Published online Jul 14, 2009. doi: 10.3748/wjg.15.3312
Revised: June 3, 2009
Accepted: June 10, 2009
Published online: July 14, 2009
Proteus syndrome is an extremely rare congenital disorder that produces multifocal overgrowth of tissue. This report presents a surgical case of a large lipoma in the abdominal wall of a patient with Proteus syndrome. She was diagnosed with Proteus syndrome based on certain diagnostic criteria. The neoplasm increased in size gradually, producing hemihypertrophy of her left lower extremity and trunk, and spread to her retroperitoneum and her left abdominal wall. She experienced gradually progressive constipation, nausea, vomiting, and abdominal pain. Computed tomography (CT) of the abdomen demonstrated a large mass in the subcutaneous adipose tissue of the left lower abdominal wall which measured 12 cm × 8 cm x 6 cm in diameter and encased the left colon. This mass in the abdominal wall was excised. The weight of the excised mass was 1550 g. The histopathological diagnosis of this mass was lipoma. After surgery, the encasement of the left colon was improved, and the patient was able to move her bowels twice per day. The excision of the large lipoma in the abdominal wall contributed to the improved bowel passage in this patient with Proteus syndrome.
- Citation: Nakayama Y, Kusuda S, Nagata N, Yamaguchi K. Excision of a large abdominal wall lipoma improved bowel passage in a Proteus syndrome patient. World J Gastroenterol 2009; 15(26): 3312-3314
- URL: https://www.wjgnet.com/1007-9327/full/v15/i26/3312.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.3312
Proteus syndrome is an extremely rare disorder characterized by postnatal overgrowth of multiple tissues derived from different cell lineage[1–3]. The patient with Proteus syndrome described in this paper experienced constipation, nausea, vomiting, and abdominal pain due to the encasement and pressure of the intestinal tract by a large fatty mass which had developed in the left abdominal wall. The excision of this mass improved the symptoms.
A 4-year-old female underwent a resection of a soft mass in her left inguinal area. This mass was pathologically diagnosed to be a lipoma. She was sent to the Department of Orthopedic Surgery because the lesion recurred and spread to the surrounding area. The recurrent tumors in her left inguinal area, left thigh and knee increased in size, and additional excisions were performed when the patient was 8- and 11-years-old. The pathological diagnosis was an infiltrating lipoma. She was diagnosed to have Proteus syndrome based on the diagnostic criteria reported[2–4]. The neoplasm increased in size gradually, and produced hemihypertrophy of the left lower extremity and trunk, and spread to the left abdominal wall and the retroperitoneum. Since the increasing abdominal mass encased and pressed the digestive organs, she gradually developed constipation. Bowel movements occurred about once a week at the time of presentation. A bowel obstruction caused symptoms including constipation, nausea, vomiting and abdominal pain. She had two healthy sisters and the rest of her family were also healthy. She had iron-deficient anemia with hypermenorrhea and she had a transfusion history. On physical examination, she had a temperature of 36.4°C, and blood pressure of 120/70 mmHg. A large mass with unclear margins was found in the left lower quadrant of her abdominal wall (Figure 1). She showed hemihypertrophy and deformity of her left lower extremity. There were large and bizarre skin tumors on her left lower extremity.
Laboratory data showed a white blood cell count of 4800 cells/mm3, hemoglobin 7.7 g/dL, hematocrit 25%, platelets 321 000 cells/mm3, normal electrolytes and blood urea nitrogen, and the liver function was normal.
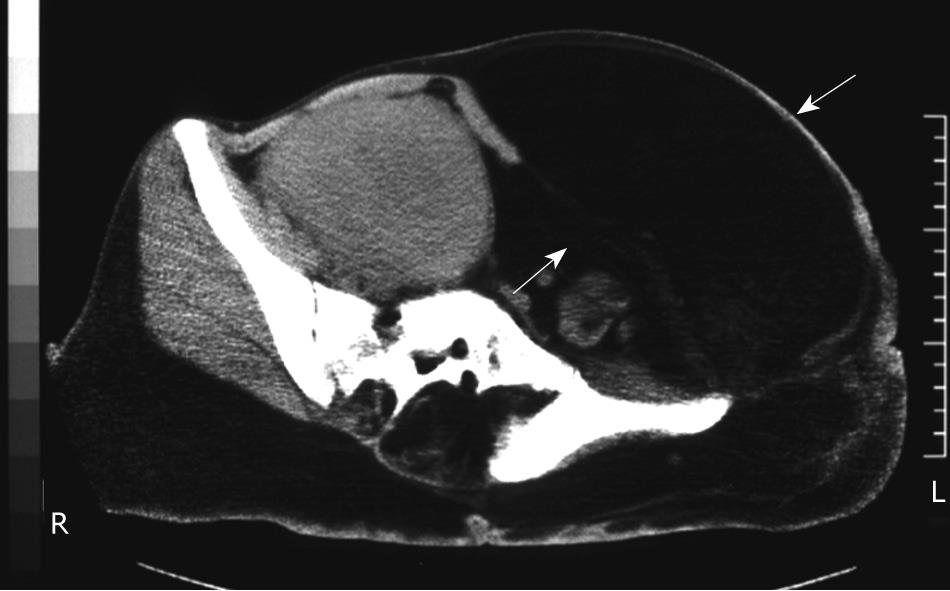
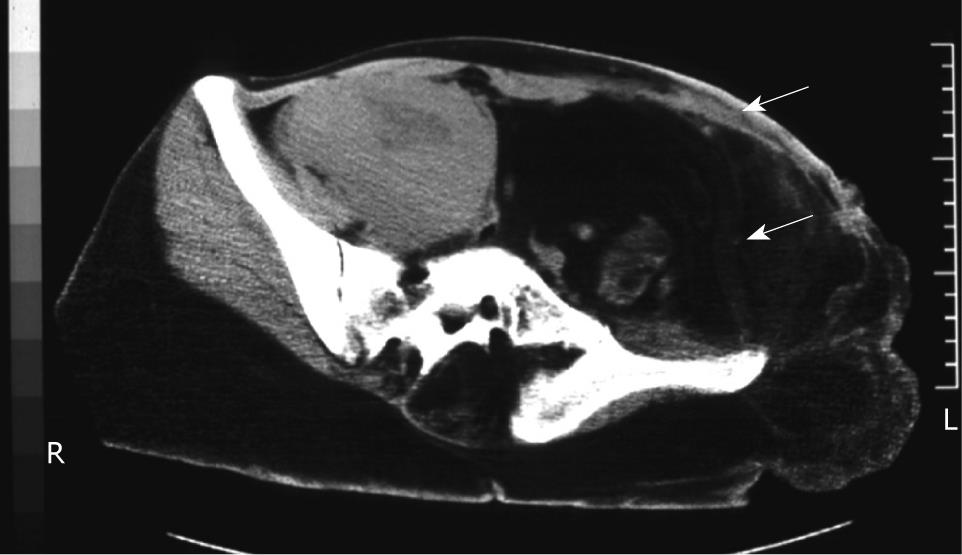
A plain abdominal X-ray examination indicated scoliosis and deformity of the pelvic bone. Colon gas in the left colon shifted to the right upper side (Figure 2). Computed tomography (CT) of the abdomen demonstrated a large mass in the subcutaneous adipose tissue at the left lower abdominal wall which was 12 cm x 8 cm x 6 cm in diameter and encased the peritoneal organs to the right side (Figure 3). An upper gastrointestinal series revealed a mass encasing the stomach toward the upper side and the small intestine toward the right upper side (data not shown).
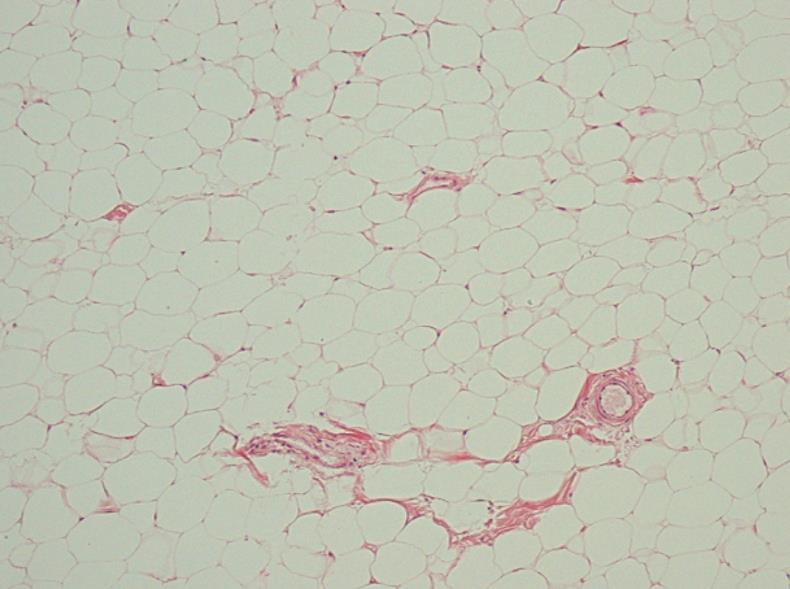
The mass in the abdominal wall was excised in 1997. The weight of the excised mass was 1550 g. A histopathological examination revealed a lobular arrangement of mature adipocytes (Figure 4), and these cells diffusely invaded into the skeletal muscle.
These findings indicated the diagnosis of a non-malignant lipoma.
The postoperative course was uneventful, the encasement of the left colon was improved, and she left the hospital on the 15th postoperative day. At present, she continues to receive medical treatment on an outpatient basis. Postoperatively, bowel movement occurred twice a day. A postoperative plain X-ray examination indicated that the shift of the left colon gas was improved (Figure 5). Postoperative CT also revealed reduced encasement of the peritoneal organs (Figure 6).
Wiedermann et al[2] proposed diagnostic criteria for Proteus syndrome: (1) gigantism of the hands and/or feet, (2) pigmented nevus, (3) hemihypertrophy, (4) subcutaneous tumors, (5) skull anomalies, (6) accelerated growth and (7) visceral abnormalities. Recently, the main diagnostic criteria for Proteus syndrome are that it is sporadic, mosaic and has a progressive course[3]. The current case presented with lipomatosis, severe hemihypertrophy of the left trunk and left lower extremity, scoliosis, endometriosis and huge bizarre-shaped body tumors. Consequently, this patient was diagnosed to have Proteus syndrome based on the above-mentioned diagnostic criteria[5] and was the 6th Japanese case described in the English literature[5–9].
This syndrome is caused by the germline loss of functional mutations in PTEN[10] and is an overgrowth syndrome[11]. PTEN acts as a negative regulator of PI3-kinase signaling by catalyzing the dephosphorylation of PIP3[1213]. This case was diagnosed based on the previous criteria for Proteus syndrome[2–4], and the germline mutation in PTEN was not examined.
Lipomatosis of the colon complicating Proteus syndrome was reported previously[14]. A 12 year-old boy with Proteus syndrome presented with gross abdominal distension and severe intractable constipation. Magnetic resonance imaging showed adipose tissue widely spread throughout the abdomen and pelvis. A laparotomy revealed a huge infiltrating lipomatosis encasing the left colon, including the rectum. On the other hand, the symptoms of bowel obstruction in the current case may have been caused by the encasement and pressure of the intestinal tract by a child-head sized lipoma that developed in the left abdominal wall. This lipoma was excised from the abdominal wall and removal of this huge lipoma produced the improvement in the patient’s symptoms.
Proteus syndrome is a complex disorder associated with varied, disproportionate, asymmetric overgrowth of many body parts and unregulated adipose tissue. The overgrowth seen in Proteus syndrome is progressive and difficult to manage. Patients with Proteus syndrome require repeated treatment for the progressive overgrowth of tissue over a long period. Aggressive treatment may cause severe functional and cosmetic consequences, so surgical intervention is often delayed until it is absolutely necessary[15]. In the current case, other sites of the lipomatosis, such as the left extremity and back, were excised when it affected the patient’s quality of life. This report presented an extremely rare case of bowel obstruction due to a large lipoma in the abdominal wall. The excision of this large mass improved the bowel passage in a patient with Proteus syndrome.
| 1. | Cohen MM Jr, Hayden PW. A newly recognized hamartomatous syndrome. Birth Defects Orig Artic Ser. 1979;15:291-296. |
| 2. | Wiedemann HR, Burgio GR, Aldenhoff P, Kunze J, Kaufmann HJ, Schirg E. The proteus syndrome. Partial gigantism of the hands and/or feet, nevi, hemihypertrophy, subcutaneous tumors, macrocephaly or other skull anomalies and possible accelerated growth and visceral affections. Eur J Pediatr. 1983;140:5-12. |
| 3. | Biesecker LG, Happle R, Mulliken JB, Weksberg R, Graham JM Jr, Viljoen DL, Cohen MM Jr. Proteus syndrome: diagnostic criteria, differential diagnosis, and patient evaluation. Am J Med Genet. 1999;84:389-395. |
| 4. | Hotamisligil GS. Proteus syndrome and hamartoses with overgrowth. Dysmorphol Clin Genet. 1990;4:87. |
| 5. | Yasuda H, Yamamoto O, Hirokawa H, Asahi M, Kashimura M, Sakai A. Proteus syndrome. Dermatology. 2001;203:180-184. |
| 6. | Hagari Y, Aso M, Shimao S, Okano T, Kurimasa A, Takeshita K. Proteus syndrome: report of the first Japanese case with special reference to differentiation from Klippel-Trenaunay-Weber syndrome. J Dermatol. 1992;19:477-480. |
| 7. | Katayama M, Imafuku S, Imayama S, Nakayama J, Hori Y. Two cases of Proteus syndrome characterized by verrucous skin lesions on the soles (abstract in English). Nishinihon J Dermatol. 1992;54:1067. |
| 8. | Miura H, Uchida Y, Ihara K, Sugioka Y. Macrodactyly in Proteus syndrome. J Hand Surg Br. 1993;18:308-309. |
| 9. | Sayama K, Hato N, Matsuda O, Shiraishi S, Miki Y. Proteus syndrome. Dermatology. 1994;189:392-395. |
| 10. | Zhou X, Hampel H, Thiele H, Gorlin RJ, Hennekam RC, Parisi M, Winter RM, Eng C. Association of germline mutation in the PTEN tumour suppressor gene and Proteus and Proteus-like syndromes. Lancet. 2001;358:210-211. |
| 11. | Barker KT, Houlston RS. Overgrowth syndromes: is dysfunctional PI3-kinase signalling a unifying mechanism? Eur J Hum Genet. 2003;11:665-670. |
| 12. | Maehama T, Dixon JE. The tumor suppressor, PTEN/MMAC1, dephosphorylates the lipid second messenger, phosphatidylinositol 3,4,5-trisphosphate. J Biol Chem. 1998;273:13375-13378. |
| 13. | Wu X, Senechal K, Neshat MS, Whang YE, Sawyers CL. The PTEN/MMAC1 tumor suppressor phosphatase functions as a negative regulator of the phosphoinositide 3-kinase/Akt pathway. Proc Natl Acad Sci USA. 1998;95:15587-15591. |
| 14. | Mackay G, Spitz L, McHugh K. Lipomatosis of the colon complicating Proteus syndrome. Arch Dis Child. 2002;86:265. |
| 15. | Biesecker L. The challenges of Proteus syndrome: diagnosis and management. Eur J Hum Genet. 2006;14:1151-1157. |