Published online Sep 26, 2016. doi: 10.5662/wjm.v6.i3.187
Peer-review started: May 3, 2016
First decision: June 17, 2016
Revised: June 18, 2016
Accepted: July 14, 2016
Article in press: July 16, 2016
Published online: September 26, 2016
Processing time: 142 Days and 20 Hours
Ilio-inguinal lymph node dissection (IILD) is a commonly performed surgical procedure for a number of malignant conditions involving mainly the male and female genitalia, and the skin; however the postoperative morbidity of IILD, due to high frequency of flap necrosis, wound infection and seroma formation, has always been a major concern for the surgeons. The aim of the study is to highlight a modified skin bridge technique of IILD using two parallel curvilinear incisions to minimize postoperative skin flap necrosis. This technique was successfully employed in 38 IILD during May 2012 to November 2013. None of the patient had flap necrosis. Two patients developed seroma while another two patients had superficial surgical site infection; they were managed conservatively. Modified skin bridge technique for IILD is an effective method to minimize flap necrosis without compromising the oncological safety.
Core tip: Ilio-inguinal lymph node dissection (IILD) has classically been associated with high postoperative complications which include flap necrosis, wound infection, seroma formation, and lymphedema. A modified skin bridge technique of performing IILD aims to minimize the postoperative wound complications. It is an effective method to minimize flap necrosis without compromising adequate oncologically safe dissection.
- Citation: Ray MD, Garg PK, Jakhetiya A, Kumar S, Pandey D. Modified skin bridge technique for ilio-inguinal lymph node dissection: A forgotten technique revisited. World J Methodol 2016; 6(3): 187-189
- URL: https://www.wjgnet.com/2222-0682/full/v6/i3/187.htm
- DOI: https://dx.doi.org/10.5662/wjm.v6.i3.187
Ilio-inguinal lymph node dissection (IILD) has classically been associated with high postoperative complications which include flap necrosis, wound infection, seroma formation, and lymphedema. Although a number of modifications of surgical techniques to perform IILD have been reported in the literature, frequency of various complications remains high. In a recent review of IILD, Hegarty et al[1] reported that frequency of skin flap necrosis varies from 7.5% to 61% in radical IILD; other major complications of IILD include infection (7.5% to 14.2%), seroma formation (5% to 13.8%) and lymphedema (2.5% to 5.2%). In 1972, Fraley et al[2] described a new technique “skin bridge technique” for IILD to reduce postoperative wound complications; however, this technique failed to gain popularity among the surgeons. We, herein, present our modified skin bridge technique which aims to lessen the frequency of postoperative skin flap necrosis.
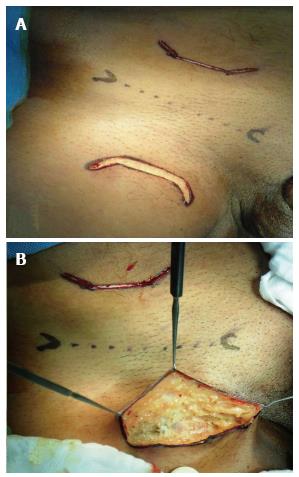
The patient was positioned supine with abduction and external rotation at hip joints (Figure 1). This technique entailed two curvilinear incisions: An inguinal incision, of approximately 7 cm length, 4 cm below and parallel to the inguinal ligament; and an iliac incision, of 5-7 cm length, 4 cm above and parallel to the inguinal ligament (Figure 2A). During the inguinal part of dissection, the skin flap was raised preserving the subcutaneous fat, just superficial to Scarpa’s fascia, with flap (Figure 2B); the lateral limit of dissection was the medial border of Sartorius and the medial limit was the lateral border of adductor longus, the upper limit was 2-3 cm above the inguinal ligament, and the lower limit was the apex of the Scarpa’s triangle. During the iliac part of the dissection - the external oblique muscle was divided along the skin incision, and the internal oblique and transverses abdominis muscles were split along the muscle fibres. The retroperitoneal space was entered thereafter. Inguinal and iliac lymphadenectomy is completed as per the standard technique. The margins of the inguinal incisions were routinely freshened before closure. Sartorius flap was routinely used to cover the femoral vessels in all patients. One closed suction drain was placed in the inguinal region; no drain was used for iliac dissection area (Figure 3). A light pressure dressing was done. All the patients were prescribed elastic stockings within eight hours of the surgery. Antithrombotic prophylaxis was not routinely prescribed. The patients were discharged on 2nd postoperative days after having been explained and taught surgical site care and how to measure daily drain output. The drain was removed in an out-patient clinic after the drain output decreased to less than 40 mL/d. All patients receive perioperative antibiotics for five days or till drainage tube was not removed.
This technique was successfully employed in 38 IILD during May 2012 to November 2013. There was no perioperative mortality. None of the patient had flap necrosis. Six patients developed seroma while another two had superficial surgical site infection; they were managed conservatively. For a unilateral ilio-inguinal lymphadenectomy, the median lymph nodes harvested were 10 (interquartile range 7-15) while the median operative time and blood loss was 50 min (interquartile range 45-60) and 15 mL (interquartile range 10-25) respectively.
IILD has been traditionally an integral part of management of male and female genital cancers, and skin cancers; however, it is associated with considerable post operative morbidity and high frequency of ischemic necrosis of skin flaps. These complications have reduced over a period of time with certain technical modifications as it is evident from two publications from a single institute in south India[3,4]. In a large series of 174 IILDs, performed from 1962 to 1990, Ravi[3] reported that postoperative complications of IILD were partial skin flap necrosis in 64%, wound infection in 14%, seroma formation in 9%, and limb lymphedema in 29% of dissections. Another paper form the same institute[4], published 14 years later highlighted a lower rate of flap necrosis (19.8%) in 202 IILDs performed from 1987 to 1998. Though there was a reduction in the rate of flap necrosis in IILDs, it continued to be considerably high (19.8%). The high postoperative morbidity associated with IILD is at the helm of many controversies: Whether the extent of lymphadenectomy can be curtailed in early cancer? Whether should one go for sentinel node biopsy? Whether there is any role for prophylactic lymphadenectomy at all? And what is the role of whole gamut of new minimally invasive techniques of IILD. We tried to address to problem of skin flap necrosis with our innovative modified skin bridge technique using two parallel curvilinear incisions.
The blood supply of the skin flap is derived from the three superficial branches of the femoral artery namely - superficial external pudendal, superficial epigastric and superficial circumflex iliac. These vessels are usually divided during conventional technique of groin dissection, and so the vascularity of the skin flaps rely solely upon the anastomotic branches of these vessels forming a microvascular arcade which lies in the camper’s fascia and runs parallel to inguinal ligament[5]. This anatomical fact is the basis of our technique as both incisions remain parallel to the inguinal ligament, and thus spare the above mentioned vessels which run superficial to Scarpa’s fascia. The curves at the ends of the curvilinear incisions define the medial and lateral boundary of the dissection; an overzealous dissection beyond the limits has been a crucial factor which can jeopardize the vascularity of skin flaps and result in its necrosis[3].
There are some minor modifications that we made in our technique compared to what was described originally by Fraley and Hutchens[2]: (1) relatively smaller skin incisions; (2) routine transposition of Sartorius muscle to cover the femoral vessels; (3) no routine femoral hernia repair; (4) no en bloc dissection of iliac and inguinal lymph nodes; and (5) routine freshening of both skin edges of inguinal incision.
Modified skin bridge technique for IILD is an effective method to minimize flap necrosis without compromising oncological safety.
Manuscript source: Invited manuscript
Specialty type: Clinical medicine
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Hu SCS, Markopoulos AK S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Hegarty PK, Dinney CP, Pettaway CA. Controversies in ilioinguinal lymphadenectomy. Urol Clin North Am. 2010;37:421-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Fraley EE, Hutchens HC. Radical ilio-inguinal node dissection: the skin bridge technique. A new procedure. J Urol. 1972;108:279-281. [PubMed] |
| 3. | Ravi R. Morbidity following groin dissection for penile carcinoma. Br J Urol. 1993;72:941-945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 93] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Pandey D, Mahajan V, Kannan RR. Prognostic factors in node-positive carcinoma of the penis. J Surg Oncol. 2006;93:133-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 139] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 5. | Spratt J. Groin dissection. J Surg Oncol. 2000;73:243-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |