Copyright
©The Author(s) 2015.
World J Gastroenterol. Nov 14, 2015; 21(42): 11904-11913
Published online Nov 14, 2015. doi: 10.3748/wjg.v21.i42.11904
Published online Nov 14, 2015. doi: 10.3748/wjg.v21.i42.11904
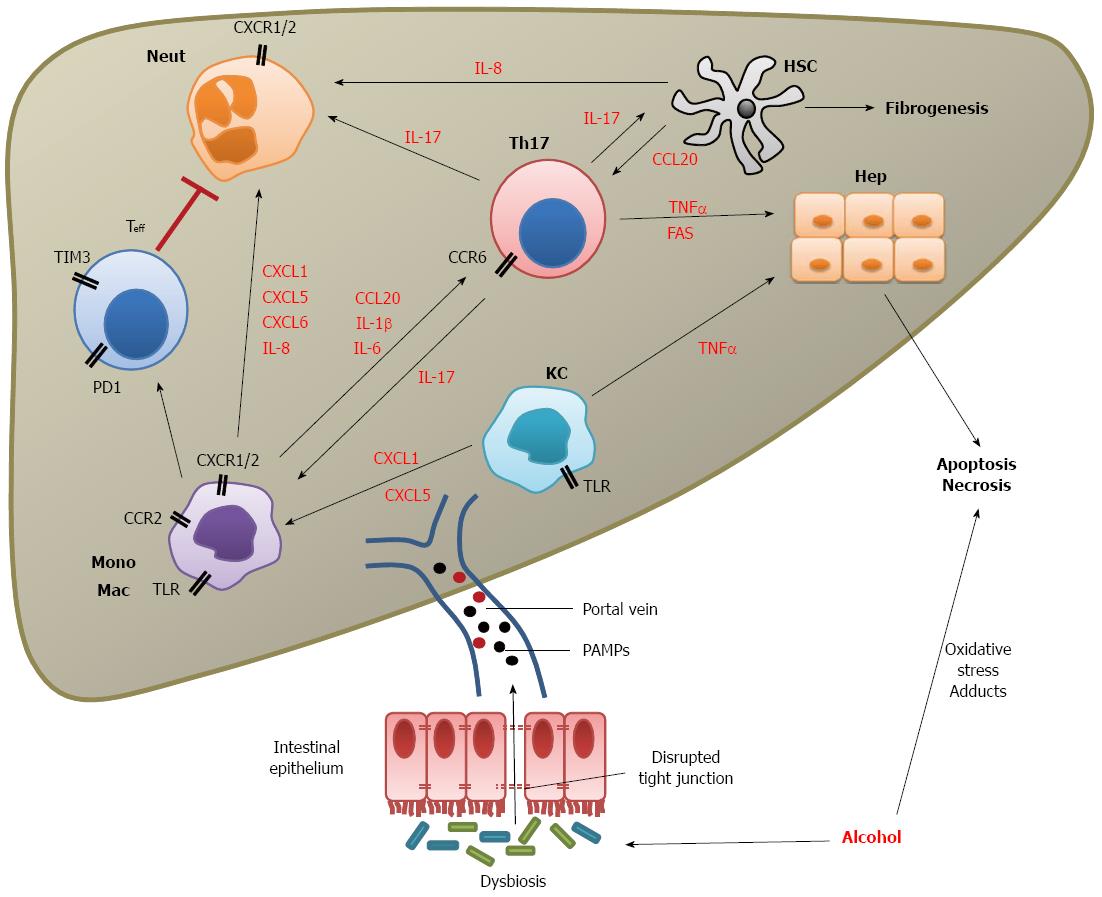
Figure 1 Immune dysfunction in acute alcoholic hepatitis.
Alcohol has a direct effect on hepatocytes by production of reactive oxygen species causing oxidative stress. It also results in the production of acetaldehyde adducts which can cause DNA damage, mutagenesis and direct cell death. Alcohol consumption also leads to intestinal bacterial overgrowth and gut dysbiosis with a loss of lactobacillus and increase in proteobacteria species. Dysbiosis together with the direct effect of acetaldehyde (a metabolite of alcohol) and pro-inflammatory cytokines disrupts epithelial tight junctions and allows the escape of pathogen-associated molecular patterns (PAMPs) into the portal circulation. Within the liver PAMPs are presented to Toll-like receptors (TLRs) on myeloid cells including monocytes (Mono), macrophages (Mac) and Kupffer cells (KC) stimulating release of cytokines and chemokines. In addition, TLR4 activation on monocytes leads to upregulation of negative inhibitory molecules programmed death 1 (PD-1) and T-cell immunoglobulin and mucin domain 3 (TIM-3) on effector T cells (Teff), which in turn inhibit neutrophil (Neut) anti-microbial functions. Chemokines and cytokines coordinate the infiltration and stimulation of other immune cells in particular neutrophils, monocytes (both by CXCL1, 5, 6 and IL-8) and Th17 cells (by CCL20). Th17 cells further increase neutrophil infiltration and also stimulate hepatic stellate cells (HSCs) to produce fibrogenic mediators. TNFα and Fas produced by T cells also leads to hepatocyte cell death by apoptosis through the Fas and TNF receptor pathways.
- Citation: Dhanda AD, Collins PL. Immune dysfunction in acute alcoholic hepatitis. World J Gastroenterol 2015; 21(42): 11904-11913
- URL: https://www.wjgnet.com/1007-9327/full/v21/i42/11904.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i42.11904