Copyright
©2012 Baishideng Publishing Group Co.
World J Gastroenterol. Sep 14, 2012; 18(34): 4684-4692
Published online Sep 14, 2012. doi: 10.3748/wjg.v18.i34.4684
Published online Sep 14, 2012. doi: 10.3748/wjg.v18.i34.4684
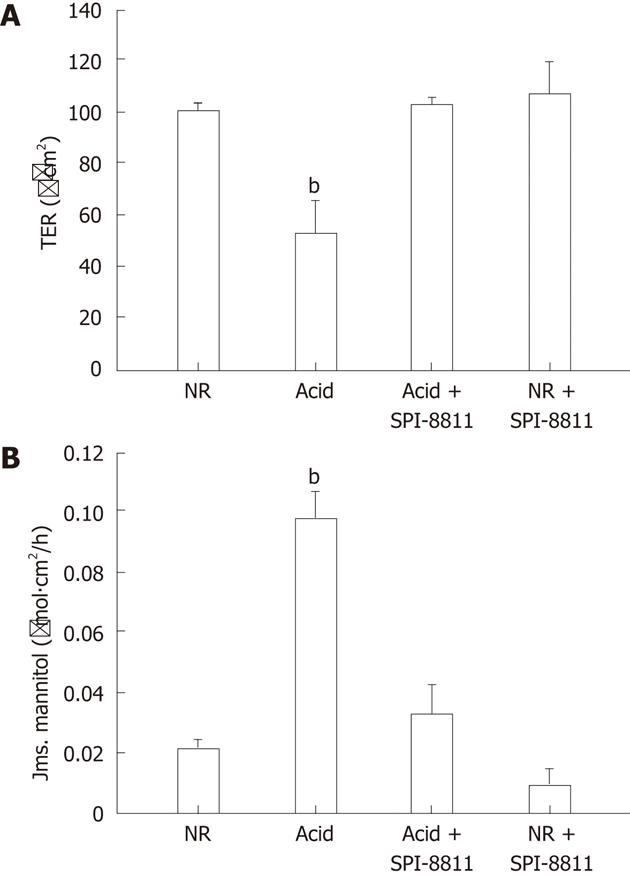
Figure 1 Barrier function of acid injured porcine gastric mucosa to pretreatment of SPI-8811 (1 μmol/L).
A: Porcine gastric mucosa mounted on Ussing chambers challenged with mucosal acid (HCl, pH 1.5) over a 90 min period had significantly lower transepithelial electrical resistance (TER) (100 Ω.cm2vs 50 Ω.cm2) when compared with control tissues bathed in normal Ringer’s (NR). Mucosal application of the ClC-2 agonist SPI-8811 (1 μmol/L) prior to application of acid blocked reductions in TER (TER, 50 Ω.cm2vs 100 Ω.cm2) .Values represent means ± SE, n = 8, bP < 0.01 vs all other treatment groups; B: As an alternative assessment of gastric mucosal barrier function, mucosal-to-serosal fluxes of 3H-mannitol were examined. In agreement with TER responses, 3H-mannitol flux was significantly elevated by treatment with acid (3H-mannitol flux, 0.02 μmol/L.cm2vs 0.10 μmol/L.cm2), and this response was inhibited by SPI-8811. (3H-mannitol flux, 0.10 μmol/L.cm2vs 0.04 μmol/L.cm2). Values represent mean ± SE, n = 6, bP < 0.01 vs all other treatment groups.
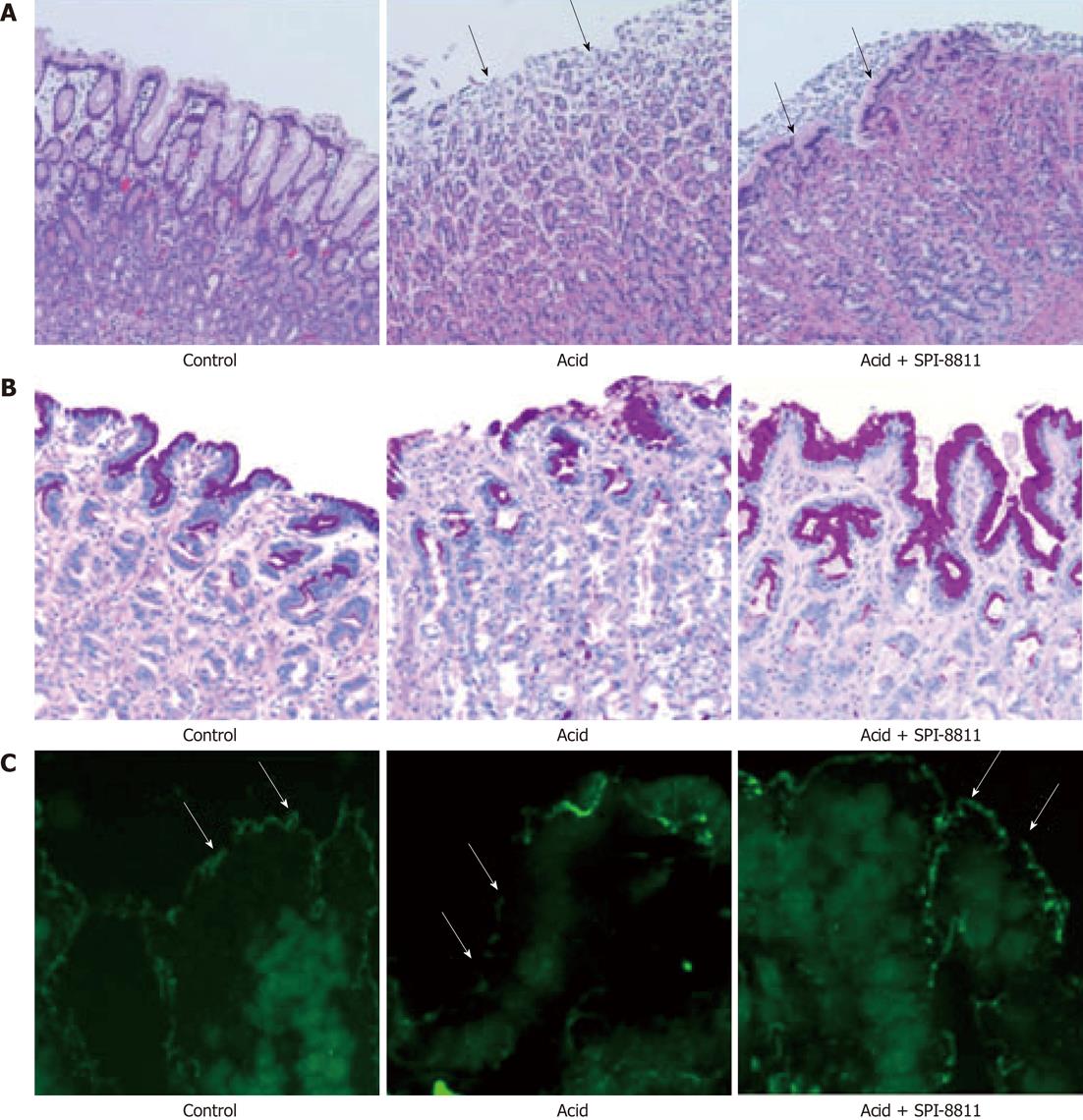
Figure 2 Histological findings in acid-injured gastric mucosal tissues.
A: Tissues bathed in normal Ringer’s appeared uninjured after 90 min in Ussing chambers, whereas those exposed to acid had substantial evidence of epithelial injury (× 100). Pretreatment with SPI-8811 ameliorated injury evident in acid-injured tissues. Each panel is representative of at least 3 separate animals; B: Periodic acid-schiff stain (PAS) staining findings in control tissues bathed in Ringer’s solution for 90 min appeared to have normal expression of surface mucus by PAS-alcian blue staining whereas tissues exposed to acid had distinct loss to surface mucus staining (× 100). However, pretreatment with SPI-8811 prevented the loss of mucus in response to acid and thus preserved the surface mucus; C: Immunofluorescence findings for tight junction protein occludin reveals control tissues bathed in Ringer’s solution for 90 min appeared to have normal immunolocalization of the tight junction protein occluding (green fluorescence) whereas tissues exposed to acid had very little visible apical epithelial occludin (× 200). However, pretreatment with SPI-8811 prevented the disorganized appearance of occludin in response to acid. Note the specific localization of occludin in each panel (arrows).
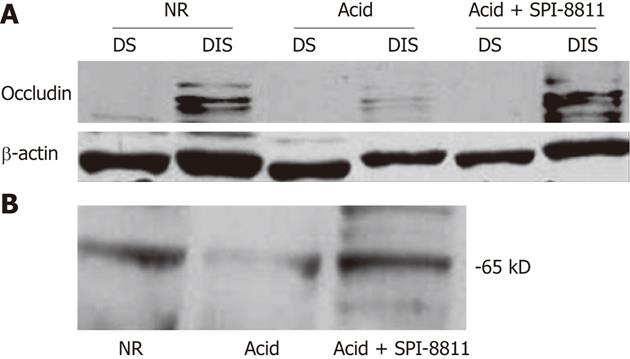
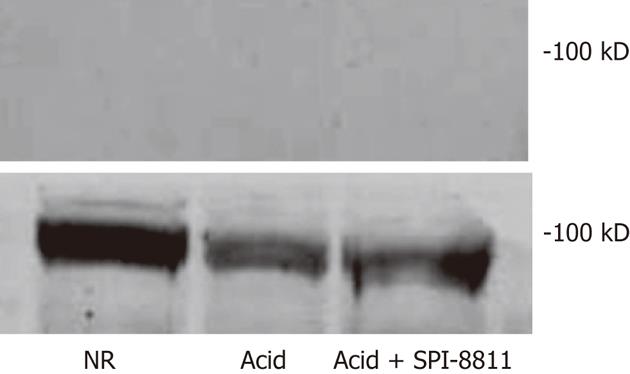
Figure 3 Expression of tight junction proteins in membrane fractions in acid injured porcine gastric mucosa.
A: Western analysis revealed expression of occludin in the detergent insoluble in tissues treated with normal Ringer’s (NR) alone, with very little discernable occludin in the detergent soluble fraction. On the other hand, treatment with acid (pH of 1.5 for 90 min) markedly reduced the expression of occludin in the detergent insoluble fraction, with a similar lack of occludin expression in the detergent soluble fraction. Pretreatment of tissues with mucosal SPI-8811 resulted in expression of occludin in the different fractions to a very similar extent as control tissues; B: Western analysis revealed expression of whole occludin in either control, acid injured and SPI-8811 pretreated and acid injured porcine gastric mucosa from Ussing chambers. Acid injury markedly reduced expression of whole occludin compared to control while pretreatment with SPI-8811 preserved the loss of occludin from acid injury. DS: Detergent soluble; DIS: Detergent insoluble.
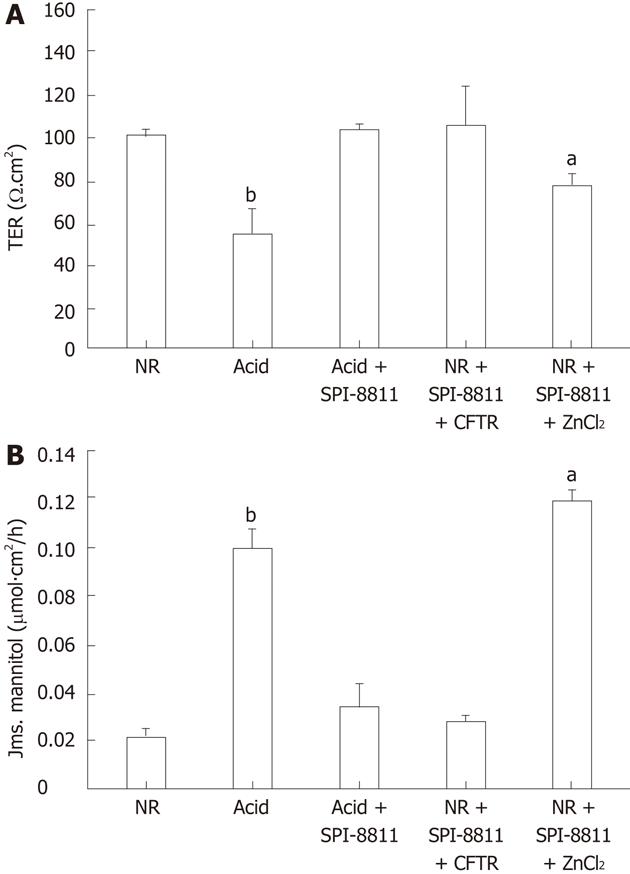
Figure 4 Electrical responses and 3H-mannitol fluxes of acid-injured porcine gastric mucosa.
A: Porcine gastric mucosa exposed to acid (pH 1.5 for 90 min) exhibited a significant drop in transepithelial electrical resistance (TER), which was completely blocked by pretreatment with SPI-8811. In attempt to discern which chloride channel was involved in the gastro protective mechanism of SPI-8811, ClC-2 and cystic fibrosis transmembrane conductance regulator (CFTR) were inhibited. Addition of the ClC-2 inhibitor ZnCl2 ameliorated the protective effect of SPI-8811 (TER, 100 Ω.cm2vs 80 Ω.cm2) whereas the CFTR inhibitor CFTR inhibitor 172 had no effect (TER, 100 Ω.cm2vs 100 Ω.cm2). Values represent mean ± SE, n = 6; aP < 0.05, bP < 0.01 vs all treatment groups; B: As an alternate measure of barrier permeability mucosal-to-serosal of 3H-mannitol flux were performed, and reveled a significant increase in mannitol permeability in acid injured tissues (bP < 0.01). Pretreatment with SPI-8811 blocked the increase in 3H-mannitol flux caused by acid injury, whereas blockade of ClC-2 inhibitor ZnCl2 block the protective effect of SPI-8811 (3H-mannitol flux, 0.04 μmol/L.cm2vs 0.12 μmol/L.cm2, aP < 0.05) on permeability but CFTR inhibitor had no effect on the level of protective properties of SPI-8811 on permeability (3H-mannitol flux, 0.04 μmol/L.cm2vs 0.05 μmol/L.cm2, bP < 0.01). Values represent mean ± SE, n = 6. NR: Normal Ringer’s.
Figure 5 Expression of ClC-2 protein in porcine mucosa.
Mucosal homogenates from porcine stomach were studied for expression of ClC-2 by western blotting. Expression of ClC-2 protein at its expected molecular weight (98 kD) was evident in all lanes. However, there appears to be greater expression of tissues bathed in Ringer’s solution as compared to those subjected to acid or acid and SPI-8811 (n = 3). NR: Normal Ringer’s.
- Citation: Nighot M, Moeser A, Ueno R, Blikslager A. Gastro protective properties of the novel prostone SPI-8811 against acid-injured porcine mucosa. World J Gastroenterol 2012; 18(34): 4684-4692
- URL: https://www.wjgnet.com/1007-9327/full/v18/i34/4684.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i34.4684