Copyright
©The Author(s) 2017.
World J Gastroenterol. Mar 14, 2017; 23(10): 1735-1746
Published online Mar 14, 2017. doi: 10.3748/wjg.v23.i10.1735
Published online Mar 14, 2017. doi: 10.3748/wjg.v23.i10.1735
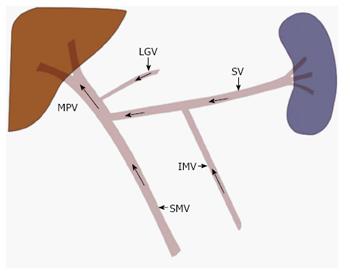
Figure 1 Normal portal venous anatomy and direction of blood flow.
The main portal vein (MPV) is most commonly formed when the splenic vein (SV) and the superior mesenteric vein (SMV) join. While variable, the inferior mesenteric vein (IMV) most commonly drains in to the splenic vein, at the level of the pancreatic body. Other tributaries may also join the MPV, such as the left gastric vein (LGV) as depicted here.
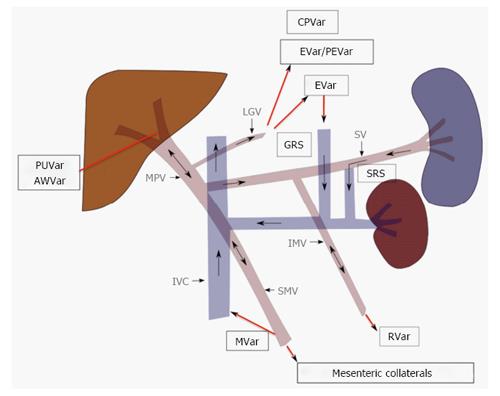
Figure 2 Portosystemic collateral pathways and direction of blood flow in portal hypertension.
Progressive resistance to hepatopetal flow results in slowed and eventually reversed flow in the main portal vein (MPV). Portal venous system decompresses by recruiting several pre-exiting collateral pathways, the selection of which is partly dictated by the location of the portal venous resistance. Paraumbilical (PUVar), abdominal wall varices (AWVar), esophageal (EVar), paraesophageal (PEVar), gastric (GVar), cardiophrenic (CPVar), mesenteric (MVar) and rectal (RVar) varices may be created in order to allow the passage the portal venous blood into systemic circulation. LGV: Left gastric vein; SV: Splenic vein; IMV: Inferior mesenteric vein; IVC: Inferior vena cava; SRS: Splenorenal shunt; GRS: Gastrorenal shunt.
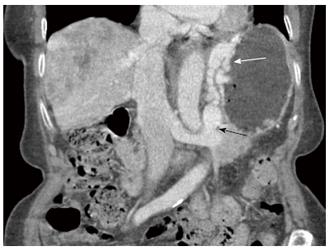
Figure 3 Axial enhanced computed tomography of the upper abdomen in portal venous phase demonstrates multiple large tubular and serpiginous esophageal (white arrow) and paraesophageal (black arrow) varices at the level of the esophageal hiatus of the diaphragm.
Figure 4 Endoscopic image of large tortuous submucosal esophageal varices protruding into the esophageal lumen.
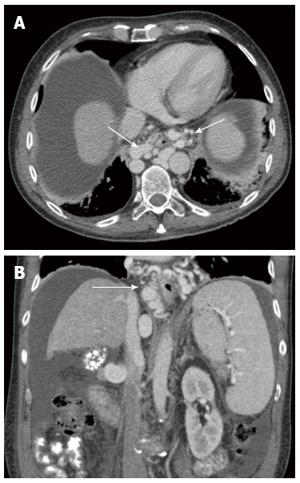
Figure 5 Axial (A) and coronal (B) cross-sectional enhanced computed tomography images show large paraesophageal varices (white arrow) surrounding the esophagus circumferentially in a patient with liver cirrhosis and portal hypertension.
Note the nodular and shrunken liver, low-density abdominal ascites and splenomegaly.
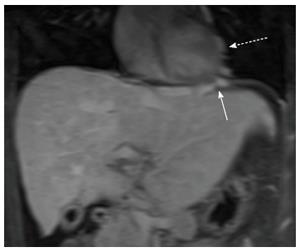
Figure 6 Coronal post-gadolinium T1-weighted fat-suppressed magnetic resonance image shows prominent cardiophrenic (white arrow) and pericardial collateral veins (dashed white arrow) in a patient with Budd-Chiari syndrome.
Figure 7 Enhanced axial computed tomography image acquired in portal venous phase demonstrates large upper abdominal omental varices (white arrow).
Additionally, several enlarged submucosal gastric (black arrow) and short gastric varices (dashed black arrow).
Figure 8 Retroflexed endoscopic image of large tortuous submucosal gastric varices (black star).
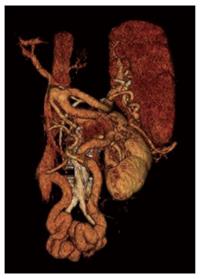
Figure 9 Coronal enhanced computed tomography image demonstrates a large gastrorenal shunt (black arrow) and perigastric, as well as, gastric submucosal varices (white arrow) in a patient with liver cirrhosis and portal hypertension.
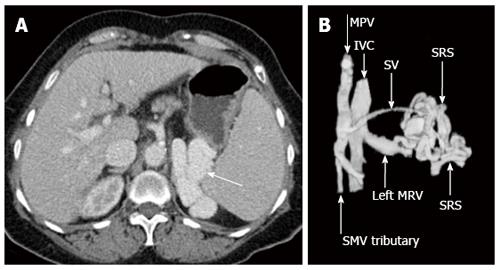
Figure 10 Axial enhanced computed tomography acquired in portal venous phase demonstrates a prominent splenorenal shunt (A, white arrow), left anterior oblique three dimensional computed tomography reconstruction re-demonstrates spontaneous splenorenal shunt draining portal venous blood into the left extra-hilar main renal vein (B).
MPV: Main portal vein; SMV: Superior mesenteric vein; IVC: Inferior vena cava; SV: Splenic vein; SRS: Spontaneous splenorenal shunt; MRV: Main renal vein.
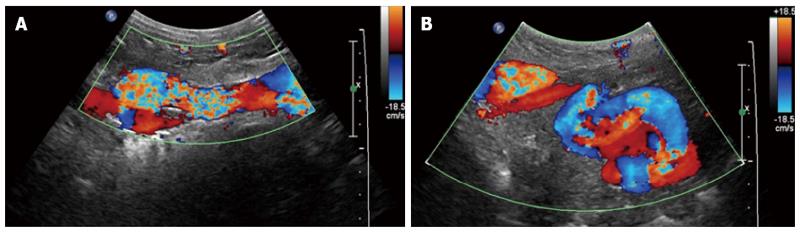
Figure 11 Sagittal (A) and transverse midline (B) Doppler sonographic images demonstrate turbulent flow within a recanalized paraumbilical vein.
Figure 12 Axial enhanced computed tomography image acquired in portal venous phase (A) and coronal-oblique three-dimensional computed tomography reconstruction (B) demonstrating large paraumbilical varices with large associated caput medusa.
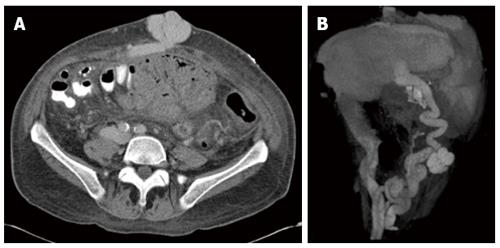
Figure 13 Right anterior oblique three-dimensional computed tomography reconstruction shows mesocaval collateral veins shunting blood from the inferior mesenteric vein to the inferior vena cava via the right ovarian vein.
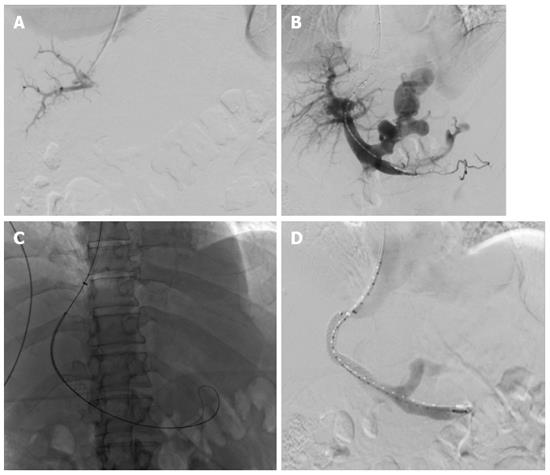
Figure 14 Transjugular intrahepatic portosystemic shunt procedure performed on a 54-year-old male with alcohol-induced cirrhosis and portal hypertension who presents with intractable ascites.
A: Rosch-Uchida transjugular intrahepatic portosystemic shunt (TIPS) trochar-needle set (Cook Medical, Bloomington, United States) was advanced into an anterior branch of the right portal vein successfully after four attempts; B: Subsequently a wire and pigtail catheter were advanced into the main portal vein and subtraction angiography was performed demonstrating large dilated left gastric varices; C: Viatorr polytetrafluoroethylene (PTFE)-covered self-expanding stent (Gore Medical, Flagstaff, United States) was deployed over the tract; D: Completion portography demonstrates patency of the TIPS with decreased overall flow into the gastric varices.
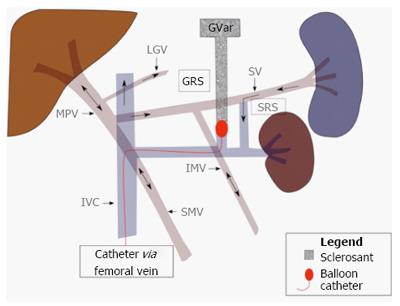
Figure 15 Retrograde balloon occlusion of gastro-renal shunt via femoral venous approach coursing through the inferior vena cava and left renal vein.
After balloon occlusion, a sclerosing agent is injected into the gastric varices (GVar). Black arrows indicate directional blood flow. MPV: Main portal vein; IMV: Inferior mesenteric vein; IVC: Inferior vena cava; GRS: Gastrorenal shunt.
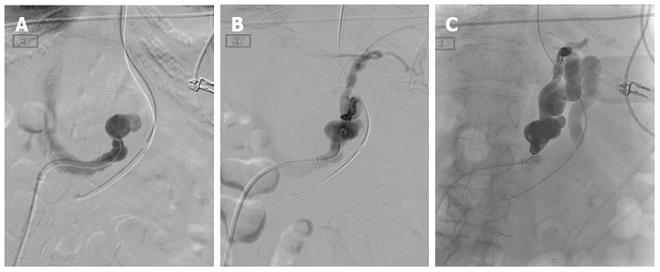
Figure 16 Coil-assisted retrograde transvenous obliteration of gastric varices in a 55-year-old patient who presented with recurrent gastric variceal bleeding refractory to endoscopic therapy.
A: Angled catheter was navigated into the left gastrorenal shunt after obtaining access from the right common femoral vein and advancing 5-french sheath into the inferior vena cava; B: Digital subtraction angiography performed through the gastrorenal shunt demonstrating large dilated shunt vessels, as well as, secondary outflow through pericardiophrenic collaterals; C: Both the proximal and distal shunts were coil-occluded and gelfoam was utilized to embolize and thrombose the gastric varices.
- Citation: Bandali MF, Mirakhur A, Lee EW, Ferris MC, Sadler DJ, Gray RR, Wong JK. Portal hypertension: Imaging of portosystemic collateral pathways and associated image-guided therapy. World J Gastroenterol 2017; 23(10): 1735-1746
- URL: https://www.wjgnet.com/1007-9327/full/v23/i10/1735.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i10.1735