Copyright
©The Author(s) 2017.
World J Gastroenterol. Nov 21, 2017; 23(43): 7678-7692
Published online Nov 21, 2017. doi: 10.3748/wjg.v23.i43.7678
Published online Nov 21, 2017. doi: 10.3748/wjg.v23.i43.7678
Figure 1 Plasma liver biochemical tests, hepatic histological examination, Col1a1 mRNA expression, and PCNA and ZO-1 protein expression in sham-operated and bile duct-obstructed rats.
Rats were administered either saline or resveratrol (R, 10 mg/kg) daily by oral gavage for 28 d after surgery. Liver sections were stained with Masson's blue trichrome stain for collagen visualization. Sham-operated animals were physiologically normal for the measured parameters; resveratrol administration to Sham animals had no effect. The results of mRNA and protein expression are presented as a percentage of the saline-administered sham group (control). Data are presented as the mean ± SE (n = 6); bP < 0.01, eP < 0.001 vs saline-treated sham group; dP < 0.01, fP < 0.001 vs saline-treated BDO group).
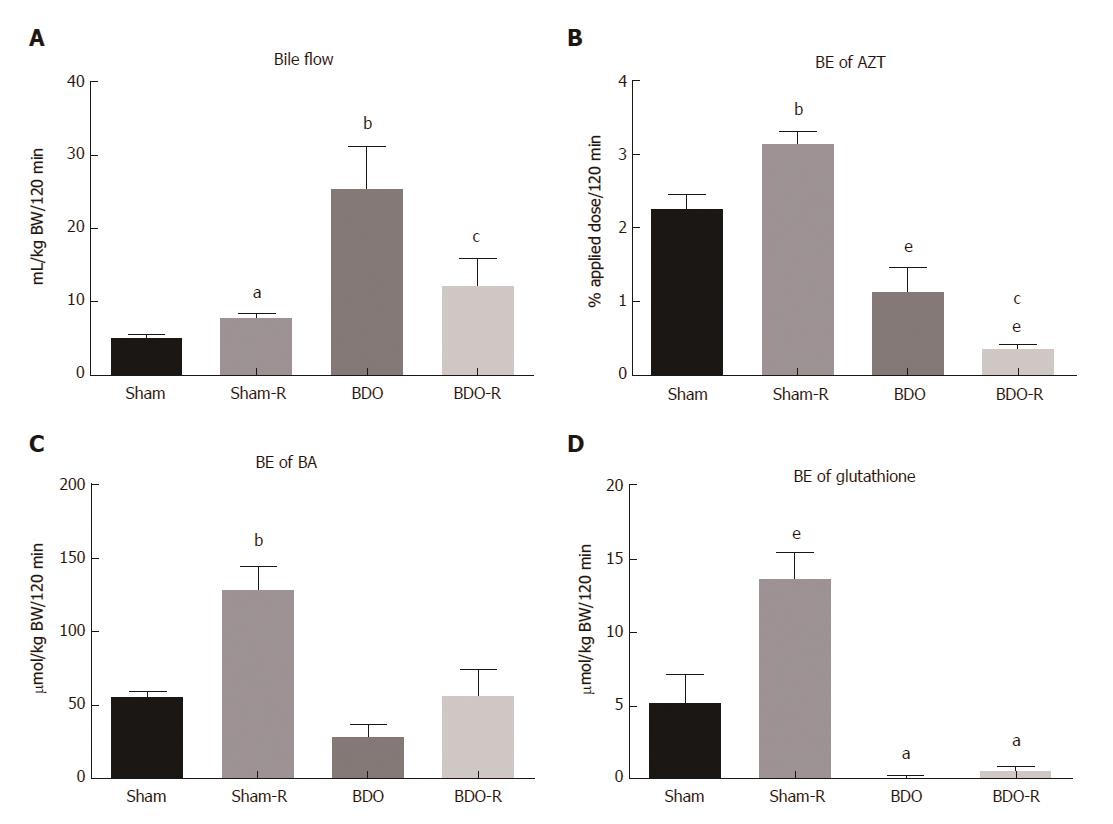
Figure 2 Influence of resveratrol administration and bile duct obstruction on the bile flow rate (A), biliary excretion of azithromycin (B), biliary excretion of bile acids (C), and biliary excretion of glutathione (D).
Rats received either saline or resveratrol (R, 10 mg/kg) daily by oral gavage for 28 d after surgical procedure. Data are presented as the mean ± SE (n = 6). aP < 0.05, bP < 0.01, eP < 0.001 vs saline-treated sham group; cP < 0.05 vs saline-treated BDO group. BE: Biliary excretion; BDO: Bile duct obstruction.
Figure 3 Reduced (GSH) (A) and oxidized (GSSG) (B) glutathione, GSH/GSSG ratio (C), and Nqo1 mRNA (D) expression in the liver of sham and bile duct-obstructed rats.
Rats were administered either saline or resveratrol (R, 10 mg/kg) daily by oral gavage for 28 d after surgery. Data are presented as the mean ± SE (n = 6, in each group). No statistically significant difference was noted between the groups. BDO: Bile duct obstruction.
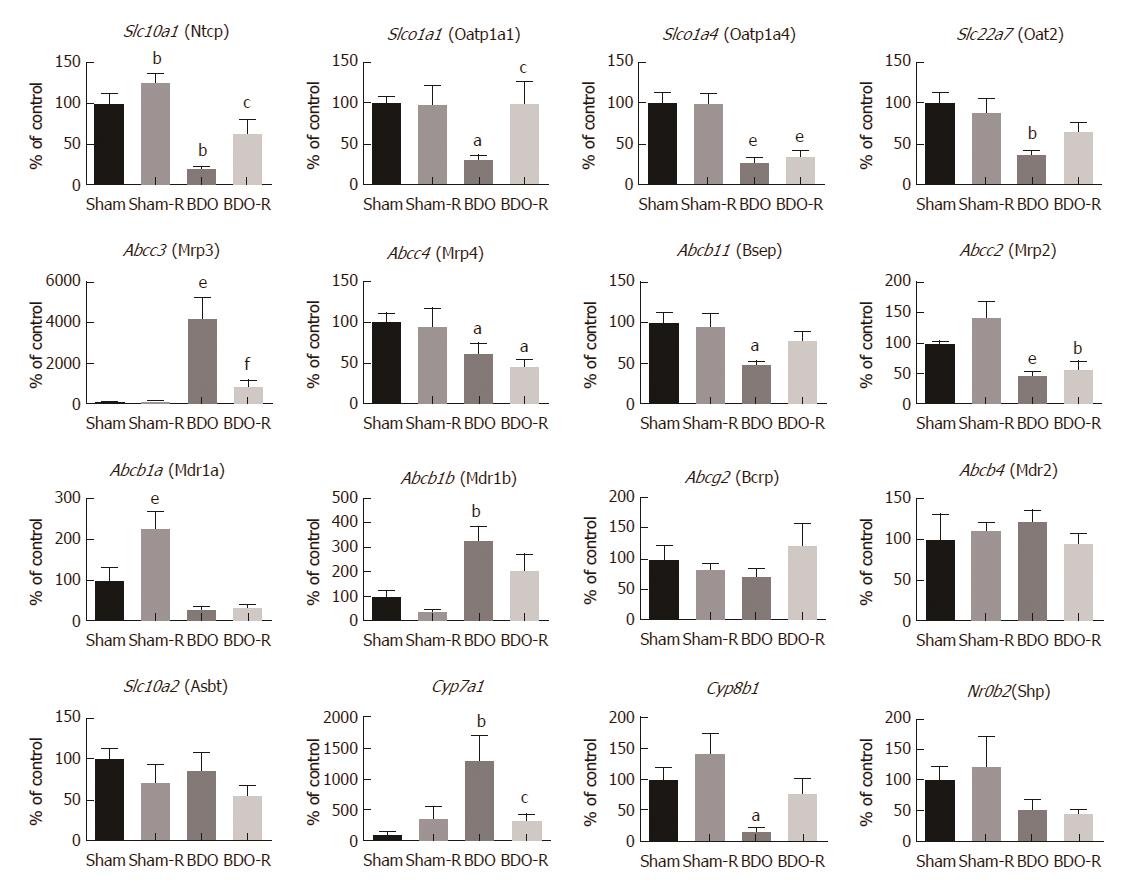
Figure 4 Gene expression of the liver transporters and enzymes involved in bile production and secretion in sham-operated and bile duct-obstructed rats.
Rats received saline or resveratrol (R, 10 mg/kg) once daily by oral gavage for 28 d after surgery. The results are presented as a percentage of the saline-administered sham group (control). Data are presented as the mean ± SE (n = 6); aP < 0.05, bP < 0.01, eP < 0.001 vs saline-treated sham group; cP < 0.05, fP < 0.001 vs saline-treated BDO group. BDO: Bile duct obstruction.
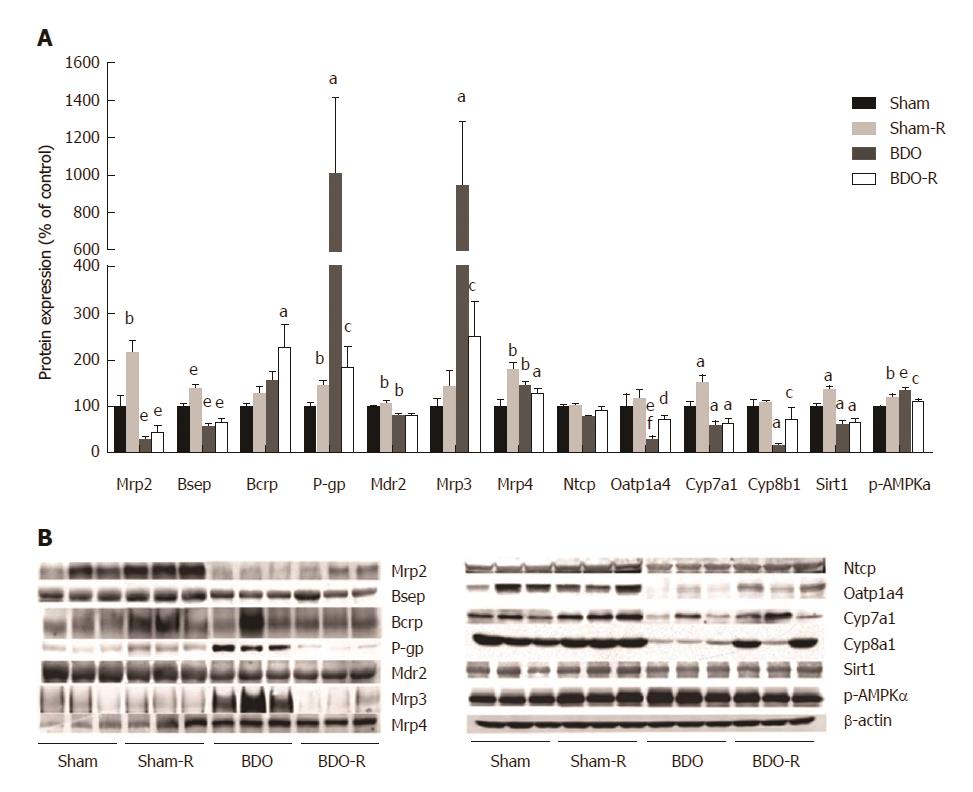
Figure 5 Protein expression of transporters, Cyp7a1, Cyp8b1, Sirt1, and p-AMPKα enzymes in the liver of sham-operated and bile duct-obstructed rats.
Rats were administered either saline or resveratrol (R, 10 mg/kg) daily by oral gavage for 28 d after surgery. The results are presented as a percentage of the saline-administered sham (control) group (A). Representative immunoblots (B). Data are presented as the mean ± SE (n = 6); aP < 0.05, bP < 0.01, eP < 0.001 vs saline-treated sham group; cP < 0.05, dP < 0.01, fP < 0.001 vs saline-treated BDO group. BDO: Bile duct obstruction.
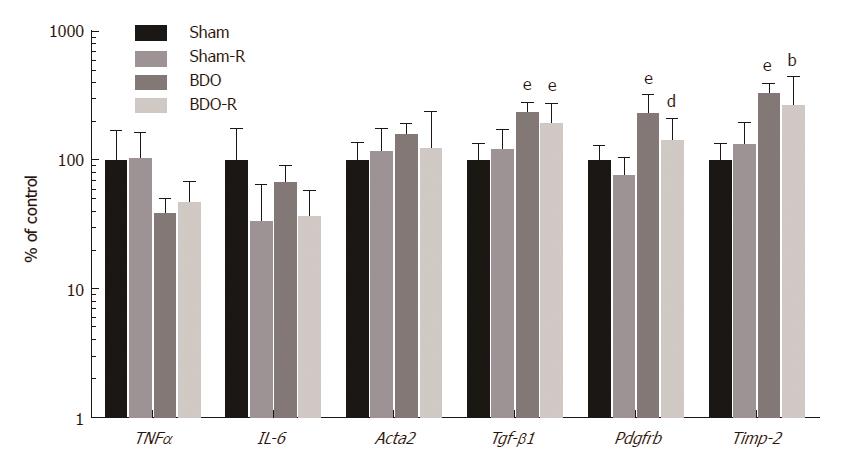
Figure 6 Gene expression of inflammatory and fibrogenic markers in the liver of sham-operated and bile duct-obstructed rats.
Rats were administered either saline or resveratrol (R, 10 mg/kg) daily by oral gavage for 28 d after surgery. The results are presented as a percentage of the saline-administered sham group (control). Data are mean ± SE (n = 6); bP < 0.01, eP < 0.001 vs saline-treated sham group; dP < 0.01, fP < 0.001 vs saline-treated BDO group. BDO: Bile duct obstruction.
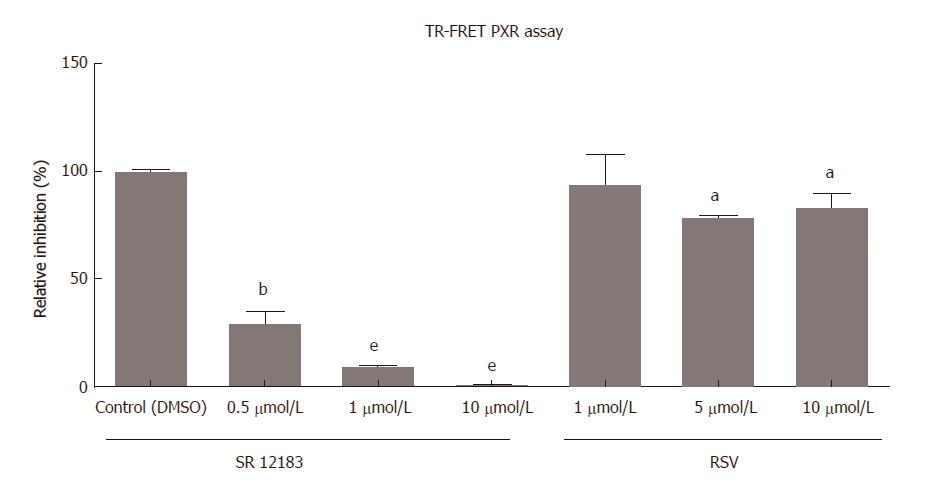
Figure 7 LanthaScreen® TR-FRET PXR competitive binding assay was performed to determine the ability of PXR to bind to the PXR ligand binding domain and replace a fluorescent PXR ligand.
SR12813, a model PXR agonist, was used as a high-affinity ligand in the PXR ligand binding domain to validate the method. The data are presented as the mean ± SD from three independent experiments (n = 3) performed in triplicate measurements. Significantly different compared to the control treatment. aP < 0.05, bP < 0.01, eP < 0.001.
- Citation: Dolezelova E, Prasnicka A, Cermanova J, Carazo A, Hyrsova L, Hroch M, Mokry J, Adamcova M, Mrkvicova A, Pavek P, Micuda S. Resveratrol modifies biliary secretion of cholephilic compounds in sham-operated and cholestatic rats. World J Gastroenterol 2017; 23(43): 7678-7692
- URL: https://www.wjgnet.com/1007-9327/full/v23/i43/7678.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i43.7678