Published online Mar 20, 2025. doi: 10.5662/wjm.v15.i1.98343
Revised: August 22, 2024
Accepted: August 29, 2024
Published online: March 20, 2025
Processing time: 96 Days and 10.5 Hours
Pulmonary embolism (PE) is a rare but devastating complication of shoulder surgery. Apart from increased morbidity and mortality rates, it may significantly impair postoperative recovery and functional outcome. Its frequency accounts for up to 5.7% of all shoulder surgery procedures with a higher occurrence in women and patients older than 70 years. It is most commonly associated with thrombophilia, diabetes mellitus, obesity, smoking, hypertension, and a history of mali
Core Tip: Pulmonary embolism is a rare and possibly fatal complication of shoulder surgery. While venous thromboembolism, which includes pulmonary embolism and deep vein thrombosis, has been extensively studied, there is a lack of data about pulmonary embolism as a distinct pathology after shoulder surgery. This review summarizes the most important information about this condition and highlights the significance of early diagnosis and treatment.
- Citation: Pitsilos C, Papadopoulos P, Givissis P, Chalidis B. Pulmonary embolism after shoulder surgery: Is it a real threat? World J Methodol 2025; 15(1): 98343
- URL: https://www.wjgnet.com/2222-0682/full/v15/i1/98343.htm
- DOI: https://dx.doi.org/10.5662/wjm.v15.i1.98343
Venous thromboembolism (VTE) is an umbrella term of two pathologies, deep vein thrombosis (DVT) and pulmonary embolism (PE)[1]. PE is the third most common cause of cardiovascular death worldwide after stroke and heart attack[2]. Most PE events originate as DVTs of the lower extremities and approximately 50% of DVTs lead to silent PE[3].
Although PE is a rare cause of perioperative morbidity and mortality following open shoulder surgery (SS), it is one of the most common reasons for readmission during the postoperative period, following surgical-site infection and other wound complications[4,5]. It is also the main cause of readmission after shoulder arthroscopy[6]. PE may occur primarily or secondarily to upper or lower-extremity DVT after SS[7]. The risk factors that increase the potential of PE after upper-extremity trauma or surgical treatment are similar to those for DVT. They include smoking, hypertension, diabetes mellitus, obesity, a history of cancer, and thrombophilia, among others[8-10]. If misdiagnosed or diagnosed late, PE may progress and become subsequently fatal[11]. Intensive care physicians must be aware of this dreadful condition following SS and keep a high index of suspicion to diagnose and manage it promptly and effectively.
The overall incidence of PE after SS is 0.08% to 5.7%[12,13]. It has been reported in patients between 26 years and 83 years of age, with the highest occurrence in patients over 70 years of age[14-17]. Women are more prone to PE, with a reported prevalence of 67.5%[18]. The timing of a PE diagnosis ranges from day 1 to day 3 during inpatient care and from day 4 to day 90 after discharge from the hospital[11,15,19,20].
Regarding the primary diagnosis, patients have a two-fold increased risk of experiencing a PE compared with those with osteoarthritis[18]. Regarding the type of surgery, shoulder arthroscopy is associated with the lowest incidence of PE and fixation of proximal humerus fractures have the highest risk of occurrence[21]. The reported incidence of PE following shoulder arthroscopy ranges from 0.01% to 5.7%[12]. Arthroscopic procedures in ambulatory surgical centres are associated with a lower risk of PE than those performed in hospital-based outpatient departments[22,23]. The prevalence of PE following shoulder arthroplasty is reported to be 0.1% to 3%[24,25]. Hemiarthroplasty is associated with a lower incidence of PE than total shoulder arthroplasty (TSA), but anatomic TSA and reverse TSA have similar risk levels[24]. The frequencies of PE after TSA for proximal humerus fractures, osteoarthritis, or rotator cuff arthropathy are similar[26]. The percentage of PE after proximal humerus fracture fixation ranges from 0.3% to 3.3%[21,27]. Interestingly, both open reduction and internal fixation (referred to as ORIF) procedures have a higher prevalence of PE than closed reduction and internal fixation[28]. After readmission for other reasons during the postoperative period following SS, the rates of PE have been reported as 0.25% to 0.3%[29].
While PE in the setting of SS is frequently reported secondary to DVTs in upper or lower extremities, it may occur without a concomitant DVT[15,30] (Table 1). Remarkably, PE seems to be more frequent than DVT after SS[31], and on some occasions, no pre-existing risk factors were identified[32,33]. In a large retrospective study, including 42237 patients, Young et al[18] correlated PE after TSA in patients with a history of proximal humerus fracture, deficiency anaemia, congestive heart failure, chronic lung disease, increased age, obesity, and fluid and electrolyte abnormalities. Longer surgical time and subsequent days of postoperative care have been also reported as significant risk factors[34]. The metabolic syndrome, which includes hypertension, diabetes mellitus, obesity and dyslipidaemia, has also been found to be significantly associated with an increased incidence of PE after SS[35]. In addition, Damodar et al[36] found that patients treated at an altitude over 4000 feet had nearly twice the risk of having postoperative PE than those treated at centres at sea level.
| General | Pulmonary embolism without deep vein thrombosis | Pulmonary embolism with deep vein thrombosis |
| Increased age; deficiency anaemia; congestive heart failure; chronic lung disease; metabolic syndrome; obesity; fluid and electrolyte abnormalities; proximal humerus fracture; TSA rather than HA; longer surgical time; longer hospitalization; higher altitude (over 4000 feet) | Older than 75 years of age; hypertension; diabetes mellitus; obesity; peripheral arterial disease; prolonged duration of surgery; history of cancer; congenital thrombophilia; prothrombin gene mutation; beta-thalassemia minor | Older than 40 years of age; hypertension; diabetes mellitus; obesity; smoking; personal or family history of thrombosis and thrombophilia; immobilization of the arm; pregnancy; oral contraceptive use; malignancy; central venous catheters; implantable cardiac rhythm devices |
The most common associated risk factors for primary PE after SS are an age of more than 75 years, peripheral arterial disease, hypertension, diabetes mellitus, obesity, prolonged duration of surgery, and a history of cancer[11,28,37,38]. Genetic conditions, such as congenital thrombophilia, prothrombin gene mutation, and beta-thalassemia minor have also been reported as predisposing factors[14,27]. Tranexamic acid, which is commonly used during shoulder arthroscopy and arthroplasty to limit blood loss and postoperative hematoma formation, does not seem to affect the risk of PE[39,40]. Similarly, the use of oral contraceptive pills has not been clearly related to an increased risk of PE after SS[41].
PE following SS may be secondary to DVT of upper or lower extremities[37,42]. Thrombosis of the cephalic and subclavian veins subsequent to blood clot formation in the arm have also been described[43,44]. In such cases, the predisposing factors for PE are similar to those associated with DVT of the upper extremities and include central venous catheters, implantable cardiac rhythm devices, a personal or family history of thrombosis and thrombophilia, immobilization of the arm, pregnancy, use of oral contraceptives, and malignancy[45].
Lower-extremity thrombosis and PE may also be encountered after SS[46]. A personal or family history of VTE, congenital prothrombotic disorders, smoking, obesity, recent surgery or immobility, a history of cancer, pregnancy, combined hormonal contraceptives or hormone replacement therapy have been associated with an increased likelihood of developing lower-extremity DVTs[47]. Other patient characteristics include an age of more than 40 years, hypertension, diabetes mellitus, inflammatory bowel disease, rheumatic diseases, heart failure, spinal cord injury, and a Glasgow Coma Scale score of less than 8[37,48].
PE after SS usually occurs following DVT of the upper or lower extremities[37,49-51]. The subclavian, axillary, brachial, and cephalic veins have been reported as sources of emboli from the upper limb[42,50,52]. The Virchow triad includes three factors that may lead to development of vascular thrombosis, namely hypercoagulability of the blood, alteration of blood flow, and endothelial damage[53].
Except for coagulopathy and anatomical factors, compression from the shaver or oedema from serum infusion during the operation, the beach-chair position, and elevated traction have been proposed as possible causes of regional DVT during shoulder arthroscopy[44,54]. In patients undergoing shoulder arthroplasty, the axillary vein may be damaged secondary to extreme traction, repeated rotation, position in extension, or by direct pressure from the retractors[55,56]. In some circumstances, the source of the PE remains unclear[30,38,57]. A DVT at the elbow or wrist after SS might be missed because the thrombus causing the PE had already been shed at the time of investigation, leaving only small residual thrombi to detect[54,58]. A right atrial thrombus secondary to atrial fibrillation has previously been implicated as a potential source of PE[58].
Prophylaxis for VTE following SS remains a topic of debate. To date, the standard of care after SS does not routinely require prophylactic medication[59,60]. It is generally believed that early ambulation and rehabilitation beginning on the same day or the first day after the operation protects patients from VTE events[61]. The National Institute for Health and Care Excellence (commonly known as NICE) guidelines for VTE prevention recommend pharmacological thromboprophylaxis in high-risk patients with one or more of the proposed risk factors (Table 2).
| Over 60 years of age |
| Obesity (BMI > 30 kg/m2) |
| Known thrombophilia |
| Dehydration |
| Active cancer or cancer treatment |
| One or more significant medical comorbidity |
| Personal history or first degree relative with a history of VTE |
| Varicose veins with phlebitis |
| Hormone replacement therapy |
| Oestrogen-containing contraceptive therapy |
| Pregnancy or delivery in the previous 6 weeks |
Regarding upper-extremity surgery, VTE prophylaxis is recommended in shoulder operations performed under general anaesthesia that lasts more than 90 min or when the patient’s condition does not allow early postoperative mobilization[62]. Recently, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) disease has been considered an additional risk factor for appearance of thromboembolic events[63].
Early ambulation, elastic stockings, foot impulse devices, and sequential compression devices on the lower extremities are widely used in the perioperative period after SS[64,65]. Medical agents used for prophylaxis in high-risk patients include aspirin, low-molecular-weight heparin, vitamin K antagonists, fondaparinux, and newer oral anticoagulants[66]. Daily administration of aspirin at 325 mg has been suggested in patients who are SARS-CoV-2-positive, in the immediate postoperative period after SS[67].
The repair of proximal humerus fractures may also require VTE chemoprophylaxis. Hoxie et al[33] reported that 7 of 137 patients treated with ORIF or hemiarthroplasty after isolated proximal humerus fractures developed a PE following procedures in which no pharmacological agents were used for VTE prevention. Only thromboembolic deterrent stockings and sequential compression devices were used. Widmer et al[68] reported that oral aspirin, pneumatic compression pumps, and early ambulation were effective for the prevention of VTE after ORIF of proximal humerus fractures. None of the 50 patients included in the study developed DVT or PE.
Shoulder arthroscopy is considered a safe procedure with a low incidence of VTE[46]. Mechanical prophylaxis alone seems to be enough for the prevention of VTE. Only 1 of 175 patients was diagnosed with asymptomatic PE following shoulder arthroscopy in a study of Takahashi et al[57], where only foot pumps or elastic stockings were used for VTE prophylaxis. Alyea et al[69] compared the effectiveness of mechanical prophylaxis alone or with concomitant aspirin administration and found no additional benefit of aspirin in cases undergoing arthroscopic rotator cuff repair.
An increase in the use of drugs for VTE prevention, especially aspirin and direct Factor Xa inhibitors, after shoulder arthroplasty has been reported recently[70]. However, the routine use of thromboprophylaxis in shoulder arthroplasty remains debatable[71]. Kirsch et al[72] found that a low dose of aspirin (81 mg) once daily for 6 weeks was associated with a low risk of VTE after primary shoulder arthroplasty. The authors recommended preoperative medical-risk stratification, but Kolz et al[15] reported that 5 of 10 patients with PE after elective shoulder arthroplasty had been taking aspirin (81 mg) daily, which makes the effectiveness of aspirin alone for VTE prophylaxis questionable.
In general, chest pain and shortness of breath are the two most frequent symptoms of PE[73]. These symptoms also present in patients experiencing PE after SS[19,25]. Hypoxia, hypocapnia, tachypnoea, palpitations, tachycardia, and signs of right-side cardiac stress on electrocardiography are other possible clinical signs[73]. When PE occurs following DVT, swelling and a new onset of pain in the extremities are common[58]. Congestion of superficial veins, cyanosis of the hands, finger paraesthesia, and functional impairment may also be present[32]. PE after SS is rarely asymptomatic[58,64]. This is explained by an intrinsic tolerance in hypoxia, which may be related to living at a high altitude for a long time or presence of chronic obstructive pulmonary disease[74].
In asymptomatic cases, low arterial oxygen saturation and elevated D-dimers may raise suspicion of this condition. However, as they may be transiently elevated because of the operation, they cannot confirm the diagnosis[58]. Computed tomography pulmonary angiography is the current gold standard for the diagnosis of PE, and it has replaced ventilation-perfusion lung scintigraphy and pulmonary angiography[75]. In fatal cases, PE after SS has been diagnosed only during post-mortem examinations[51,56].
Anticoagulant therapy is the mainstay for the treatment of PE and is classically divided into three phases. In the acute phase (i.e. the first 5 days to 10 days after diagnosis) the treatment options include subcutaneous injection of low-molecular-weight heparin or fondaparinux, intravenous unfractionated heparin, or the oral Factor Xa inhibitors rivaroxaban and apixaban[76]. In the second phase (i.e. the next 3 months to 6 months) direct oral anticoagulants or vitamin K antagonists are usually administered[77,78]. An overlap period of administering oral agents with heparins or fondaparinux is required until the former reach effective levels[75]. Oral anticoagulants include the thrombin inhibitor dabigatran etexilate and the Factor Xa inhibitors rivaroxaban, apixaban, and edoxaban[73]. These agents have been proven equivalent to vitamin K antagonists but with lower risk of clinically relevant bleeding and no need to monitor the international normalized ratio[75]. In the event of PE after SS, warfarin is commonly used for up to 6 months during this period[11,15,19,33]. In the last phase, medical treatment is continued in high-risk patients for preventing PE recurrence. The optimal duration of this phase is estimated by weighting the risk of recurrence and bleeding[79].
Patients with PE who are hemodynamically stable are at low risk of death and can usually be discharged within the first 2 days after diagnosis[80]. However, PE may be associated with hemodynamic instability and a high risk of early mortality[73]. In such cases, immediate intravenous administration of thrombolytic agents is needed to promptly restore pulmonary perfusion. Extended hospitalization may be required[79].
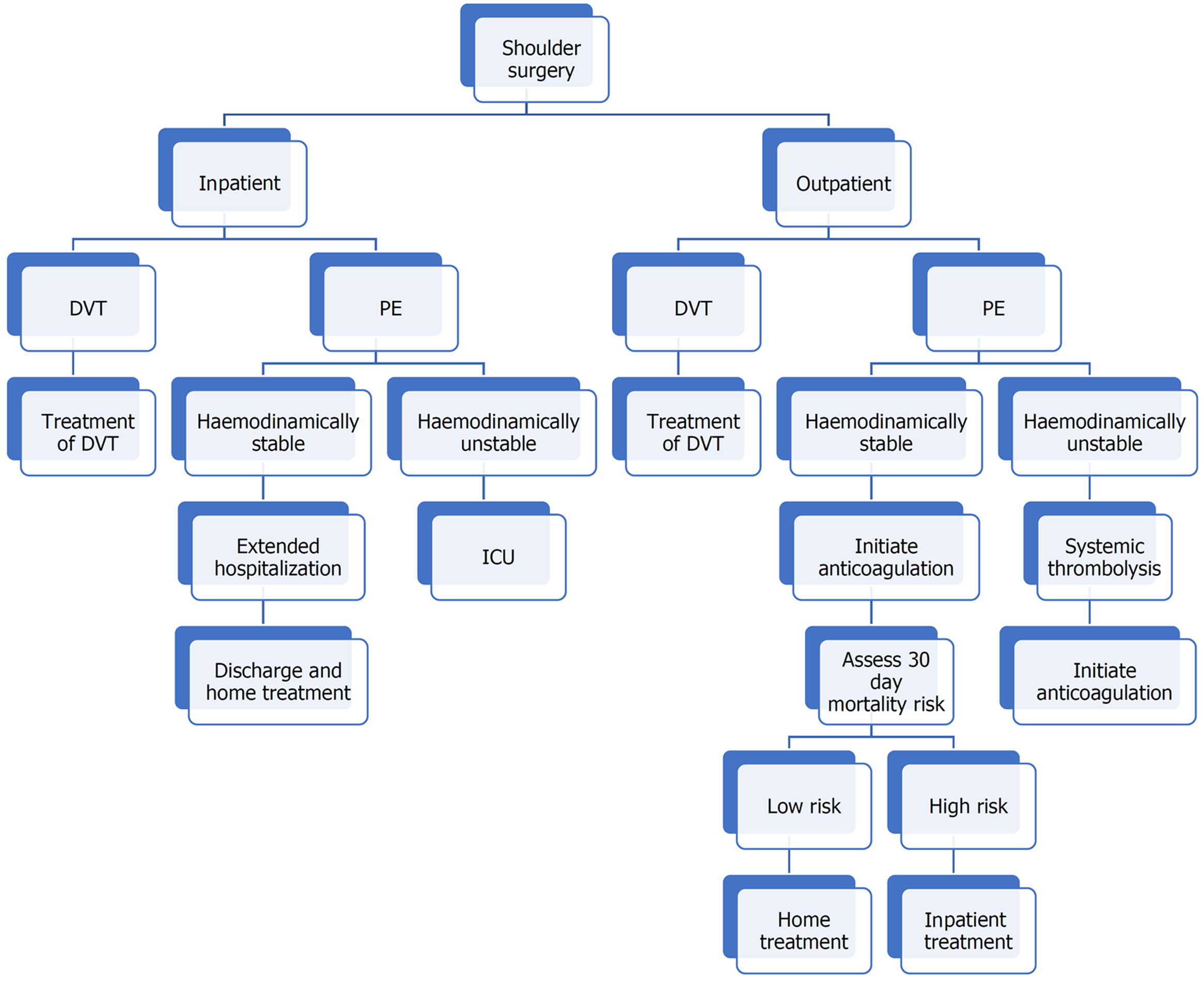
Most patients with PE after SS are properly treated[14,15,20,37]. Extended hospitalization or transfer to an intensive care unit are often needed until the patient is considered sufficiently stable for discharge[25]. PE secondary to cardiopulmonary arrest is rarely fatal[43,49]. The PE Severity Index uses 11 clinical criteria to predict the 30-day outcome of patients with PE[81]. An algorithm for the management of PE after SS is shown in Figure 1.
In most patients, the functional outcome of the surgical procedure is not affected but a delay in rehabilitation should be expected[11,67]. Although strenuous exercise and squeezing of the arm are contraindicated, the evidence that physiotherapy of the shoulder should be avoided or modified is not sufficient[58]. The shoulder pathology and postoperative recommendations indicate that early passive or gentle active range-of-motion exercises can be commenced and continue until joint function is restored. However, data regarding the frequency, intensity, and duration of exercises are not available, and no specific rehabilitation protocol exists[42,67].
Stiffness is the most common complication and may take up to 6 months to resolve[32]. Aggressive physiotherapy and interventions, such as intra-articular injections or manipulation under aesthesia, may be needed if the joint range-of-motion does not improve postoperatively[37]. In rare cases, PE may lead to delayed recovery, persisting pain, and inability to reach former levels of strength, performance, and sports activity[50].
PE is a rare but potentially fatal complication after SS. Clinicians should have a high degree of suspicion for PE if respiratory difficulty develops in the postoperative period. While thromboprophylaxis following SS remains a topic of debate, the number of risk factors predisposing to the development of PE continues to increase. Prevention and early diagnosis and treatment are of utmost importance to limit the associated morbidity and mortality. As early physiotherapy and range-of-motion exercises do not adversely affect the prognosis of PE, they are highly recommended to preserve shoulder mobility and function.
| 1. | Blitzer RR, Eisenstein S. Venous Thromboembolism and Pulmonary Embolism: Strategies for Prevention and Management. Surg Clin North Am. 2021;101:925-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 2. | Essien EO, Rali P, Mathai SC. Pulmonary Embolism. Med Clin North Am. 2019;103:549-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 104] [Article Influence: 17.3] [Reference Citation Analysis (1)] |
| 3. | Meignan M, Rosso J, Gauthier H, Brunengo F, Claudel S, Sagnard L, d'Azemar P, Simonneau G, Charbonnier B. Systematic lung scans reveal a high frequency of silent pulmonary embolism in patients with proximal deep venous thrombosis. Arch Intern Med. 2000;160:159-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 150] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 4. | Westermann RW, Pugely AJ, Ries Z, Amendola A, Martin CT, Gao Y, Wolf BR. Causes and Predictors of 30-Day Readmission After Shoulder and Knee Arthroscopy: An Analysis of 15,167 Cases. Arthroscopy. 2015;31:1035-1040.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 5. | Xu S, Baker DK, Woods JC, Brabston EW 3rd, Ponce BA. Risk Factors for Early Readmission After Anatomical or Reverse Total Shoulder Arthroplasty. Am J Orthop (Belle Mead NJ). 2016;45:E386-E392. [PubMed] |
| 6. | Hill JR, McKnight B, Pannell WC, Heckmann N, Sivasundaram L, Mostofi A, Omid R, Rick Hatch GF 3rd. Risk Factors for 30-Day Readmission Following Shoulder Arthroscopy. Arthroscopy. 2017;33:55-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 62] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 7. | Na SS, Kim DH, Choi BC, Cho CH. Incidence, characteristics, and risk factors of venous thromboembolism in shoulder arthroplasty-a systematic review. Int Orthop. 2022;46:2081-2088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Gür V, Yapici F, Subaşı IÖ, Gökgöz MB, Tosun M, Tardus I, Koçkara N. Incidence and Factors Associated With Pulmonary Embolism After Upper Extremity Trauma: A Tertiary Hospital Experience in Turkey. Cureus. 2023;15:e41077. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Cogan CJ, Flores SE, Freshman RD, Chi HM, Feeley BT. Effect of obesity on short- and long-term complications of shoulder arthroplasty. J Shoulder Elbow Surg. 2023;32:253-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 22] [Reference Citation Analysis (0)] |
| 10. | Ojike NI, Bhadra AK, Giannoudis PV, Roberts CS. Venous thromboembolism in shoulder surgery: a systematic review. Acta Orthop Belg. 2011;77:281-289. [PubMed] |
| 11. | Durant TJ, Cote MP, Arciero RA, Mazzocca AD. Fatal pulmonary embolism after arthroscopic rotator cuff repair: a case series. Muscles Ligaments Tendons J. 2014;4:232-237. [PubMed] |
| 12. | Li T, Li Y, Zhang L, Pang L, Tang X, Zhu J. Venous thromboembolism after arthroscopic shoulder surgery: a systematic review. J Orthop Surg Res. 2023;18:103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Rees JL, Craig R, Nagra N, Baldwin M, Lane JCE, Price A, Beard DJ, Abram S, Judge A, Prieto-Alhambra D, Furniss D, Carr AJ. Serious adverse event rates and reoperation after arthroscopic shoulder surgery: population based cohort study. BMJ. 2022;378:e069901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 14. | Edgar R, Nagda S, Huffman R, Namdari S. Pulmonary embolism after shoulder arthroscopy. Orthopedics. 2012;35:e1673-e1676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Kolz JM, Aibinder WR, Adams RA, Cofield RH, Sperling JW. Symptomatic Thromboembolic Complications After Shoulder Arthroplasty: An Update. J Bone Joint Surg Am. 2019;101:1845-1851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Gupta P, Quan T, Zimmer ZR. Thirty-day morbidity and mortality following revision total shoulder arthroplasty in octogenarians. Shoulder Elbow. 2022;14:402-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | White CA, Duey A, Zaidat B, Li T, Quinones A, Cho SK, Kim JS, Cagle PJ. Does age at surgery influence short-term outcomes and readmissions following anatomic total shoulder arthroplasty? J Orthop. 2023;37:69-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 18. | Young BL, Menendez ME, Baker DK, Ponce BA. Factors associated with in-hospital pulmonary embolism after shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24:e271-e278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | Hoxie SC, Sperling JW, Cofield RH. Pulmonary embolism following rotator cuff repair. Int J Shoulder Surg. 2008;2:49-51. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Imberti D, Dentali F, Ivaldo N, Murena L, Paladini P, Castagna A, Barillari G, Guerra E, Tonello C, Castoldi F, Lazzaro F, Benedetti R, Camporese G, Porcellini G; RECOS Investigators. Venous Thromboembolism in Patients Undergoing Shoulder Arthroscopy: Findings From the RECOS Registry. Clin Appl Thromb Hemost. 2015;21:486-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Jameson SS, James P, Howcroft DW, Serrano-Pedraza I, Rangan A, Reed MR, Candal-Couto J. Venous thromboembolic events are rare after shoulder surgery: analysis of a national database. J Shoulder Elbow Surg. 2011;20:764-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 60] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 22. | Qin C, Curtis DM, Reider B, Shi LL, Lee MJ, Athiviraham A. Orthopaedic Shoulder Surgery in the Ambulatory Surgical Center: Safety and Outcomes. Arthroscopy. 2019;35:2545-2550.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 23. | Randelli P, Castagna A, Cabitza F, Cabitza P, Arrigoni P, Denti M. Infectious and thromboembolic complications of arthroscopic shoulder surgery. J Shoulder Elbow Surg. 2010;19:97-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 69] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 24. | Jiang JJ, Toor AS, Shi LL, Koh JL. Analysis of perioperative complications in patients after total shoulder arthroplasty and reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1852-1859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 25. | Willis AA, Warren RF, Craig EV, Adler RS, Cordasco FA, Lyman S, Fealy S. Deep vein thrombosis after reconstructive shoulder arthroplasty: a prospective observational study. J Shoulder Elbow Surg. 2009;18:100-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 57] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 26. | Lung BE, Kanjiya S, Bisogno M, Komatsu DE, Wang ED. Preoperative indications for total shoulder arthroplasty predict adverse postoperative complications. JSES Open Access. 2019;3:99-107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 27. | Heyer JH, Parker RL, Lynch T, Parry T, Neviaser AS. Rate of venous thromboembolism after surgical treatment of proximal humerus fractures. Arch Orthop Trauma Surg. 2021;141:403-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | Petrigliano FA, Bezrukov N, Gamradt SC, SooHoo NF. Factors predicting complication and reoperation rates following surgical fixation of proximal humeral fractures. J Bone Joint Surg Am. 2014;96:1544-1551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 29. | Day JS, Ramsey ML, Lau E, Williams GR. Risk of venous thromboembolism after shoulder arthroplasty in the Medicare population. J Shoulder Elbow Surg. 2015;24:98-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 30. | Dal Molin FF, Dal Molin SF. THROMBOEMBOLIC COMPLICATION AFTER ARTHROSCOPIC SHOULDER SURGERY. Rev Bras Ortop. 2010;45:312-315. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 31. | Singh JA, Sperling JW, Cofield RH. Cardiopulmonary complications after primary shoulder arthroplasty: a cohort study. Semin Arthritis Rheum. 2012;41:689-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 32. | Goldhaber NH, Lee CS. Isolated Pulmonary Embolism following Shoulder Arthroscopy. Case Rep Orthop. 2014;2014:279082. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 33. | Hoxie SC, Sperling JW, Cofield RH. Pulmonary embolism after operative treatment of proximal humeral fractures. J Shoulder Elbow Surg. 2007;16:782-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 34. | Zhang D, Dyer GSM, Earp BE. Venous Thromboembolism After Total Shoulder Arthroplasty: A Database Study of 31,918 Cases. J Am Acad Orthop Surg. 2022;30:949-956. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 35. | Murphy AB, Menendez ME, Watson SL, Ponce BA. Metabolic syndrome and shoulder arthroplasty: epidemiology and peri-operative outcomes. Int Orthop. 2016;40:1927-1933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 36. | Damodar D, Vakharia R, Vakharia A, Sheu J, Donnally CJ 3rd, Levy JC, Kaplan L, Munoz J. A higher altitude is an independent risk factor for venous thromboembolisms following total shoulder arthroplasty. J Orthop. 2018;15:1017-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 37. | Kuremsky MA, Cain EL Jr, Fleischli JE. Thromboembolic phenomena after arthroscopic shoulder surgery. Arthroscopy. 2011;27:1614-1619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 38. | Yamamoto T, Tamai K, Akutsu M, Tomizawa K, Sukegawa T, Nohara Y. Pulmonary embolism after arthroscopic rotator cuff repair: a case report. Case Rep Orthop. 2013;2013:801752. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 39. | Carbone A, Poeran J, Zubizarreta N, Chan J, Mazumdar M, Parsons BO, Galatz LM, Cagle PJ. Administration of tranexamic acid during total shoulder arthroplasty is not associated with increased risk of complications in patients with a history of thrombotic events. J Shoulder Elbow Surg. 2021;30:104-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 40. | Sun Y, Xiao D, Fu W, Cai W, Huang X, Li Q, Li J. Efficacy and Safety of Tranexamic Acid in Shoulder Arthroscopic Surgery: A Systematic Review and Meta-Analysis. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 41. | Stone AV, Agarwalla A, Gowd AK, Jacobs CA, Macalena JA, Lesniak BP, Verma NN, Romeo AA, Forsythe B. Oral Contraceptive Pills Are Not a Risk Factor for Deep Vein Thrombosis or Pulmonary Embolism After Arthroscopic Shoulder Surgery. Orthop J Sports Med. 2019;7:2325967118822970. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 42. | Watanabe H, Nagase Y, Tamai K, Tanaka S. Pulmonary embolism associated with upper extremity deep venous thrombosis after shoulder arthroscopy: A case report. J Orthop Sci. 2019;24:746-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 43. | Li Y, Wang Z, Sang X. Subclavian vein thrombosis and fatal pulmonary embolism after proximal humerus fracture surgery. J Orthop Surg (Hong Kong). 2019;27:2309499019832728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 44. | Polzhofer GK, Petersen W, Hassenpflug J. Thromboembolic complication after arthroscopic shoulder surgery. Arthroscopy. 2003;19:E129-E132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 45. | Singh O, Juneja D. Upper extremity deep vein thrombosis: An intensivist's perspective. World J Crit Care Med. 2023;12:130-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (3)] |
| 46. | Schick CW, Westermann RW, Gao Y; ACESS Group, Wolf BR. Thromboembolism Following Shoulder Arthroscopy: A Retrospective Review. Orthop J Sports Med. 2014;2:2325967114559506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 47. | Jones NR, Round T. Venous thromboembolism management and the new NICE guidance: what the busy GP needs to know. Br J Gen Pract. 2021;71:379-380. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 48. | Paydar S, Sabetian G, Khalili H, Fallahi J, Tahami M, Ziaian B, Abbasi HR, Bolandparvaz S, Ghaffarpasand F, Ghahramani Z. Management of Deep Vein Thrombosis (DVT) Prophylaxis in Trauma Patients. Bull Emerg Trauma. 2016;4:1-7. [PubMed] |
| 49. | Kim SJ, Yoo KY, Lee HG, Kim WM, Jeong CW, Lee HJ. Fatal pulmonary embolism caused by thrombosis of contralateral axillary vein after arthroscopic right rotator cuff repair -A case report-. Korean J Anesthesiol. 2010;59 Suppl:S172-S175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 50. | Hariri A, Nourissat G, Dumontier C, Doursounian L. Pulmonary embolism following thrombosis of the brachial vein after shoulder arthroscopy. A case report. Orthop Traumatol Surg Res. 2009;95:377-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 51. | Madhusudhan TR, Shetty SK, Madhusudhan S, Sinha A. Fatal pulmonary embolism following shoulder arthroplasty: a case report. J Med Case Rep. 2009;3:8708. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 52. | Creighton RA, Cole BJ. Upper-extremity deep venous thrombosis after shoulder arthroscopy: a case report. J Shoulder Elbow Surg. 2007;16:e20-e22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 53. | Kushner A, West WP, Khan Suheb MZ, Pillarisetty LS. Virchow Triad. 2024 Jun 7. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 54. | Cortés ZE, Hammerman SM, Gartsman GM. Pulmonary embolism after shoulder arthroscopy: could patient positioning and traction make a difference? J Shoulder Elbow Surg. 2007;16:e16-e17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 55. | Arcand M, Burkhead WZ Jr, Zeman C. Pulmonary embolism caused by thrombosis of the axillary vein after shoulder arthroplasty. J Shoulder Elbow Surg. 1997;6:486-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 56. | Saleem A, Markel DC. Fatal pulmonary embolus after shoulder arthroplasty. J Arthroplasty. 2001;16:400-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 57. | Takahashi H, Yamamoto N, Nagamoto H, Sano H, Tanaka M, Itoi E. Venous thromboembolism after elective shoulder surgery: a prospective cohort study of 175 patients. J Shoulder Elbow Surg. 2014;23:605-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 58. | Ji L, Lyu CL, Feng M, Qiang H. Asymptomatic Pulmonary Embolism After Shoulder Arthroscopy: Case Report and Literature Review. Orthop Surg. 2021;13:1119-1125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 59. | Geerts WH, Pineo GF, Heit JA, Bergqvist D, Lassen MR, Colwell CW, Ray JG. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:338S-400S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2163] [Cited by in RCA: 1964] [Article Influence: 93.5] [Reference Citation Analysis (0)] |
| 60. | Mismetti P, Zufferey P, Pernod G, Baylot, Estebe JP, Barrelier MT, Pegoix M, Nertl P. Thromboprohylaxis in orthopedic surgery and traumatology. Ann Fr Anesth Reanim. 2005;24:871-889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 61. | Rockwood CA Jr, Wirth MA, Blair S. Warning: pulmonary embolism can occur after elective shoulder surgery-report of two cases and survey of the members of the American Shoulder and Elbow Surgeons. J Shoulder Elbow Surg. 2003;12:628-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 62. | Venous thromboembolism in over 16s: Reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism. London: National Institute for Health and Care Excellence (NICE); 2018 Mar- . [PubMed] |
| 63. | Miesbach W, Makris M. COVID-19: Coagulopathy, Risk of Thrombosis, and the Rationale for Anticoagulation. Clin Appl Thromb Hemost. 2020;26:1076029620938149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 259] [Cited by in RCA: 264] [Article Influence: 52.8] [Reference Citation Analysis (0)] |
| 64. | Aibinder WR, Sanchez-Sotelo J. Venous Thromboembolism Prophylaxis in Shoulder Surgery. Orthop Clin North Am. 2018;49:257-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 65. | Hill J, Treasure T; Guideline Development Group. Reducing the risk of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in patients admitted to hospital: summary of the NICE guideline. Heart. 2010;96:879-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 124] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 66. | Flevas DA, Megaloikonomos PD, Dimopoulos L, Mitsiokapa E, Koulouvaris P, Mavrogenis AF. Thromboembolism prophylaxis in orthopaedics: an update. EFORT Open Rev. 2018;3:136-148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 152] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 67. | Chauhan A, Villacis D, Boente R, Romeo AA. Venous thromboembolism after arthroscopic rotator cuff repair in a patient with a negative presurgical SARS-CoV-2 test who developed symptomatic COVID-19 three days after surgery. J Shoulder Elbow Surg. 2021;30:e251-e255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 68. | Widmer BJ, Bassora R, Warrender WJ, Abboud JA. Thromboembolic events are uncommon after open treatment of proximal humerus fractures using aspirin and compression devices. Clin Orthop Relat Res. 2011;469:3332-3336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 69. | Alyea E, Gaston T, Austin LS, Wowkanech C, Cypel B, Pontes M, Williams G. The Effectiveness of Aspirin for Venous Thromboembolism Prophylaxis for Patients Undergoing Arthroscopic Rotator Cuff Repair. Orthopedics. 2019;42:e187-e192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 70. | Agarwal AR, Ahmed AF, Stadecker M, Miller AS, Best MJ, Srikumaran U. Trends in Venous Thromboembolism After Shoulder Arthroplasty in the United States: Analysis Following the 2009 American Academy of Orthopaedic Surgeons Clinical Practical Guidelines. J Am Acad Orthop Surg. 2023;31:364-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 71. | Hole RM, Fenstad AM, Gjertsen JE, Lie SA, Furnes O. Thromboprophylaxis in primary shoulder arthroplasty does not seem to prevent death: a report from the Norwegian Arthroplasty Register 2005-2018. Acta Orthop. 2021;92:401-407. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 72. | Kirsch JM, Gutman M, Patel M, Rondon A, Ramsey ML, Abboud JA, Williams GR, Namdari S. Low-dose aspirin and the rate of symptomatic venous thromboembolic complications following primary shoulder arthroplasty. J Shoulder Elbow Surg. 2021;30:1613-1618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 73. | Freund Y, Cohen-Aubart F, Bloom B. Acute Pulmonary Embolism: A Review. JAMA. 2022;328:1336-1345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 121] [Article Influence: 40.3] [Reference Citation Analysis (0)] |
| 74. | Cancienne JM, Burrus MT, Diduch DR, Werner BC. High altitude is an independent risk factor for venous thromboembolism following arthroscopic rotator cuff repair: a matched case-control study in Medicare patients. J Shoulder Elbow Surg. 2017;26:7-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 75. | Di Nisio M, van Es N, Büller HR. Deep vein thrombosis and pulmonary embolism. Lancet. 2016;388:3060-3073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 411] [Cited by in RCA: 580] [Article Influence: 64.4] [Reference Citation Analysis (0)] |
| 76. | Wells PS, Forgie MA, Rodger MA. Treatment of venous thromboembolism. JAMA. 2014;311:717-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 144] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 77. | EINSTEIN–PE Investigators; Büller HR, Prins MH, Lensin AW, Decousus H, Jacobson BF, Minar E, Chlumsky J, Verhamme P, Wells P, Agnelli G, Cohen A, Berkowitz SD, Bounameaux H, Davidson BL, Misselwitz F, Gallus AS, Raskob GE, Schellong S, Segers A. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med. 2012;366:1287-1297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1646] [Cited by in RCA: 1691] [Article Influence: 130.1] [Reference Citation Analysis (0)] |
| 78. | Hokusai-VTE Investigators; Büller HR, Décousus H, Grosso MA, Mercuri M, Middeldorp S, Prins MH, Raskob GE, Schellong SM, Schwocho L, Segers A, Shi M, Verhamme P, Wells P. Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med. 2013;369:1406-1415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1287] [Cited by in RCA: 1341] [Article Influence: 111.8] [Reference Citation Analysis (0)] |
| 79. | Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, Huisman M, King CS, Morris TA, Sood N, Stevens SM, Vintch JRE, Wells P, Woller SC, Moores L. Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report. Chest. 2016;149:315-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3126] [Cited by in RCA: 3434] [Article Influence: 381.6] [Reference Citation Analysis (2)] |
| 80. | Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, Gibbs JS, Huisman MV, Humbert M, Kucher N, Lang I, Lankeit M, Lekakis J, Maack C, Mayer E, Meneveau N, Perrier A, Pruszczyk P, Rasmussen LH, Schindler TH, Svitil P, Vonk Noordegraaf A, Zamorano JL, Zompatori M; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35:3033-3069, 3069a. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1883] [Cited by in RCA: 1896] [Article Influence: 172.4] [Reference Citation Analysis (0)] |
| 81. | Hassine M, Kallala MY, Mahjoub M, Boussaada M, Bouchahda N, Gamra H. [Pulmonary embolism: the Pulmonary Embolism Severity Index (PESI) score and mortality predictors]. Pan Afr Med J. 2023;45:48. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |