Published online Mar 20, 2024. doi: 10.5662/wjm.v14.i1.89853
Peer-review started: November 14, 2023
First decision: November 30, 2023
Revised: December 6, 2023
Accepted: February 2, 2024
Article in press: February 2, 2024
Published online: March 20, 2024
Processing time: 113 Days and 17.8 Hours
The occurrence of thyroid cancer (TC) has increased in recent decades. Exposure to outdoor artificial light at night (ALN) is associated with an increased risk of cancer.
To investigated the impact of ALN, as a significant environmental pollutant, on TC incidence worldwide.
The assessment involved analyzing satellite ALN data in conjunction with TC incidence data [adjusted standardized rate (ASR)], while considering the quality of cancer registries (QCR), gross domestic product (GDP) per person, and health expenditure per person (HEP) for each country.
Results indicated a correlation between higher ASR and ALN exposure percentages, particularly in countries with higher GDP or HEP quartiles (all P< 0.05). Significant differences in ASR were observed across QCR levels, both high and low quality (all P < 0.05), but not in countries without registry activity. However, when evaluating ASR against ALN exposure percentages while considering GDP/HEP quartiles or QCR levels, no significant associations were found (all P > 0.10).
The findings suggest a potential link between higher GDP and adverse health conditions, serving as possible risk factors for TC, rather than a direct association with ALN. Limitations include the use of cross-sectional data, temporal misalign
Core Tip: We explored the impact of outdoor artificial light at night (ALN) on thyroid cancer (TC) worldwide. While a correlation was found between higher TC rates and ALN exposure in countries with greater economic indicators [gross domestic product (GDP) and health expenditure per person (HEP)], the association disappeared when accounting for registry quality. The findings suggest that high GDP may be more closely linked to health conditions and TC risk factors than ALN, possibly indicating a lifestyle connection to carcinogenesis. While correlations between ALN and economic factors are observed, a direct link of ALN to TC remains unconfirmed. Additionally, higher GDP/HEP could contribute to better diagnostic access, aiding TC diagnosis and registry inclusion.
- Citation: Tselebis A, Koukkou E, Milionis C, Zabuliene L, Pachi A, Ilias I. Artificial night light and thyroid cancer. World J Methodol 2024; 14(1): 89853
- URL: https://www.wjgnet.com/2222-0682/full/v14/i1/89853.htm
- DOI: https://dx.doi.org/10.5662/wjm.v14.i1.89853
The occurrence of thyroid cancer (TC) has increased in recent decades, in contrast to the incidence of most solid tumors in developed countries, which either remains stable or decreases. The reasons for this increase are still unclear; this epidemiological discrepancy compared to other neoplasias merits further research. Outdoor artificial light at night (ALN) is ubiquitous in the modern world and exposure to it is one of the major environmental pollutants[1]. Light pollution has increased to such an extent that it no longer affects not only residents of large cities, but also those living in more remote areas. Exposure to ALN is associated with an increased risk of cancer[2]. The association of ALN with carcinogenesis is relatively novel. It has been suggested that exposure to ALN reduces nocturnal production of melatonin, which acts as a tumor suppressor[3]. However, little data focused on TC in relation to light pollution have been presented in the literature so far[3]. In this study we aimed to assess, worldwide, the potential impact of ALN on TC, using available satellite ALN data and reported TC epidemiological data.
To study the potential impact of ALN on TC, published satellite data on light pollution worldwide in 173 countries were used[1] (for a global image of ALN circa 2016, Earth at Night (Black Marble) 2016 Color Maps). In particular, exposure levels-per (%) population and per (%) surface area of each country- to ALN > 87 μcd/m2 and ALN > 688 μcd/m2 (levels at which the ability to view the natural night sky is lost and where the Milky Way is no longer visible, respectively) - were used. These thresholds were chosen because the 87 μcd/m2 level corresponds to 50% more night luminance compared to normal, whereas the 688 μcd/m2 level denotes the total loss of the natural appearance of the night sky[1]. Light pollution data were estimated with reference to the corresponding per country TC incidence data as provided by the World Health Organization and the Global Initiative for Cancer Registry Development (https://gco.iarc.fr/). In particular, we used the standardized per age and per 100.000 population of each country TC incidence adjusted standardized rate (ASR). The normality of the data distribution was assessed by the Kolmogorov-Smirnoff test. To assess financial influences (as an indirect measure of living conditions and lifestyle) data were collected for gross domestic product (GDP) per person for each country (https://data.worldbank.org/indicator/NY.GDP.PCAP.CD) and health expenditure per person (HEP) for each country (https://data.worldbank.org/indicator/SH.XPD.CHEX.PC.CD) from the World Bank. The quality of cancer registries (QCR), classified in three groups as either high quality registries, registries of lower quality or no registry activity, per the Global Initiative for Cancer Registry Development; https://gco.iarc.fr/) was also noted. Comparisons of ASR and ALN exposure percentages were done according to GDP/HEP quartiles or QCR levels with the Kruskall Wallis test (KW, with statistical significance set at P < 0.05). The ASR was evaluated against ALN exposure percentages, conditioned for GDP/HEP quartiles and QCR levels, with Kendall’s Tau test (KT, due to non-normal data distribution, with statistical significance set at P < 0.05). Statistical analyses were done with Minitab v.17.1 (Minitab Inc, State College, PA, United States, 2010) and JASP v0.15 (JASP Team, University of Amsterdam, NL, 2021).
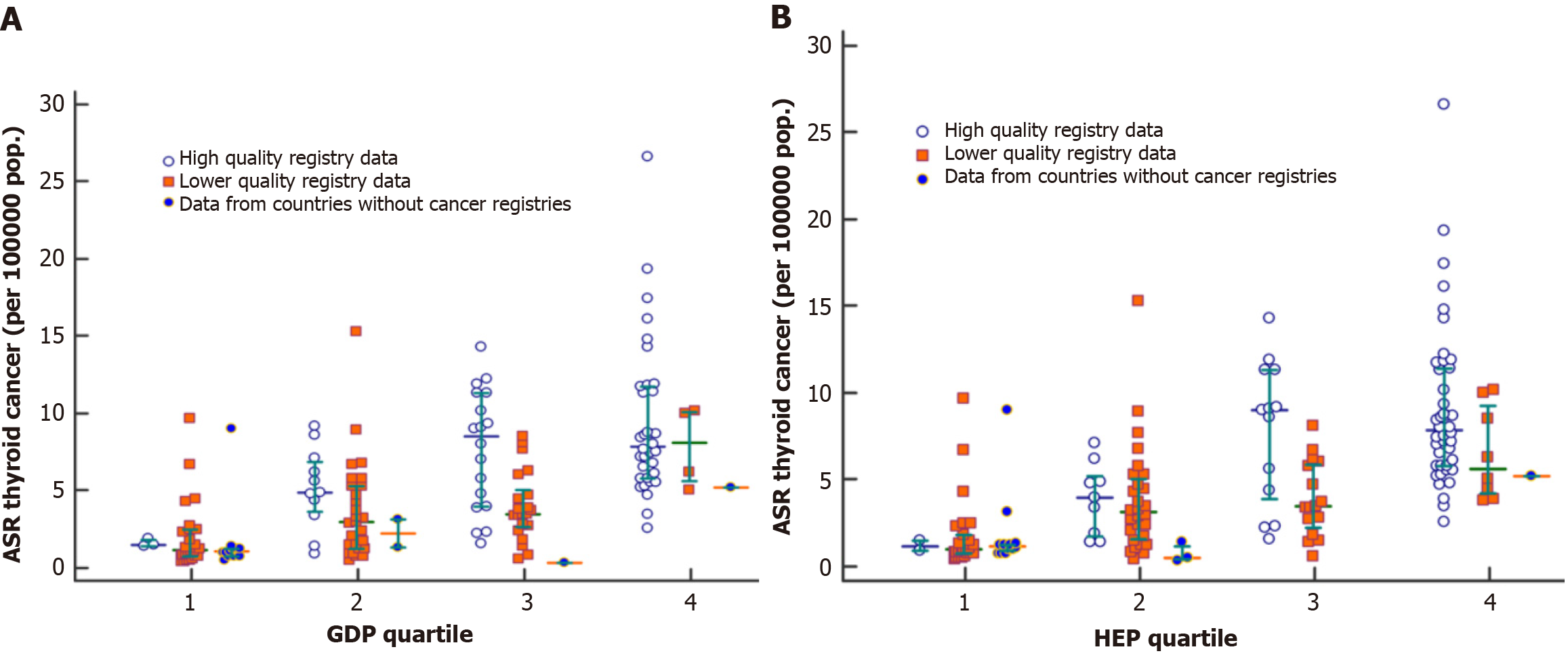
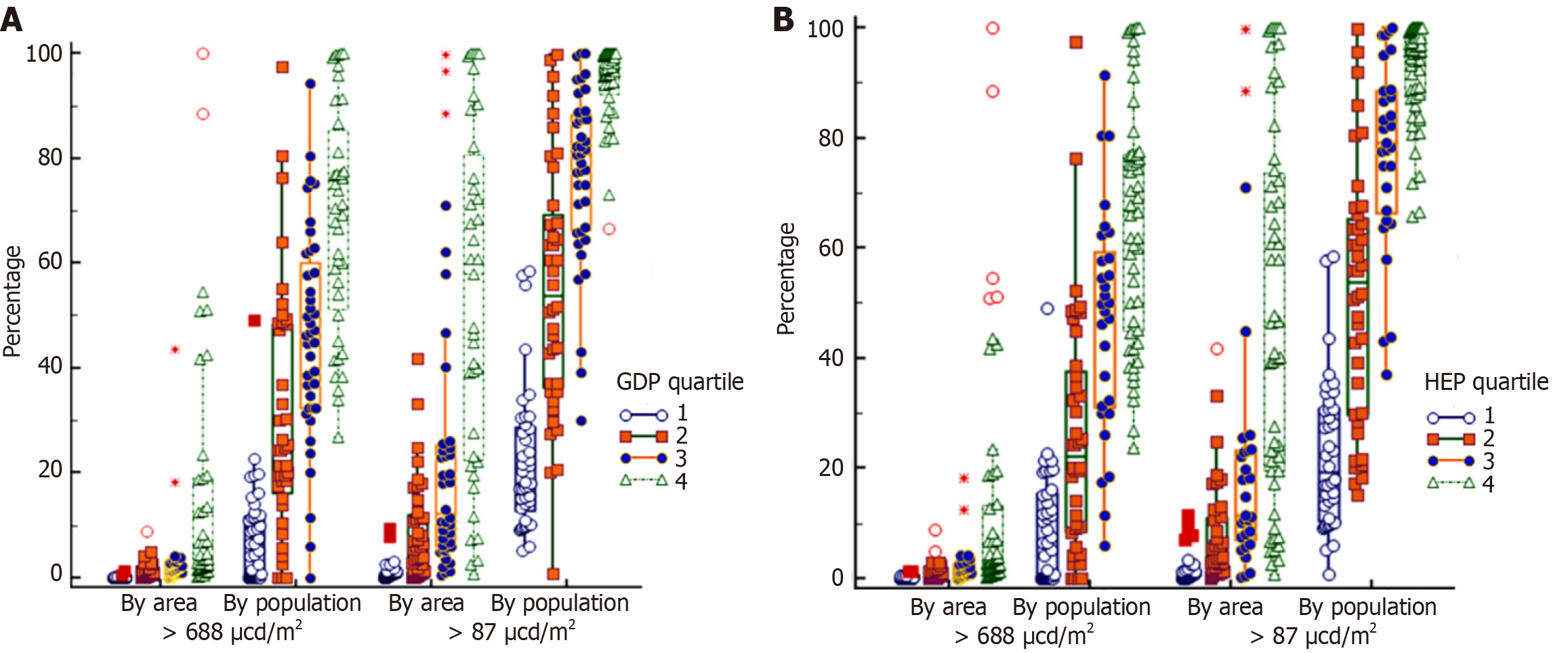
The median value worldwide, per (%) population or per (%) area, of ALN > 87 μcd/m2, was 67.3% and 7.5%, while ALN > 688 μcd/m2 was 34.6% and 0.7%, respectively. The median ASR was 4.2/100000 population. There were significant differences of ASR and ALN exposure percentages by GDP quartiles or HEP quartiles (Figures 1 and 2).
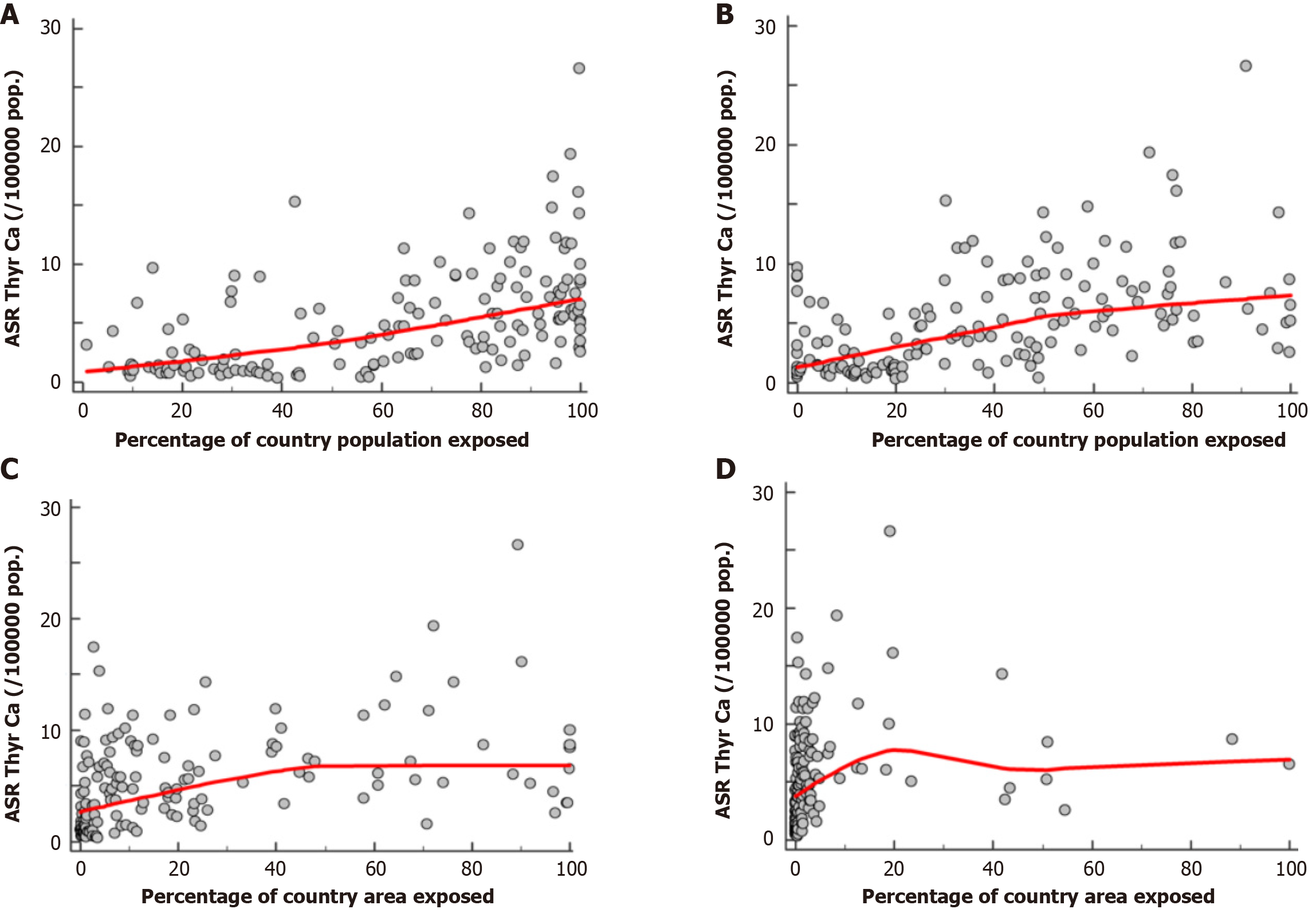
Higher ASR and ALN exposure percentages were noted with higher GDP quartiles or HEP quartiles (all P < 0.05, KW). Differences in ASR were significant for QCR of high quality and lower quality (all P < 0.05, KW), but not for data with countries with no registry activity. Evaluation of ASR against ALN exposure percentages, taking into account GDP/ HEP quartiles or QCR levels did not yield significant results (KT ranged from -0.145 to + 0.272, all P > 0.10) (Figure 3, Supple
The global scale of the ALN problem is illustrated by the fact that, according to available data, 83% of the world’s population lives under conditions of severe light pollution[1]. In our study we aimed to clarify the nature of the relationship between ALN and TC, taking into account GDP or HEP and level of QCR. We noted differences in ASR by GDP quantiles and HEP quantiles worldwide; however ASR was not associated with exposure to ALN. Moreover, the higher the QCR was the higher ASR was noted. Thus, financial indicators were associated with the incidence of TC, whereas ALN was not associated with its incidence.
Currently, the annual rate of TC’s new cases worldwide is increasing, estimated at about 20% from 1990 to 2013. The rise recorded is similar in Europe, the United States of America, Canada and Australia, although changes in increased incidence are greater in low income countries compared to high income countries[4,5]. The causes of this "epidemic" remain largely unclear[6]. It may represent a true increase or simply an increase in diagnoses of subclinical tumors that would otherwise have caused no symptoms, had they gone undetected[7]. Possibly, the ease of diagnosing very small tumors, due to advances in medical technology and screening programs, may play a role[8-10]. Perhaps, however, some factors related to lifestyle are also to blame.
Research has already identified some factors that affect the likelihood of developing TC. Genetics, exposure to ionizing radiation and iodine intake have been found to increase the risk[4]. There are also studies that have associated air pollution, obesity, smoking and alcohol intake to TC[11,12]. Recently, a study published also inculpated light pollution[3]. The researchers reported that city lights at night suppress melatonin (which may regulate estrogen activity, has antineoplastic properties and assists in the adaptability of humans to their environment) and disrupts circadian rhythms, which is also a risk factor for carcinogenesis[13].
Regarding the data that we used, the satellite night illumination data used in this work were from 2016; these were obtained with Visible Infrared Imaging Radiometer Suite (VIIRS), and are considered to be very accurate[1]. The VIIRS ALN data are also considered to be a proxy of socioeconomic conditions. Data for the latter, which we used, were from 2019 and 2020, mostly before or at the beginning of the coronavirus disease 2019 pandemic. The TC incidence data which were used were also from 2019-2020. Experts argue that the latency period from the beginning of the neoplastic process to diagnosis of TC is approximately 2.5 years[14]. Thus, for ALN vs TC incidence, this study takes into consideration this lag time. However, the temporal misalignment of cross-sectional data from different years (2016 for ALN, 2019-2020 for TC incidence, and 2019-2020 for economic data) may have affected the accuracy of the associations studied, especially considering the latency period for TC. Another limitation of the study is that the accuracy of epidemiological data for cancer incidence may not be satisfactory in countries with low quality cancer registries or without cancer registries. This introduces potential bias, as the accuracy of TC data may vary widely between countries. The VIIRS ALN data may be a proxy of socioeconomic conditions[15,16], but to a different degree depending on the country[17,18]; the relationship may be more accurate in richer vis-à-vis poorer ones[19]. Thus, the relationship between ALN data and socioeconomic conditions may not be uniform across all countries; while we recognize this, we have to accept a consequent degree of uncertainty in the interpretation of results. According to our results, light pollution might be associated with a lifestyle leading to carcinogenesis, but we were not able to delve deeply into specific lifestyle factors. Another caveat, regarding the analysis performed for this study is that all the data which were used were cross-sectional; while the use of such data is commonly implemented, particularly in the social sciences, experts argue that there are limits to the representability of such an approach.
Our findings imply that intense ALN is indeed associated to financial measures such as GDP but it is the latter, and not ALN, which may create conditions that are detrimental to health and a potential risk factor for TC. It is possible that light pollution is associated with a lifestyle that leads to carcinogenesis. Furthermore, higher GDP and HEP implies better access to diagnostic means, possible facilitation of TC diagnosis and better inclusion in cancer registries. Exploring the underlying mechanisms linking light pollution, socioeconomic status, and lifestyle factors to TC risk is crucial for a more comprehensive understanding of these associations. Physicians should be aware of the potential impact of lifestyle, including exposure to ALN, on cancer risk. Further research seems imperative to elucidate the intricate relationship between ALN, lifestyle factors, and TC. Future investigations should delve into specific aspects of lifestyle, such as sleep hygiene and circadian rhythm disruptions, to identify modifiable risk factors. The broader implications for public health should not be overlooked: public health initiatives aimed at reducing light pollution, promoting healthy sleep habits, and raising awareness about the potential impacts of ALN on health may contribute to overall cancer prevention strategies.
The increasing incidence of thyroid cancer (TC) globally has sparked interest in identifying potential environmental factors contributing to this rise. While prior research has explored various risk factors, the association between artificial light at night (ALN) and TC remains an underexplored area. Present status: Current data indicate a notable increase in TC cases, along with a rise in exposure to ALN. Significance of the Study: Our findings imply that intense ALN is indeed associated to financial measures such as gross domestic product (GDP), but it is the latter, and not ALN, which may create conditions that are detrimental to health and a potential risk factor for TC.
The study is motivated by the need to comprehensively investigate the impact of ALN on TC at a global scale, recognizing the ubiquitous nature of light pollution in the modern world. Main topics and key problems: The primary focus is on evaluating the relationship between ALN exposure and TC incidence worldwide. The study delves into the prevalence of ALN using satellite data and examines whether there is a significant association with rates of TC. The research investigates the role of socioeconomic conditions, as indicated by GDP and health expenditure per person (HEP), in contributing to TC incidence. The study incorporates the quality of cancer registries (QCR) as a variable, recognizing the potential impact of data accuracy on the observed relationships. Significance for future research: By exploring the interplay between ALN exposure, socioeconomic factors, and TC, this study lays the groundwork for a more holistic understanding of the risk factors associated with TC. The study contributes to the broader field of environmental determinants of cancer, emphasizing the need for researchers to consider light pollution as a potential lifestyle-related factor impacting cancer risk. Acknowledging the limitations in exploring specific lifestyle factors in this study, future research can delve deeper into understanding the precise elements of lifestyle, such as sleep hygiene and circadian rhythm disruptions, which may contribute to TC risk.
Main objectives: To quantify and assess the prevalence of ALN exposure globally vis-à-vis TC epidemiology, using satellite data and cancer registries, respectively and controlling for financial conditions by country. Realized: Achieved through the analysis of ALN levels exceeding specific thresholds vis-à-vis TC epidemiology. Correlations among different financial indicators with both ALN exposure and TC incidence were noted, providing insights into potential socioeconomic influences. We integrated the QCR as a variable to account for potential variations in data accuracy. Future research: Significance: The study sets the stage for future research by highlighting the intricate relationship between ALN, socioeconomic factors, lifestyle, and TC risk. Future investigations can build upon these insights, delving deeper into specific lifestyle factors and refining preventive interventions.
Research Methods Used-Novelty: The study leveraged ALN data to explore its potential association with TC, integrating ALN exposure data with socioeconomic indicators such as GDP and HEP. Moreover, it considered the QCR as a variable that potentially leads to variations in data accuracy. Statistical Analyses: The data were analyzed with the Kolmogorov-Smirnoff, Kruskall Wallis and Kendall's Tau tests.
The global prevalence of ALN exposure was assessed, revealing that 67.3% of the world's population experiences ALN levels surpassing 87 μcd/m², and 34.6% surpassing 688 μcd/m². Globally, TC incidence, measured by the Adjusted Standardized Rate (ASR), was found to be 4.2 per 100000 population. Significant variations in ASR and ALN exposure percentages were noted across GDP and HEP quartiles, with higher values correlating to higher economic indicators. Differences in ASR were observed concerning the QCR, showing higher ASR in high-quality registries compared to lower quality ones. ASR by GDP and HEP quartiles demonstrated higher rates with increased economic indicators, and ALN exposure percentages also rose with higher economic quartiles. Direct associations between ASR and ALN exposure percentages were not significant. The study underscores the intricate relationship between ALN, economic indicators, and TC, emphasizing the role of socioeconomic conditions in cancer epidemiology. Problems that Remain to be Solved: The study found no direct link between ALN and TC, emphasizing the need for further research to understand their complex relationship. Consideration of QCR is crucial, urging refined assessments of data accuracy.
New theories proposed: While this study primarily focused on empirical investigations rather than proposing new theoretical frameworks, it introduced a nuanced perspective on the relationship between ALN, socioeconomic factors, and TC. The absence of a direct correlation between ALN and TC challenges existing theories that oversimplify the link between light pollution and cancer risk. The findings encourage a more complex understanding of environmental and socioeconomic influences on cancer incidence, prompting future theoretical developments in this field. New Methods Proposed: The study did not explicitly propose new research methods but demonstrated an innovative approach through the integration of diverse methodologies. Notably, the interdisciplinary analysis, global scale examination and incorporation of socioeconomic indicators represent methodological advancements. The study's emphasis on the QCR as a variable and its statistical analyses contribute to methodological robustness.
Future research should delve deeper into understanding the complex dynamics between ALN exposure and cancer risk. Investigating specific patterns of light exposure, considering variations in intensity, duration, and timing, may provide a more nuanced understanding of how ALN influences cancer incidence. Future research could also investigate the role of economic factors in shaping lifestyle choices, healthcare access, and environmental exposures, refining our understanding of the socioeconomic mechanisms influencing cancer incidence. Research focusing on the improvement of cancer registry quality assessment methods is crucial. Developing strategies to enhance data accuracy, especially in regions with lower-quality registries, will contribute to more reliable and comparable cancer incidence data. This could involve collaborations to standardize data collection practices globally.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medical laboratory technology
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Qin Y, China; Tzeng IS, Taiwan S-Editor: Qu XL L-Editor: A P-Editor: Guo X
| 1. | Falchi F, Cinzano P, Duriscoe D, Kyba CC, Elvidge CD, Baugh K, Portnov BA, Rybnikova NA, Furgoni R. The new world atlas of artificial night sky brightness. Sci Adv. 2016;2:e1600377. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 727] [Cited by in RCA: 610] [Article Influence: 67.8] [Reference Citation Analysis (0)] |
| 2. | Jones RR. Exposure to artificial light at night and risk of cancer: where do we go from here? Br J Cancer. 2021;124:1467-1468. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Zhang D, Jones RR, James P, Kitahara CM, Xiao Q. Associations between artificial light at night and risk for thyroid cancer: A large US cohort study. Cancer. 2021;127:1448-1458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 4. | Pizzato M, Li M, Vignat J, Laversanne M, Singh D, La Vecchia C, Vaccarella S. The epidemiological landscape of thyroid cancer worldwide: GLOBOCAN estimates for incidence and mortality rates in 2020. Lancet Diabetes Endocrinol. 2022;10:264-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 340] [Article Influence: 113.3] [Reference Citation Analysis (2)] |
| 5. | Olson E, Wintheiser G, Wolfe KM, Droessler J, Silberstein PT. Epidemiology of Thyroid Cancer: A Review of the National Cancer Database, 2000-2013. Cureus. 2019;11:e4127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 68] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 6. | Kim J, Gosnell JE, Roman SA. Geographic influences in the global rise of thyroid cancer. Nat Rev Endocrinol. 2020;16:17-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 292] [Article Influence: 58.4] [Reference Citation Analysis (1)] |
| 7. | Rossi ED, Pantanowitz L, Hornick JL. A worldwide journey of thyroid cancer incidence centred on tumour histology. Lancet Diabetes Endocrinol. 2021;9:193-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 70] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 8. | Soheylizad M, Khazaei S, Jenabi E, Delpisheh A, Veisani Y. The Relationship Between Human Development Index and Its Components with Thyroid Cancer Incidence and Mortality: Using the Decomposition Approach. Int J Endocrinol Metab. 2018;16:e65078. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Lee TJ, Kim S, Cho HJ, Lee JH. The incidence of thyroid cancer is affected by the characteristics of a healthcare system. J Korean Med Sci. 2012;27:1491-1498. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Ades F, Senterre C, de Azambuja E, Sullivan R, Popescu R, Parent F, Piccart M. Discrepancies in cancer incidence and mortality and its relationship to health expenditure in the 27 European Union member states. Ann Oncol. 2013;24:2897-2902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Sadeghi H, Rafei M, Bahrami M, Haghdoost A, Shabani Y. Attributable risk fraction of four lifestyle risk factors of thyroid cancer: a meta-analysis. J Public Health (Oxf). 2018;40:e91-e98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Huo S, Liu Y, Sun A, Zhang B. Environmental and social determinants of thyroid cancer: A spatial analysis based on the Geographical Detector. Front Endocrinol (Lausanne). 2022;13:1052606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 13. | Tordjman S, Chokron S, Delorme R, Charrier A, Bellissant E, Jaafari N, Fougerou C. Melatonin: Pharmacology, Functions and Therapeutic Benefits. Curr Neuropharmacol. 2017;15:434-443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 420] [Cited by in RCA: 506] [Article Influence: 63.3] [Reference Citation Analysis (0)] |
| 14. | Howard J. Minimum Latency and Types or Categories of Cancer. Centers for Disease Control. 2015. Available from: https://www.cdc.gov/wtc/pdfs/policies/WTCHP-Minimum-Cancer-Latency-PP-01062015-508.pdf. |
| 15. | Gibson J, Susan O, Boe-Gibson G. Night lights in economics: Sources and uses, LICOS Discussion Paper, No. 419. LICOS Centre for Institutions and Economic Performance. 2020. Available from: https://www.econstor.eu/bitstream/10419/230506/1/1688648216.pdf. |
| 16. | Gibson J, Olivia S, Boe-Gibson G, Li C. Which night lights data should we use in economics, and where? J Dev Econ. 2021;149:102602. [DOI] [Full Text] |
| 18. | Zumbrun J. Nighttime Light Can Illuminate Fudged Data. Wall Street Journal 2023; January 21-22: A2Available online as Shining a Light (Literally) on How Much Dictators Manipulate Their Economic Stats. Available from: https://www.wsj.com/articles/shining-a-light-literally-on-how-much-dictators-manipulate-their-economic-stats-11674183190. |
| 19. | Perez-Sindín XS, Chen THK, Prishchepov AV. Are night-time lights a good proxy of economic activity in rural areas in middle and low-income countries? Examining the empirical evidence from Colombia. Remote Sens Appl. 2021;24:100647. [DOI] [Full Text] |