm rupture via the sigmoid mesocolon into the lumen of the sigmoid colon in a 37-year-old patient with BD.
Core tip: Spontaneous abdominal aortic pseudoaneurysm rupture via the sigmoid mesocolon into the lumen of the sigmoid colon is a rare clinical manifestation. We report a case of a patient with Behçet’s disease who was successfully treated with stent grafting instead of surgical management.
- Citation: Lee SL, Ku YM, Won Y. Spontaneous aortic pseudoaneurysm rupture into the sigmoid colon in Behçet’s disease patient. World J Gastroenterol 2015; 21(46): 13201-13204
- URL: https://www.wjgnet.com/1007-9327/full/v21/i46/13201.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i46.13201
Behçet’s disease (BD) is an autoimmune disease associated with vasculitis. BD was originally described by the Turkish dermatologist Hulusi Behçet in 1937. BD is characterized by recurrent oral aphthous ulcers, genital lesions, and uveitis[1]. The vascular manifestations of BD are less frequent but are associated with increased mortality[1,2]. Venous thromboses and thrombophlebitis are more frequently observed vascular problems. However, major arterial complications such as stenosis, occlusion, aneurysm, and pseudoaneurysm can also occur[2,3]. There are currently no reports of spontaneous abdominal aortic pseudoaneurysm rupture into the sigmoid mesocolon and lumen of the sigmoid colon (causing lower gastrointestinal bleeding) in a BD patient. Thus, we report the first BD patient who presented with a spontaneous abdominal aortic pseudoaneurysm rupture via the sigmoid mesocolon into the lumen of the sigmoid colon. We performed stent-grafting treatment at our institution.
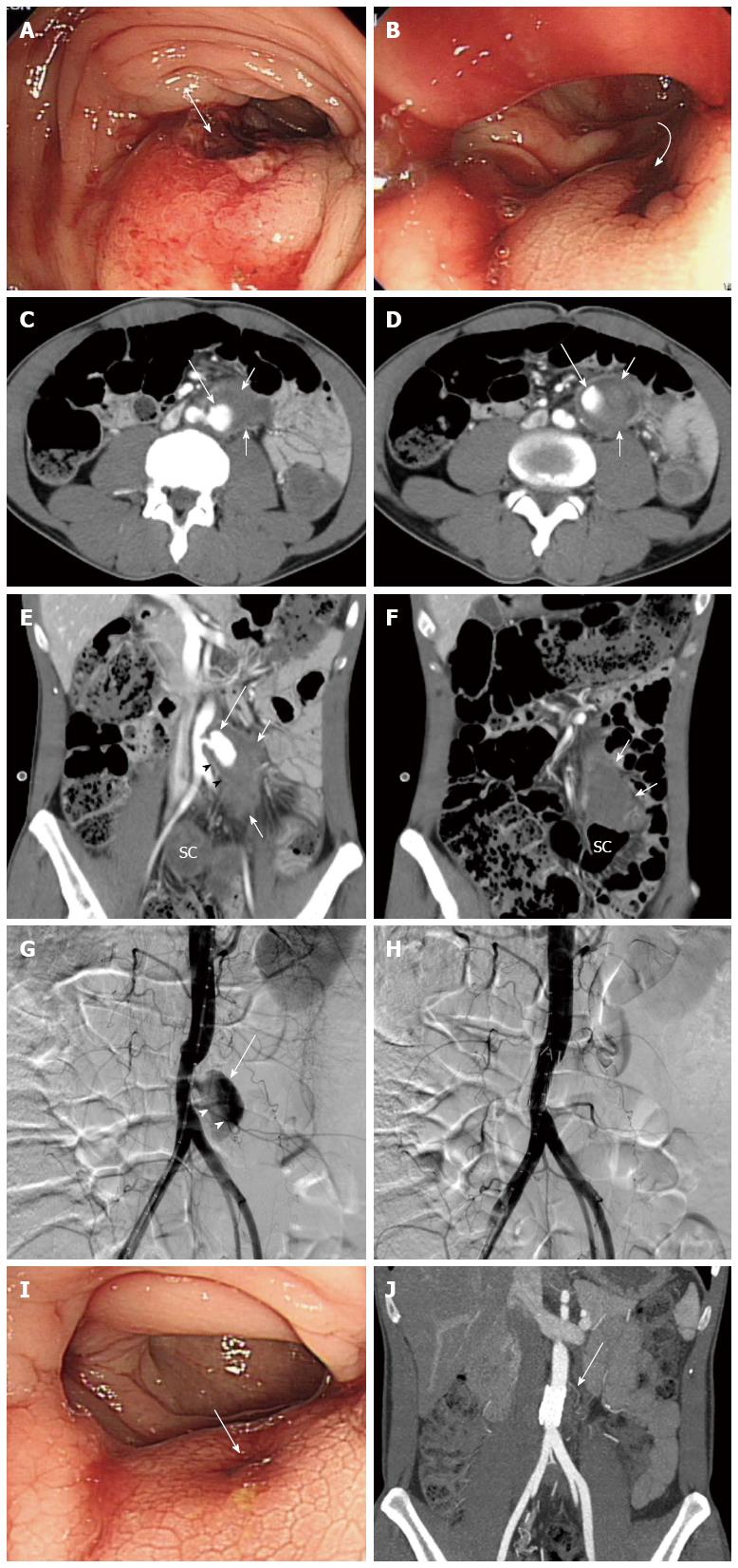
A 37-year-old male presented with recurrent episodes of oral and genital ulcers and a 1-d history of hematochezia. The patient was diagnosed with BD. A physical examination revealed tenderness in the lower abdomen. There was no palpable mass and no evidence of impaired peripheral perfusion. In the emergency department, the patient’s blood pressure at arrival was 100/75 mmHg, and the patient’s pulse at arrival was 109 beats/min. The laboratory investigations indicated the following results: creatinine, 1.32 mg/dL; C-reactive protein, 0.94 mg/dL; white blood cells, 10240/mm3; hemoglobin, 11.2 g/dL; and hematocrit, 32.9%. A preprocedural sigmoidoscopy revealed a submucosal tumor-like protrusion with a bleeding ulceration in the proximal sigmoid colon (Figure 1A and B). A computed tomography (CT) examination was performed to evaluate lower gastrointestinal bleeding using a 128-detector-row CT scanner (AS +, Siemens Medical Solutions, Forchheim, Germany). An enhanced CT of the abdomen revealed an enhanced pseudoaneurysm immediately above the origin site of the inferior mesenteric artery. Additionally, there was a hematoma extending into the subperitoneal space of the sigmoid mesocolon (Figure 1C-E). A hematoma was also noted in the lumen of the sigmoid colon (Figure 1E and F). A frontal abdominal aortogram revealed a pseudoaneurysm immediately above the origin site of the inferior mesenteric artery (Figure 1G). A stent-graft was inserted through the opening of the common femoral arteriotomy after angiographic evaluation. The 23 mm × 33 mm stent-graft (W.L. Gore & Associates, Flagstaff, AZ, United States) was covered with polytetrafluoroethylene. The stent length was sufficient to cover an area 2 cm proximal and distal to the pseudoaneurysm margin. After stent grafting, the pseudoaneurysm disappeared (Figure 1H). The patient was treated with antibiotics on the day of the procedure and then for 7 d to prevent stent graft infection. The follow-up sigmoidoscopy 4 d after the procedure revealed no evidence of active bleeding (Figure 1I). The CT angiography performed 6 mo after the procedure demonstrated complete remission of the aortic pseudoaneurysm and hematoma in the sigmoid mesocolon without evidence of graft infection (Figure 1J).
Cardiovascular involvement in BD occurs in 7%-29% of cases[2], and vein involvement is more common than arterial involvement[4]. The large arteries in BD patients may be involved in pseudoaneurysm formation, stenosis, or occlusion. These vascular complications frequently occur in the aorta and common iliac artery[1,4]. In BD patients, saccular pseudoaneurysm may be induced by transmural necrosis of the wall of the large muscular arteries by the occlusion of the vasa vasorum and perivascular inflammation. These changes result in the destruction of elastic fibers in the media and vascular wall perforation[1,5]. In the majority of cases, aortic pseudoaneurysms are confined to the great vessel space of the retroperitoneum. If a pseudoaneurysm in the lower abdominal aorta ruptures into the subperitoneal space then the hemorrhage can extend along the plane of the inferior mesenteric artery into the sigmoid mesocolon[6]. In our patient, enhanced CT revealed enhanced saccular outpouching arising from the abdominal aorta above the origin site of the inferior mesenteric artery. The hematoma extended into the sigmoid mesocolon, which suggests rupture.
An aorto-colic fistula is an extremely rare complication of infrarenal abdominal aortic aneurysm and can cause lower gastrointestinal bleeding[7-9]. The incidence of primary aorto-colic fistula is reported as low as 0.69%-2.36%[7]. The precise mechanism controlling aorto-colic fistula formation has not been elucidated. However, inflammation due to colonic diverticulitis and mechanical erosion represent possible antecedents[7,9]. In our patient, the abrasive effect of the pseudoaneurysm and hematoma in the sigmoid mesocolon resulted in transmural necrosis of the sigmoid colon wall.
There is frequently bleedings during both clinical and subclinical events in patients with aorto-enteric fistula[9]. The presence of air in the aneurysm and contrast media within the lumen of the colon on computed tomography are compatible with aorto-colic fistula[7,9]. Our patient had reduced air density inside the pseudoaneurysm and hematoma of the subperitoneal space. However, the mesocolic hematoma displaced the sigmoid colon. Blood clots (Hounsfield Unit density of > 30) were suspected inside the colon lumen and were suggestive of aorto-colic fistula. A sigmoidoscopy confirmed erosion and oozing blood clots at the top of the extrinsic indentation of the sigmoid colon.
Stent graft implantation is an accepted treatment for aortic pseudoaneurysms because it blocks blood flow from the aorta[1,2]. Surgical repair represents another treatment option. However, the high recurrence rate of pseudoaneurysms following surgery in BD patients may make clinicians reluctant to recommend surgical bypass operations[2,10]. After inserting the stent graft in our patient the blood flow to the pseudoaneurysm was blocked, which attenuated the lower gastrointestinal bleeding.
In conclusion, spontaneous aortic pseudoaneurysm rupture into the sigmoid colon via the mesocolon is an extremely rare cause of lower gastrointestinal bleeding. Although infrequently encountered, spontaneous aortic pseudoaneurysm rupture can be diagnosed early based on the findings of sigmoidoscopy and multidetector CT. The patient can be effectively treated using a stent graft.
A 37-year-old male diagnosed with Behcet’s disease presented hematochezia for 1 d.
The patient had massive lower gastrointestinal bleeding with large ulceration revealed by sigmoidoscopy.
Ulceration related with subepithelial gastrointestinal tumor and aortic pseudoaneurysm rupture with aortoenteric fistula
All labs were within normal limits except for mildly elevated white blood cell counts.
Enhanced computed tomography revealed an enhanced pseudoaneurysm immediately above the origin site of the inferior mesenteric artery. There was a hematoma extending into the subperitoneal space of the sigmoid mesocolon.
A stent graft of the aortic pseudoaneurysm associated with aortoenteric fistula.
Cardiovascular involvement in Behçet’s disease with vein involvement is more common than arterial involvement. The large arteries in Behçet’s disease patients may be involved in pseudoaneurysm formation, stenosis, or occlusions that frequently occur in the aorta and common iliac artery
Spontaneous aortic pseudoaneurysm rupture into the sigmoid colon via the mesocolon in Behçet’s disease patient is an extremely rare cause of lower gastrointestinal bleeding and can be effectively treated with stent grafting instead of surgical management.
Aortic pseudoaneurysm rupture into the sigmoid colon in a patient with Behçet’s disease is a very rare and interesting case.
P- Reviewer: Cho YS, Misra SP, Souza JLS, Thomopoulos KC S- Editor: Gong ZM L- Editor: A E- Editor: Ma S
| 1. | Ko GY, Byun JY, Choi BG, Cho SH. The vascular manifestations of Behçet’s disease: angiographic and CT findings. Br J Radiol. 2000;73:1270-1274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 71] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Park JH, Chung JW, Joh JH, Song SY, Shin SJ, Chung KS, Lee DY, Won JY, Kim SJ. Aortic and arterial aneurysms in behçet disease: management with stent-grafts--initial experience. Radiology. 2001;220:745-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 98] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 3. | Ugurlucan M, Sayin OA, Surmen B, Kafali E, Basaran M, Alpagut U, Dayioglu E, Onursal E. Complication of Behcet’s disease: spontaneous aortic pseudoaneurysm. J Card Surg. 2006;21:589-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Marzban M, Mandegar MH, Karimi A, Abbasi K, Movahedi N, Navabi MA, Abbasi SH, Moshtaghi N. Cardiac and great vessel involvement in “Behcet’s disease”. J Card Surg. 2008;23:765-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 5. | Chae EJ, Do KH, Seo JB, Park SH, Kang JW, Jang YM, Lee JS, Song JW, Song KS, Lee JH. Radiologic and clinical findings of Behçet disease: comprehensive review of multisystemic involvement. Radiographics. 2008;28:e31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 87] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 6. | Oliphant M, Berne AS. The subperitoneal space. Dynamic radiology of the abdomen: normal and pathologic anatomy. 5th ed. New York: Springer 2000; 607-634. |
| 7. | Aksoy M, Yanar H, Taviloglu K, Ertekin C, Ayalp K, Yanar F, Guloglu R, Kurtoglu M. Rupture of abdominal aortic aneurysm into sigmoid colon: a case report. World J Gastroenterol. 2006;12:7549-7550. [PubMed] |
| 8. | Banerjee A. Atypical manifestations of ruptured abdominal aortic aneurysms. Postgrad Med J. 1993;69:6-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Saers SJ, Scheltinga MR. Primary aortoenteric fistula. Br J Surg. 2005;92:143-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 187] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 10. | Okada K, Eishi K, Takamoto S, Ando M, Kosakai Y, Nakano K, Sasako Y, Kobayashi J. Surgical management of Behçet’s aortitis: a report of eight patients. Ann Thorac Surg. 1997;64:116-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 1.7] [Reference Citation Analysis (0)] |