Published online Sep 20, 2022. doi: 10.5662/wjm.v12.i5.414
Peer-review started: April 28, 2022
First decision: June 8, 2022
Revised: June 22, 2022
Accepted: August 21, 2022
Article in press: August 21, 2022
Published online: September 20, 2022
Processing time: 141 Days and 0.2 Hours
Despite its high prevalence, migraine remains underdiagnosed worldwide. A significant reason is the knowledge gap in physicians regarding diagnostic criteria, clinical features, and other clinical aspects of migraine.
To measure the knowledge deficit in physicians and medical students and to assess the prevalence of migraine in the same population.
An online questionnaire was developed and distributed among physicians and final year medical students on duty in various medical and surgical specialties of Allied and DHQ Hospitals, Faisalabad, between October 2018 and October 2019. Inclusion criteria were public practicing physicians who experience headaches, while those who never experienced headaches were excluded. Different questions assessed respondents on their knowledge of triggers, diagnosis, management, and prophylaxis of the migraine headache. They were asked to diagnose themselves using embedded ICHD-3 diagnostic criteria for different types of migraine. Graphs, tables, and figures were made using Microsoft Office 2016 and Microsoft Visio, and data analysis was done in R Studio 1.4.
We had 213 respondents and 175 fulfilled inclusion criteria, with 99 (52%), 58 (30%) and 12 (6.3%) belonging to specialties of medicine, surgery, and others, respectively. Both genders were symmetrically represented (88 male and 87 female). Fifty-two (24.4%) of our 213 respondents were diagnosed with migraine, with 26 (50%) being aware of it. Females had higher prevalence among study participants (n = 28, 32.2%) compared to males (n = 20, 22.7%, P = 0.19). A majority (62%) of subjects never consulted any doctor for their headache. Similarly, a majority (62%) either never heard or did not remember the diagnostic criteria of migraine. Around 38% falsely believed that having any type of aura is essential for diagnosing migraine. The consultation rate was 37% (n = 65), and migraineurs were significantly more likely to have consulted a doctor, and a neurologist in particular (P < 0.001). Consulters and migraineurs fared better in the knowledge of diagnostic aspects of the disease than their counterparts. There was no significant difference in other knowledge aspects between consulters versus non-consulters and migraineurs versus non-migraineurs.
Critical knowledge gaps exist between physicians and medical students, potentially contributing to misdiagnosis and mismanagement of migraine.
Core Tip: Despite its high prevalence, migraine remains underdiagnosed worldwide. A significant reason is the knowledge gap in physicians regarding diagnostic criteria, clinical features, and other clinical aspects of migraine. The primary objectives of this study were to measure the knowledge deficit in physicians and medical students and to assess the prevalence of migraine in the same population.
- Citation: Choudry H, Ata F, Naveed Alam MN, Ruqaiya R, Suheb MK, Ikram MQ, Chouhdry MM, Muaz M. Migraine in physicians and final year medical students: A cross-sectional insight into prevalence, self-awareness, and knowledge from Pakistan. World J Methodol 2022; 12(5): 414-427
- URL: https://www.wjgnet.com/2222-0682/full/v12/i5/414.htm
- DOI: https://dx.doi.org/10.5662/wjm.v12.i5.414
Headache is the top neurological complaint of patients presenting to general practitioners and neurologists. Migraine, one of the commonest headaches, is the sixth most prevalent disease globally and the second largest cause of disability, affecting more than 1 billion people[1,2]. Although not directly fatal, migraine results in considerable loss of work hours, productivity, and quality of life, culminating in a health burden and significant cost. In the United States alone, the annual expenditure on migraine exceeds 78 billion USD[3]. Despite being one of the top causes of morbidity, millions of migraine cases remain undiagnosed worldwide, leading to a preventable burden on the system[4]. This underdiagnosis has been attributed to lapses in physicians’ knowledge and lack of patient consultation, besides various other factors[5,6]. A recent study published in 2021 revealed several knowledge gaps in primary care providers concerning migraine diagnosis, with only 6.3% of physicians aware of migraine prevention guidelines[7]. Studies have elucidated a significantly higher prevalence of migraine in physicians, attributed to the better knowledge of diagnostic criteria and a variety of presentations of this headache[8]. Studies have also shown a specifically higher prevalence of migraine in headache specialists (53% compared to 19.3% in general practitioners), relating it to a better knowledge of the diagnostic criteria of migraine[9].
Prevention is the key management strategy for a significant subset of the population experiencing migraines, particularly those who cannot take abortive treatment. Preventive strategies, including drugs, indications of prophylaxis, and avoidance of triggers, constitute an essential piece of knowledge for managing physicians in this regard. Some of the triggers of migraines may not be commonly known by physicians, leading to incomplete medical advice and counseling. Studies have shown a significant difference in the discussion of migraine triggers (with the patients) among neurologists and other physicians (82% vs 51%)[10]. Only a physician adequately equipped with proper knowledge of prevention and triggers can manage migraine patients properly with a comprehensive education of prevention strategies. Lack of awareness of triggering factors among patients increases the frequency of otherwise avoidable exacerbations of migraine[11].
Pakistan’s estimated 1-year prevalence of migraine (22.5%) is considerably higher than the global 1-year prevalence of 15%[12,13]. Headache patients present in the outpatient settings of multiple specialties of our hospitals, including surgery. Junior doctors (including sub-interns, i.e., final year medical students) in Pakistan’s public hospitals serve as the first contact with health care for most patients with headaches. Therefore, the knowledge, attitudes and practices related to headache serve a pivotal role in the accurate and timely diagnosis and management of patients with headache syndromes, including migraine. Knowing the types of migraines and diagnostic criteria, and screening tools for some common types are essential for correct diagnosis. Transient neurological disturbances, usually in the form of visual or auditory sensory issues that precede migraine headaches, are known as auras. Aura is not experienced by 60%–80% of migraine patients, leading to a diagnosis of migraine without aura[14]. Worldwide, some studies recently have highlighted the gaps in physicians’ knowledge regarding the diagnosis of migraine[5,15,16]. We hypothesize similar gaps exist in our clinical settings in Pakistan; viewing aura as an integral part of the diagnosis of migraine being one such gap in knowledge. It is imperative for physicians to be aware of migraine without aura as it constitutes > 70% of migraine cases in Pakistan[17].
The aim of the study was to provide the first insight in the region into physicians’ knowledge regarding the diagnosis and management of migraine. The primary objective was to gauge the knowledge of physicians and final-year medical students regarding the triggers, diagnosis, management and prevention of migraine in Pakistan. Secondary objectives included determining the awareness of their own migraine among migraineurs, as well as estimating the point-prevalence of migraine among the physician population in Pakistan. Moreover, we also sought an assessment of the attitudes of our respondents towards medical consult-seeking for their headaches and self-medication (without a medical consult).
A web-based 30-question anonymous questionnaire was developed consisting of simple multiple choice as well as multiple choice–multiple response questions.
The questionnaire was distributed among physicians and final year medical students on duty in various medical and surgical specialties of Allied and DHQ Hospitals, the affiliated hospitals of Faisalabad Medical University. Participants were required to fill in the questionnaire in the presence of a team member to avoid misinterpretation of any question.
Inclusion criteria were physicians and final year medical students who experienced headaches. Private practitioners and non-practicing physicians were excluded. The data were collected between October 15, 2018 and October 15, 2019.
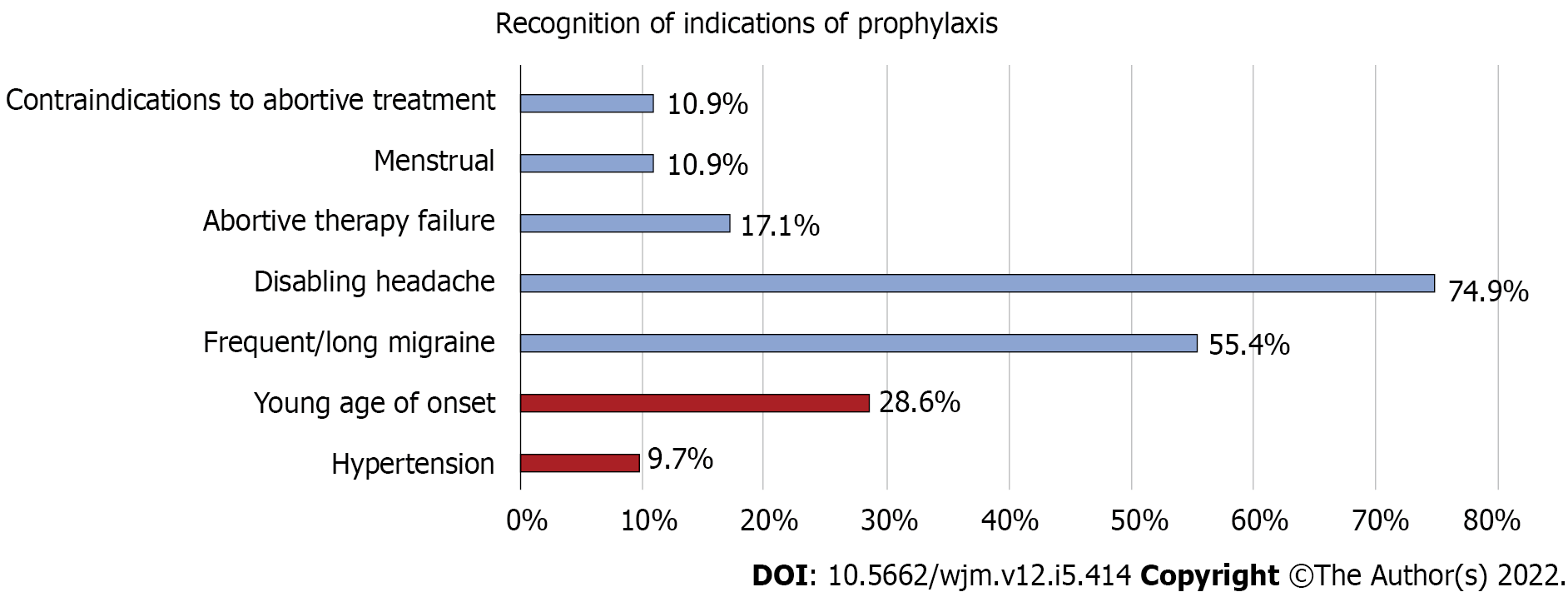
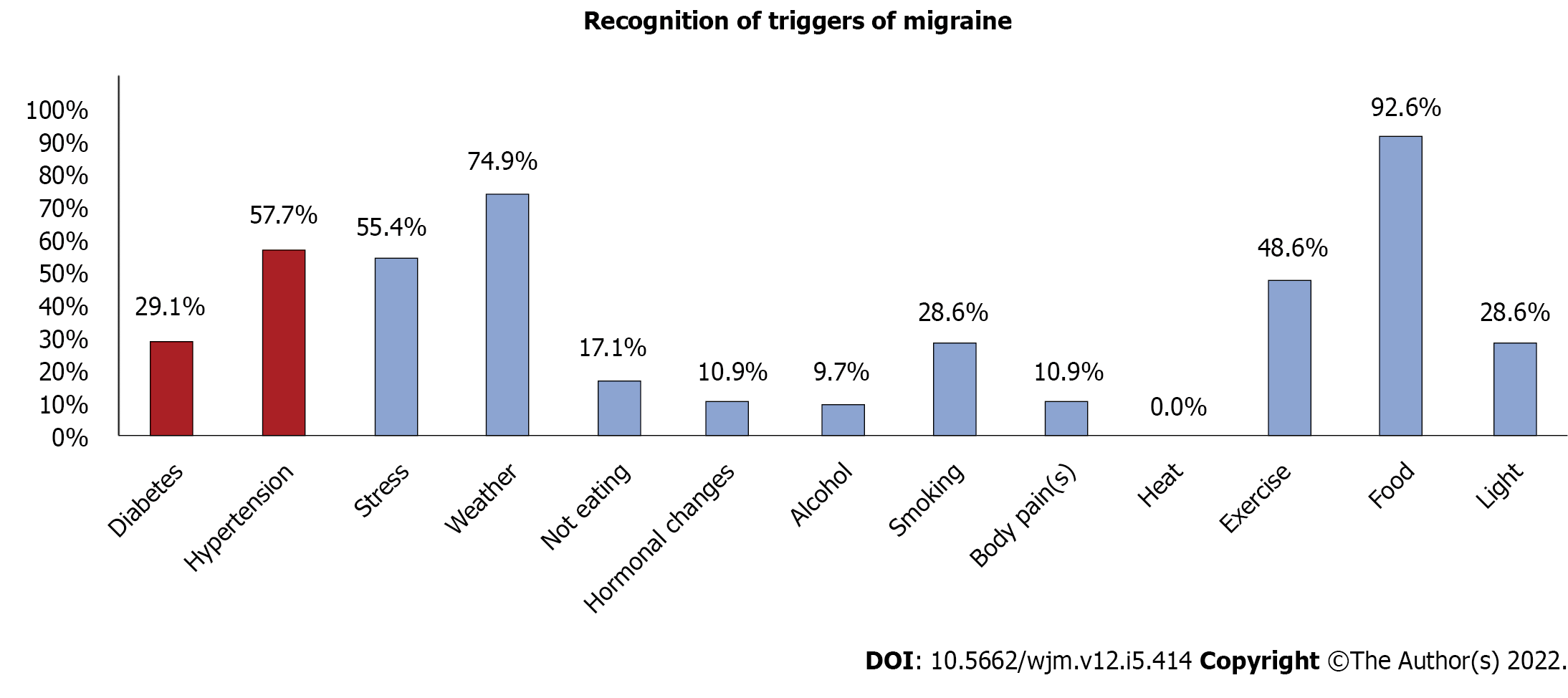
Respondents were asked if they thought they had a migraine and were then assessed on their knowledge of the definition, triggers and prophylaxis of the migraine, utilizing various subjective and objective questions. The triggers of migraine and the list of indications of prophylaxis of migraine were adopted from Kelman et al[19] and American Headache Society Consensus statement, respectively[18,19]. They were questioned about their knowledge of diagnostic criteria, prophylactic therapy and migraine triggers. They were also asked to choose appropriate answers from a list of available triggers of migraine and indications and duration for prophylaxis. Distractors were introduced in the triggers and indications of prophylaxis checklists to assess better for recognition (Figures 1 and 2). Migraineurs were further asked questions about their triggers, abortive and prophylactic therapy use and efficacy, medical consultation seeking, and over-the-counter (OTC) drug use. For diagnosis, ICHD-3 diagnostic criteria of migraine with aura, migraine without aura, and chronic migraine were embedded in the questionnaire. Respondents were asked to self-diagnose by matching their symptoms to these criteria within the questionnaire. Migraine cases (migraineurs) were the respondents who chose any type of migraine after going through all the diagnostic criteria. Self-awareness of migraine was defined as migraineurs who thought they had a migraine, while cases who answered “no” or “not sure” when asked if they had migraine were termed unaware. Sample size and sampling: a migraine prevalence of 30% in physicians was assumed (greater than the general population migraine prevalence of 22.5% in Pakistan) and sample size for a prevalence study was calculated for an estimated physician population of 100000 with a confidence interval level and precision of 95% and 6%, respectively. Source Forge’s free online sample size calculator was used (sampsize.sourceforge.net). The sample size determined was 186 for the prevalence study.
Reliability testing of migraine awareness was performed with the correlation coefficient (κ) to assess agreement between those who thought they had a migraine (self-aware) and confirmed cases of migraine. The sensitivity and specificity of the self-awareness of migraine were calculated by comparing it with the final diagnosis. The prevalence of migraine was calculated among all the respondents, including the excluded ones, to assess the actual prevalence of the disease in the physician and medical student population. Data analysis was run between groups using R version 1.4.1106, with an additional package of epitools. Chi-square, Mann–Whitney and Fisher’s exact tests were applied wherever applicable after tests of the normalcy of distribution (Shapiro–Wilk). Graphs, tables and figures were made using Microsoft Office 2016 and Microsoft Visio. This study was reported in accordance with The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines[20].
We distributed the questionnaire to a total of 275 subjects and managed to get a response from 213 of them, setting our response rate at 77.5%. One hundred and ninety participants fulfilled the inclusion criteria. After the application of exclusion criteria, we were left with 175 participants. Among them, 39 were medical students, and the rest of them were physicians. Males and females were symmetrically represented, with 88 males and 87 females. The average age was 25.7 ± 4.1 years. Most of our subjects (56%, n = 98) belonged to the specialty of medicine and allied, 30% (n = 51) to surgery and allied, and 5% (n = 9) to others (including pathology, radiology, etc.). A majority (62.3%, n = 109) of our respondents never consulted anyone for the headaches. The basic characteristics and demographic data of participants are summarized in Table 1.
| Characteristics | Results (N = 175), n (%) |
| Gender | Females: 88 (50.3) |
| Males: 87 (49.7) | |
| Age (yr) | Mean: 25.7 ± 4.1 |
| Grade | Medical student: 39 (22.3) |
| House officers: 74 (42.3) | |
| Non-trainee medical officers: 17 (9.7) | |
| Trainee medical officer: 38 (21.7) | |
| Senior registrar: 4 (2.3) | |
| Assist professor: 2 (1.1) | |
| Professor: 1 (0.6) | |
| Specialty of doctors | Medicine & allied: 98 (56) |
| Surgery & allied: 51 (29.1) | |
| Others: 9 (5.1) | |
| Not answered: 17 (9.7) | |
| Do you have migraine? | Yes: 22 (12.6) |
| No: 109 (62.3) | |
| Maybe: 44 (25.1) | |
| Confirmed migraine after reading the ICHD-3 criteria of all 3 types of migraine | Migraine without aura: 36 (20.6) |
| Migraine with aura: 9 (5.1) | |
| Chronic migraine: 3 (1.7) | |
| No migraine: 127 (72.6) | |
| Consulted any physician | GP: 19 (10.8) |
| Medical specialist: 22 (12.6) | |
| Neurologist: 10 (5.7) | |
| Ophthalmologist: 19 (10.8) | |
| Other: 9 (5.1) | |
| No consultation: 110 (62.8) | |
| Physician able to diagnose migraine | Yes: 45 (25.7) |
| No: 9 (5.1) | |
| Maybe: 9 (5.1) | |
| Never consulted: 112 (64) | |
| Knowledge of diagnostic criteria of migraine | Heard and remember it: 66 (37.7) |
| Heard about it but don't remember: 85 (48.6) | |
| Never heard about it: 24 (13.7) | |
| Knowledge of prophylaxis of migraine | I know its indications: 59 (33.7) |
| I knew its indications but don't remember: 70 (40) | |
| Know only that it exists: 26 (14.8) | |
| Don't know about it at all: 20 (11.4) | |
| Aura is essential for migraine? | Yes: 66 (37.7) |
| No: 83 (46.8) | |
| Not sure: 26 (14.7) | |
| Duration of standard prophylactic therapy of migraine? | Do not know: 100 (57.1) |
| 1 mo: 10 (5.7) | |
| 3 mo: 27 (15.4) | |
| 6 mo1: 24 (13.7) | |
| 12 mo: 14 (8) | |
| Monthly headache rate for prophylaxis | ≥ 2 per mo: 64 (36.6) |
| ≥ 3 per mo: 52 (29.7) | |
| ≥ 4 per mo1: 43 (24.6) | |
| ≥ 5 per mo: 15 (8.6) | |
| Not available: 1 (0.6) | |
| Used abortive (migraine patients only) | Yes: 12 (25) |
| No: 34 (70.8) | |
| Maybe: 2 (4.2) | |
| Used prophylactic therapy (migraine patients only) | Yes: 9 (18.7) |
| No: 38 (79.2) | |
| Not sure: 1 (2.1) |
Forty-eight (27.4%) of our 175 respondents were diagnosed with migraine using the questionnaire-embedded, self-diagnosis algorithm. This made the total prevalence of migraine in our sample of physicians and medical students 24.4%. Females, as expected, had higher prevalence (n = 28, 32.2%) compared to males (n = 20, 22.7%) among the final sample.
Only 21 (43.8%) of our 48 migraineurs were fully aware of their disease before the application of the embedded criteria, while eight (16.7%) and 19 (39.6%) were completely unaware and not sure, respectively. Similarly, out of 127 non-migraineurs, 126 correctly thought they did not have a migraine. This made the sensitivity and specificity of this self-awareness 43.8% and 99.2%, respectively. The correlation coefficient Cohen’s between self-awareness and migraine diagnosis was 0.52, showing a moderate level of association. The physicians’ diagnosis of migraine had similar sensitivity (37.5%), specificity (97.6%), and correlation coefficient values (0.43).
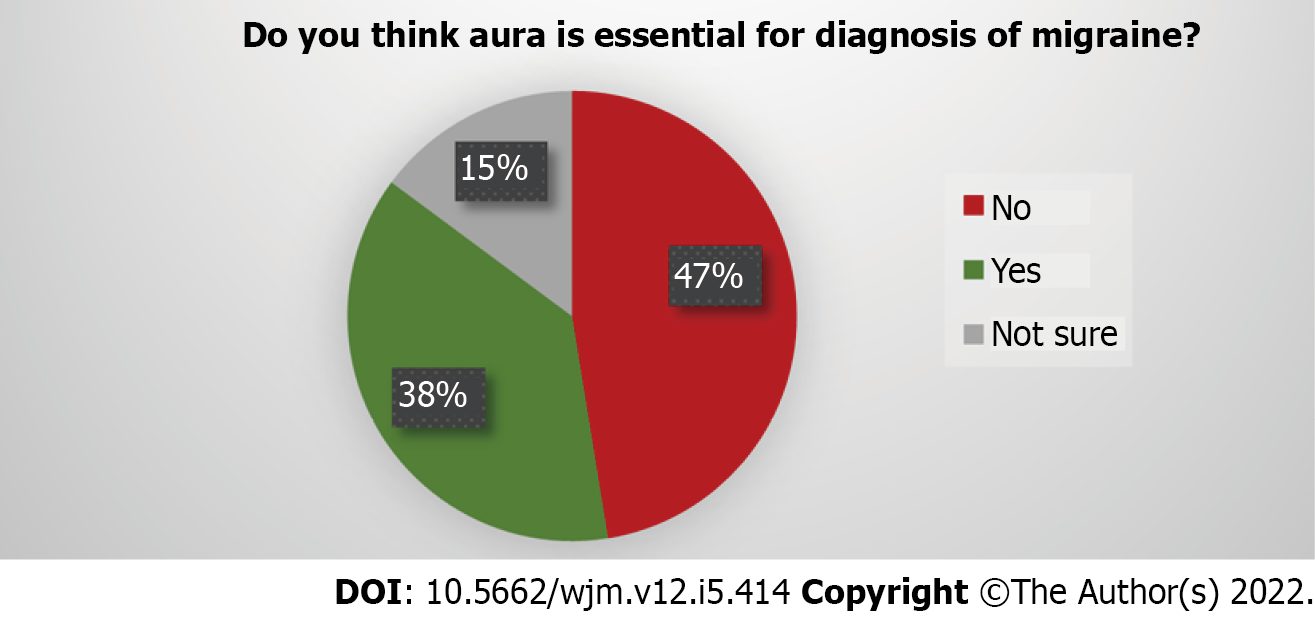
A major proportion of participants (36.7%) erroneously believed that having any type of aura is essential for diagnosing migraine (Figure 3). Almost half of the respondents (n = 85, 48.6%) said they did not remember the diagnostic criteria of migraine, while 13% had never heard about the criteria at all. 11.4% of respondents did not know that prophylactic therapy even existed, while only 33.7% said they remember prophylaxis indications. Only 13.7% (n = 24) could correctly identify the correct duration of prophylaxis while 57.1% (n = 100) of subjects did not know, 21.1% (n = 37) underestimated, and 8% (n = 14) overestimated the duration of prophylactic therapy of migraine. Respondents were able to recognize, on average, just 1.3 of 5 real indications and 3.5 of 11 real triggers. Stress was by far the most commonly recognized trigger, recognized by 92.6% of respondents.
Only 60.6% (n = 66) respondents had sought consult. In general, consultation seekers had better knowledge of diagnostic criteria and prophylactic therapy in the subjective questions. The difference almost reached significance in the knowledge about prophylactic therapy (Table 2), where 57.8% of consulters said they remembered the indications of prophylaxis compared with just 28% of non-consulters (OR: 1.84, P = 0.05). Similarly, only 40.4% of those who chose not to consult correctly believed that aura is essential for a migraine diagnosis compared with a majority (59.1%) of consultation seekers (OR: 0.47, P = 0.02). Paradoxically, non-consulters were more likely to correctly identify the monthly headache rate cut-off for initiation of prophylaxis (30.3%) versus consulters (15.1%), and the difference was significant (P = 0.02). However, upon further analysis, it was revealed that consulters were more likely than non-consulters to underestimate the monthly headache rate threshold for starting the prophylaxis, with a mean monthly rate chosen by this group to be 2.85 versus 3.18 by the non-consulters (P = 0.03). There was no significant difference in recognizing triggers and indications of prophylaxis between both groups (Table 2). Additionally, headache frequency in both groups was also similar.
| Consultation seeking | Migraine | |||||
| Non-consulters (n = 109) | Consulters (n = 66) | P | Migraineurs (n = 48) | Non-migraineurs (n = 127) | P | |
| Gender | Females: 54 (49.5%); Males: 55 (50.5%) | Females: 34 (51.5%); Males: 32 (48.5%) | 0.8 | Females: 28 (58.3%); Males: 20 (41.7%) | Females: 60 (47.2%); Males: 67 (52.7%) | 0.19 |
| Knowledge of diagnostic criteria | Remember: 37 (33.9%); Don’t remember:72 (66.1%) | Remember: 29 (43.9%); Don’t remember: 37 (56.1%) | 0.24 | Remember: 25 (52.1%); Don’t remember: 23 (47.9%) | Remember: 41 (32.3%); Don’t remember: 86 (67.7%) | 0.016; OR: 2.26 (95% CI: 1.1-4.5) |
| Know prophylaxis indications | Yes: 31 (28.4%); No:78 (71.6%) | Yes: 38 (34.9%); No: 28 (42.4%) | 0.05 | Yes: 21 (43.7%); No: 27 (56.2%) | Yes: 38 (29.9%); No: 89 (70.1%) | 0.08 |
| Aura essential for diagnosis? | Yes: 65 (59.6%); No or not sure: 44(40.4%)1 | Yes: 27 (40.9%); No or not sure: 39 (51.1%)1 | 0.016; OR: 0.47 (95%CI: 0.25-0.87) | Yes: 22 (45.8%); No or not sure: 26 (54.2%) | Yes: 70 (55.1%); No or not Sure: 57 (44.9%) | 0.27 |
| Consulted | Neurologist: 10 (15.2%); Other doctor(s): 56 (84.8%); None: 0 (0%) | Neurologist:8 (16.7%); Other doctors:21 (43.7%); None: 19 (39.6%) | Neurologist: 2 (1.6%); Other doctors: 35 (27.6%); None: 90 (70.9%) | < 0.001 | ||
| Monthly attack cutoff for prophylaxis2 | Correctly Identified: 33 (30.3%); Could not Identify: 75 (68.8%) | Correctly Identified: 10 (15.1%); Could not Identify: 56 (84.9%) | 0.02 | Correctly Identified: 16; Could not Identify: 32 | Correctly Identified: 27 (21.4%); Could not Identify: 99 (78.6%) | 0.11 |
| Know correct duration of prophylaxis?3 | Yes: 28 (25.7%); No: 81 (74.3%) | Yes :20 (30.3%); No: 46 (69.7%) | 0.5 | Yes: 13 (27%); No: 35 (73%) | Yes: 35 (27.5%); No: 92 (72.5%) | 0.94 |
| Frequency of headache attacks (per month) | None: 31 (28.4%); ≤ 1: 39(35.8%); 2: 17 (15.6%); 3: 6 (5.5%); ≥ 4: 16 (14.7%) | None: 13 (19.7%); ≤ 1: 22 (33.3%); 2: 13 (19.7%); 3: 8 (12.1%); ≥ 4: 10 (15.1%) | 0.4 | None: 4 (8.3%); ≤ 1: 16 (33.3%); 2: 9 (18.7%); 3: 6 (12.5%); ≥ 4: 13 (27.1%) | None: 40 (31.5%); ≤ 1: 45 (35.4%); 2: 21 (15.7%); 3: 8 (6.3%); ≥ 4: 13 (2.4%)1 | < 0.01 |
| Total triggers recognized | Median: 4, IQR: 5 | Median: 3, IQR: 4 | 0.29 | Median: 3.5, IQR: 3 | Median: 4, IQR: 5 | 0.297 |
| Total indications recognized | Median: 2, IQR: 1 | Median: 1, IQR: 1 | 0.21 | Median: 1, IQR: 1 | Median: 1, IQR: 1 | 0.22 |
| Distractor(s) recognized as triggers | Yes: 47 (43.1%); No: 62 (56.9%) | Yes: 29 (43.9%); No: 37 (56.1%) | 0.91 | Yes: 22 (45.8%); No: 26 (54.2%) | Yes: 54 (42.5%); No: 73 (57.5%) | 0.69 |
| Distractor(s) recognized as Indications | Yes: 37 (33.9%); No: 71 (65.1%) | Yes: 17 (25.7%); No: 49 (74.2%) | 0.23 | Yes: 16 (33.3%); No: 32 (66.7%) | Yes: 38 (22.1%); No: 88 (87.9%) | 0.68 |
| Migraineurs | Migraineurs: 19 (17.4%); Non-migraineurs: 90 (82.5%)1 | Migraineurs: 29 (43.9%); Non-migraineurs: 37 (56.1%)1 | < 0.001; OR: 3.7 (95%CI: 1.8-7.5) | |||
Migraineurs were much more likely to have visited a doctor than non-migraineurs, and the difference was significant (OR: 3.7, P < 0.001). A neurologist consultation was even more significantly associated with a diagnosis of migraine (OR: 17.4, P < 0.001). Females were more likely (31.8%) to have migraines than were males (22.9%), although the difference was not significant. Similarly, there was no significant difference between knowledge of duration or prophylaxis indications and triggers between migraineur and non-migraineur populations.
Migraineurs were more likely than non-migraineurs to remember the diagnostic criteria (52% vs 32%, OR: 2.26, P = 0.016). They were also more likely to know prophylaxis indications (43% vs 29.9%), but the difference here was just above significance (P = 0.08). Headache attacks per month were significantly higher in migraineurs (median 2 ± 4) than non-migraineurs (0.5 ± 2 IQR), and the difference was significant (P < 0.01).
Awareness of one’s own disease was more common in females (53%) than in males (40%), but the difference was not significant. Migraine-aware respondents were significantly more likely to have visited a physician (81%) than were unaware migraineurs (44%, OR: 5.0, P = 0.01). Neurologist consultation, in particular, was more common in migraine aware (6/21) versus unaware (2/27, OR: 9.6, P = 0.024) participants. All knowledge questions related to diagnosis and prophylaxis had similar results in both groups (Table 3).
| Migraine awareness | |||
| Migraine aware (n = 21) | Not aware (n = 27) | P | |
| Gender | Females: 13 (61.9%); Males: 8 (38.1%) | Females: 15 (55.5%); Males: 12 (45.5%) | 0.65 |
| Diagnostic criteria | Remember: 12 (57.1%); don’t remember: 9 (42.9%) | Remember: 13 (48%); don’t remember: 14 (52%) | 0.53 |
| Know prophylaxis indications | Know indications: 11 (52.4%); do not know about either prophylaxis or its indications: 10 (47.6%) | Know indications: 10 (37%); do not know about either prophylaxis or its indications: 17 (63%) | 0.44 |
| Aura essential for diagnosis? | No: 13 (61.9%); yes or not sure: 8 | No: 13 (48.1%); yes or not sure: 14 (51.9%) | 0.34 |
| Consulted | Neurologist: 6 (28.6%); Any other physician: 11 (52.4%); Didn't consult: 4 (19%)1 | Neurologist: 2 (7.4%); Any other physician: 10 (37%); Didn’t consult: 151 (55.6%) | 0.02; OR: 9.6 (95%CI: 1.5-96) |
| Monthly attack cutoff for prophylaxis | Correctly identified: 5 (23.8%); Couldn't identify: 16 (76.2%) | Correctly identified: 11 (40.7%); Couldn't identify: 16 (59.2%) | 0.22 |
| Know duration of prophylaxis | Correctly identified: 6 (28.5%); Couldn't identify:15 (71.4%) | Correctly identified: =7 (33.3%); Couldn’t identify: 20 (66.7%) | 0.83 |
| Respondent’s frequency of attacks (per month) | None: 1 (4.8%); ≤ 1: 8 (38.1%); 2: 2 (9.5%); 3: 3 (14.3%); ≥ 4: 7 (33.3%) | None: 3 (11.1%); ≤ 1: 8 (29.6%); 2: 7 (25.9%); 3: 3 (11.1%); ≥ 4: 6 (22.2%) | 0.5 |
| Average no of triggers recognized | Median: 3, IQR: 3 | Median: 4, IQR: 3 | 0.32 |
| Average no of indications recognized | Median: 1, IQR: 1 | Median: 2, IQR: 1 | 0.17 |
Our study presents the first extensive data on awareness and knowledge of migraine among physicians in Pakistan, with a point-prevalence of migraine at 24.4%. A similar prevalence has been reported in neighboring countries in the region[21,22]. Herekar et al[12] have previously reported a 1-year prevalence of migraine in the general population of Pakistan to be 22.5%. The differences in prevalence have been attributed to methodological variations and changes in cultural attitudes towards disease that lead to underdiagnosis in certain subsets of the population[23,24].
Lack of awareness and knowledge of migraine and its management among physicians causes a striking yet avoidable burden on its demographics. One of the critical reasons for underdiagnoses of migraine is unfamiliarity with the diagnostic criteria and the reluctance to use diagnostic tools among physicians[5,25]. Kristoffersen et al[16], who surveyed knowledge of Neurology residents in Norway regarding migraine, reported lapses in the knowledge of neurology residents below the bare minimum. Only half of the neurology residents had used the diagnostic criteria regularly, undoubtedly leading to inadequate familiarity with migraine presentations and subsequent underdiagnosis. Gültekin et al[5] reported that only 10% of primary care physicians in Turkey could give the complete diagnostic criteria of migraine. We report similar findings in our population, as 62% of participants in our study admitted not remembering the diagnostic criteria. When tested objectively, 38% believed in the myth that migraine could not be diagnosed without aura. This further indicates a fundamental unfamiliarity with types of migraine, migraine without aura in particular. The inadequate familiarity with not only the diagnostic criteria but the types of migraine as well can undeniably lead to an underdiagnosis and mismanagement of a plethora of cases.
The migraine triggers originated from self-reports by patients, but some have been experimentally verified[26]. Advice regarding triggers has varied through the years. Historically, it was argued that the best way to avoid headache was to avoid the triggers. Still, recent evidence suggests that the association of triggers with the headache is a learned process of the brain that subsequently attaches it to the headache. According to this theory, slow desensitization techniques rather than avoidance strategy is the way forward[27]. Nonetheless, knowledge of the trigger itself is vital for physicians if they counsel the patient appropriately for either strategy. The fact that an average physician in our study could not recognize even half of the triggers from the list points to an apparent deficiency in this knowledge. Moreover, perhaps even more worryingly, almost half of the participants chose the distractors (hypertension and diabetes) as triggers.
Menstrual migraine is associated with particularly significant morbidity due to the longer duration, increased severity, and periodicity, and also because of its refractoriness to abortive treatment[28]. The disability associated with it deserves a special mention because it, arguably, is the most common migraine trigger, with 70% of female migraineurs reporting this trigger[28]. It is also one of the most common disabling conditions presented in gynecological practices[29] but 42% of our respondents did not recognize it as a trigger. In comparison, an overwhelming majority (90%) did not know that menstrual migraine can itself be an indication for initiation of prophylaxis, which reveals a vital missing piece in physicians’ knowledge on the subject.
Studies on migraine have consistently demonstrated the role of preventive therapy in reducing disease burden[30]. Preventive therapy is central in managing migraineurs with severe and frequent attacks as the overutilization of abortive therapy may frequently lead to medication-overuse headaches or resistant migraine[31]. Preventive therapy is also required in some cases to augment responsiveness to abortive therapy as it reduces the frequency and duration of the migraine attacks and the severity[13]. Silberstein and colleagues demonstrated that preventive therapy (when indicated) combined with abortive was much more effective in reducing the migraine load than abortive therapy alone[31]. Moreover, management of chronic migraine requires an approach involving a combination of abortive, preventive, and behavioral therapy. In our sample, chronic migraine (frequent attacks) as an indication of prophylaxis was recognized by 50% of respondents, which fares relatively better than recognition of other indications but is still inadequate. On the contrary, only 33% of physicians and medical students thought they remembered the indications of prophylaxis. When tested from a list of indications, a physician could identify only about one indication out of five. These results reveal another vital knowledge gap that needs priority focus.
Physicians, in general, underestimate the role of preventive therapy[31-34]. The American Migraine Communication study highlighted physicians under-rating the disability caused by migraine and thus the need for prophylactic therapy[35]. In contrast, there is some evidence that neurologists, compared with other physicians, tend to emphasize the role of prophylaxis[36]. Physicians’ unfamiliarity with preventive therapy means an inability to manage chronic migraine cases properly. Preventive therapy use among physicians in our sample (18%) was similar to the prevalence reported elsewhere in the literature[31,37]. The fact that more than two thirds of physicians in our sample did not remember the indications of prophylaxis when asked subjectively is particularly troubling for a large subset of special cases. These comprise but are not limited to chronic migraine, menstrual-related, resistant migraine, and other more severe forms of migraine, which are contingent upon preventive therapy and are perhaps responsible for several mishandled cases. Additionally, we found no meaningful differences between consulters and non-consulters for recognition of prophylaxis indications. Our inference is that the under-emphasis on preventive therapy in the form of avoidance of triggers or drug therapy is so pervasive that even after consulting a physician for the headache, respondents did not gain any meaningful knowledge of these aspects of the migraine.
Weber et al[38] reported that primary care physicians suffering from migraine described receiving more migraine patients in their practice than their healthy colleagues. Their patients were more likely to have a better quality of life. This is perhaps related to the sensitivity of such physicians towards migraineurs. A similar inference can be made from our results, as migraineurs were more likely to state that they knew the diagnostic criteria. However, the difference was not significant when asked the question regarding diagnosis objectively, i.e., the question related to the aura. The improved knowledge of the disease’s diagnosis and management in physicians with migraine (Table 2) puts them in a better position to understand and help the patients. Migraineurs in our study were also more likely to have visited a doctor (61.4% vs 29.1%). The association was strongest with a neurologist’s consultation (OR: 17.4, P < 0.001). This potentially represents the role of a consultation, especially with a neurologist, in diagnosing migraine[39]. The subjective feeling of knowledge related to diagnostic criteria as well as prophylactic therapy was also significantly better in consultation seekers (Table 2). We think this is a result of discussion about the disease with their consulting physicians or more intrigue and reflection about the disease resulting from the consultation. The consulting process, the resultant introspection, and perhaps reading about their condition helped physicians improve their knowledge. This is also reflective of the power and efficacy of a medical consultation[39]. The contradictory results on the monthly headache rate threshold of preventive therapy can be logically explained with a further breakdown of data, as consulters favored the prophylaxis more and underestimated the threshold for initiation of prophylaxis, constituting a better trend overall.
Radtke et al[25] reported 70% awareness of migraine in their sample in 2012, with a coefficient of agreement value of 0.46 between ICHD-II criteria and awareness. At 44%, migraine in our sample was lower ( = 0.52). The sensitivity of physicians’ diagnosis among the sample collected by Radtke et al[25] was also better at 63%. We did not specify the temporal order of events in our question, i.e., whether they knew about their migraine before consulting a doctor or suspected one after their visit. Hence, this self-awareness of migraine is not mutually exclusive to the consulting physician’s diagnosis of migraine in our cases. However, our data hint toward the role of physicians’ consultation in producing this self-awareness. Although consulting with physicians could not contribute to better knowledge of the subjects, it still helped diagnose the disease in many cases. The precision of diagnosis was better when consultations came from neurologists (Table 3). However, the number in our sample was too small, and more studies are needed for a more generalizable inference. Our study thus reinforces the earlier findings that the advice to seek consultation for a headache instead of OTC medication use is essential and needs to be practiced by our physicians[39].
The ever-increasing global burden of non-communicable diseases concerning morbidity and the fact that migraine is jumping the ladder of the most prevalent diseases exponentially is alarming[40]. Every effort has to be made for an accurate and timely diagnosis of migraine. Fortunately, with the advent of new data on drug therapy in migraine, this era is also witnessing a remarkable change in its mana
Our study had some limitations grounded in the study design used. Firstly, the subjective questions on diagnostic criteria and prophylactic treatment were subject to social desirability bias as most respondents were not open to accepting their knowledge deficit. Secondly, we did not use any migraine diagnosis registry due to lack of the aforementioned, but our data collection team ensured that respondents understood the diagnostic criteria during collection. Thirdly, excluding the cases that did not experience headaches may have potentially excluded a specific subset of doctors whose knowledge was not tested. This, albeit small, was a potential source of sampling bias in our study. Fourthly, although almost all the questionnaires were filled in the presence of one of the study team members and we tried to keep the questionnaire as short as possible, there was still a possibility that some of the participants might not have read the questions and criteria thoroughly; an inherent possibility with the questionnaire-based studies. Despite these limitations, we believe the study was largely free from any systematic biases.
Despite its high prevalence and high associated morbidity, migraine diagnosis and management knowledge remain below the minimum functionally required among physicians in Pakistan. Steps need to be taken to bridge the knowledge gap among doctors to address underdiagnosis and mismanagement of the disease.
Despite its high prevalence, migraine remains underdiagnosed worldwide. A significant reason is the knowledge gap in physicians regarding diagnostic criteria, clinical features, and other clinical aspects of migraine.
This research was conducted to see whether migraine follows the same trends of underdiagnosis in Physicians of Pakistan as globally.
We aimed to measure the knowledge deficit in physicians and medical students and to assess the prevalence of migraine in the same population.
An online questionnaire was developed and distributed among physicians and final-year medical students on duty in various medical and surgical specialties of Allied and DHQ Hospitals, Faisalabad, between October 2018 and October 2019. Inclusion criteria were public practicing physicians who experience headaches, while those who never experienced headaches were excluded. Different questions assessed respondents on their knowledge of triggers, diagnosis, management, and pro
We had 213 respondents and 175 fulfilled inclusion criteria, with 99 (52%), 58 (30%) and 12 (6.3%) belonging to specialties of medicine, surgery, and others, respectively. Both genders were symmetrically represented (88 male and 87 female). Fifty-two (24.4%) of our 213 respondents were diagnosed with migraine, with 26 (50%) being aware of it. Females had higher prevalence among study participants (n = 28, 32.2%) compared to males (n = 20, 22.7%, P = 0.19). A majority (62%) of subjects never consulted any physician for their headache. Similarly, a majority (62%) either never heard or did not remember the diagnostic criteria of migraine, and 38% falsely believed that having any type of aura was essential for diagnosing migraine. The consultation rate was 37% (n = 65), and migraineurs were significantly more likely to have consulted a physician, a neurologist in particular (P < 0.001). Consulters and migraineurs fared better in the knowledge of diagnostic aspects of the disease than their counterparts. There was no significant difference in other knowledge aspects between consulters and non-consulters and migraineurs and non-migraineurs.
Critical knowledge gaps exist between physicians and medical students, potentially contributing to the misdiagnosis and mismanagement of migraine cases.
Migraine remains an underdiagnosed disease in the general population as well as among healthcare providers. Education, timely diagnosis, and management will help reduce its global burden.
We are grateful to all the participating medical students, residents and senior doctors for their time and input, without which this project would not have been accomplished. We also want to thank the Department of Neurology, Punjab Medical College Faisalabad, for providing constructive feedback on the project.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American college of physicians; American Society of Tropical Medicine and Hygiene, American College of Academic International Medicine.
Specialty type: Neurosciences
Country/Territory of origin: Pakistan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Hasabo EA, Sudan; Lu H, China S-Editor: Wu YXJ L-Editor: Kerr C P-Editor: Wu YXJ
| 1. | GBD 2016 Headache Collaborators. Global, regional, and national burden of migraine and tension-type headache, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17:954-976. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1276] [Cited by in RCA: 1174] [Article Influence: 167.7] [Reference Citation Analysis (0)] |
| 2. | GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1211-1259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5428] [Cited by in RCA: 5098] [Article Influence: 637.3] [Reference Citation Analysis (0)] |
| 3. | Gooch CL, Pracht E, Borenstein AR. The burden of neurological disease in the United States: A summary report and call to action. Ann Neurol. 2017;81:479-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 258] [Article Influence: 43.0] [Reference Citation Analysis (0)] |
| 4. | Miller S, Matharu MS. Migraine is underdiagnosed and undertreated. Practitioner. 2014;258:19-24, 2. [PubMed] |
| 5. | Gültekin M, Balci E, İsmaİLOĞULLARI S, Yetkin F, Baydemir R, Erdoğan F, Mİrza M, Özge A. Awareness of Migraine Among Primary Care Physicians in Turkey: A Regional Study. Noro Psikiyatr Ars. 2018;55:354-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Diamond S, Bigal ME, Silberstein S, Loder E, Reed M, Lipton RB. Patterns of diagnosis and acute and preventive treatment for migraine in the United States: results from the American Migraine Prevalence and Prevention study. Headache. 2007;47:355-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 139] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 7. | Verhaak AMS, Williamson A, Johnson A, Murphy A, Saidel M, Chua AL, Minen M, Grosberg BM. Migraine diagnosis and treatment: A knowledge and needs assessment of women's healthcare providers. Headache. 2021;61:69-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 8. | Xie W, Li R, He M, Cui F, Sun T, Xiong J, Zhao D, Na W, Liu R, Yu S. Prevalence and risk factors associated with headache amongst medical staff in South China. J Headache Pain. 2020;21:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 9. | Evers S, Brockmann N, Summ O, Husstedt IW, Frese A. Primary headache and migraine in headache specialists - does personal history of doctors matter? Cephalalgia. 2020;40:96-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Sheftell FD, Cady RK, Borchert LD, Spalding W, Hart CC. Optimizing the diagnosis and treatment of migraine. J Am Acad Nurse Pract. 2005;17:309-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Jain R, Ishar H, Chouksey D, Rathi P, Athale S, Sodani A. Awareness of triggers of headache in migraine patients -a study from a tertiary centre from central india. 2020:111-5.. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Herekar AA, Ahmad A, Uqaili UL, Ahmed B, Effendi J, Alvi SZ, Shahab MA, Javed U, Herekar AD, Khanani R, Steiner TJ. Primary headache disorders in the adult general population of Pakistan - a cross sectional nationwide prevalence survey. J Headache Pain. 2017;18:28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Ashina M. Migraine. N Engl J Med. 2020;383:1866-1876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 452] [Article Influence: 90.4] [Reference Citation Analysis (0)] |
| 14. | Eigenbrodt AK, Ashina H, Khan S, Diener HC, Mitsikostas DD, Sinclair AJ, Pozo-Rosich P, Martelletti P, Ducros A, Lantéri-Minet M, Braschinsky M, Del Rio MS, Daniel O, Özge A, Mammadbayli A, Arons M, Skorobogatykh K, Romanenko V, Terwindt GM, Paemeleire K, Sacco S, Reuter U, Lampl C, Schytz HW, Katsarava Z, Steiner TJ, Ashina M. Diagnosis and management of migraine in ten steps. Nat Rev Neurol. 2021;17:501-514. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 194] [Cited by in RCA: 283] [Article Influence: 70.8] [Reference Citation Analysis (0)] |
| 15. | Aljunaid MA, Jamal HH, Mubarak AA, Bardisi W. Levels and determinants of knowledge about chronic migraine diagnosis and management among primary health-care physicians in ministry of health, Jeddah 2019. J Family Med Prim Care. 2020;9:2324-2331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Kristoffersen ES, Faiz KW, Winsvold BS. Neurology residents' knowledge of the management of headache. Cephalalgia. 2019;39:1396-1406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Jat MI, Afridi MI, Kumar A, Lal C, Toufique F, Ram D. Frequency and pattern of common primary headache among depressed patients at tertiary care centre, Karachi. J Pak Med Assoc. 2017;67:1689-1692. [PubMed] |
| 18. | American Headache Society. The American Headache Society Position Statement On Integrating New Migraine Treatments Into Clinical Practice. Headache. 2019;59:1-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 241] [Article Influence: 34.4] [Reference Citation Analysis (0)] |
| 19. | Kelman L. The triggers or precipitants of the acute migraine attack. Cephalalgia. 2007;27:394-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 527] [Cited by in RCA: 567] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 20. | von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:e296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2924] [Cited by in RCA: 3457] [Article Influence: 192.1] [Reference Citation Analysis (0)] |
| 21. | Al-Hashel JY, Ahmed SF, Alroughani R. Prevalence of Primary Headache Disorders in Kuwait. Neuroepidemiology. 2017;48:138-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 22. | Rabiee B, Zeinoddini A, Kordi R, Yunesian M, Mohammadinejad P, Mansournia MA. The Epidemiology of Migraine Headache in General Population of Tehran, Iran. Neuroepidemiology. 2016;46:9-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Bokhari FA, Sami W, Shakoori TA, Ali SA, Qureshi GA. Clinical characteristics of 226 college-going female migraineurs in Lahore, Pakistan - putting ICHD-2 to the road test. Neuro Endocrinol Lett. 2008;29:965-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Murtaza M, Kisat M, Daniel H, Sonawalla AB. Classification and clinical features of headache disorders in Pakistan: a retrospective review of clinical data. PLoS One. 2009;4:e5827. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 25. | Radtke A, Neuhauser H. Low rate of self-awareness and medical recognition of migraine in Germany. Cephalalgia. 2012;32:1023-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Pavlovic JM, Buse DC, Sollars CM, Haut S, Lipton RB. Trigger factors and premonitory features of migraine attacks: summary of studies. Headache. 2014;54:1670-1679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 104] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 27. | Martin PR. Managing headache triggers: think 'coping' not 'avoidance'. Cephalalgia. 2010;30:634-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 28. | Vetvik KG, MacGregor EA. Menstrual migraine: a distinct disorder needing greater recognition. Lancet Neurol. 2021;20:304-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 75] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 29. | Burch RC, Loder S, Loder E, Smitherman TA. The prevalence and burden of migraine and severe headache in the United States: updated statistics from government health surveillance studies. Headache. 2015;55:21-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 359] [Article Influence: 35.9] [Reference Citation Analysis (0)] |
| 30. | D'Amico D, Solari A, Usai S, Santoro P, Bernardoni P, Frediani F, De Marco R, Massetto N, Bussone G; Progetto Cefalee Lombardia Group. Improvement in quality of life and activity limitations in migraine patients after prophylaxis. A prospective longitudinal multicentre study. Cephalalgia. 2006;26:691-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 31. | Silberstein SD. Preventive Migraine Treatment. Continuum (Minneap Minn). 2015;21:973-989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 116] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 32. | Hansen LC, Gaul C, Pogatzki-Zahn E, Baron R, Gierthmühlen J. Do doctors treat themselves differently than their patients? Cephalalgia. 2020;40:788-796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 33. | Roessler T, Zschocke J, Roehrig A, Friedrichs M, Friedel H, Katsarava Z. Administrative prevalence and incidence, characteristics and prescription patterns of patients with migraine in Germany: a retrospective claims data analysis. J Headache Pain. 2020;21:85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 34. | Minen M, Shome A, Halpern A, Tishler L, Brennan KC, Loder E, Lipton R, Silbersweig D. A migraine management training program for primary care providers: An overview of a survey and pilot study findings, lessons learned, and considerations for further research. Headache. 2016;56:725-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 35. | Lipton RB, Hahn SR, Cady RK, Brandes JL, Simons SE, Bain PA, Nelson MR. In-office discussions of migraine: results from the American Migraine Communication Study. J Gen Intern Med. 2008;23:1145-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 36. | Lipton RB, Bigal ME, Rush SR, Yenkosky JP, Liberman JN, Bartleson JD, Silberstein SD. Migraine practice patterns among neurologists. Neurology. 2004;62:1926-1931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 37. | Lipton RB, Bigal ME, Diamond M, Freitag F, Reed ML, Stewart WF; AMPP Advisory Group. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68:343-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1520] [Cited by in RCA: 1635] [Article Influence: 90.8] [Reference Citation Analysis (0)] |
| 38. | Weber M, Daurès JP, Fabre N, Druais PL, Dardenne J, Slama A, El Hasnaoui A. [Influence of general practitioners' personal knowledge on migraine in medical attitudes towards their patients suffering from migraine]. Rev Neurol (Paris). 2002;158:439-445. [PubMed] |
| 39. | Lantéri-Minet M. The role of general practitioners in migraine management. Cephalalgia. 2008;28 Suppl 2:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 40. | Benziger CP, Roth GA, Moran AE. The Global Burden of Disease Study and the Preventable Burden of NCD. Glob Heart. 2016;11:393-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 330] [Article Influence: 47.1] [Reference Citation Analysis (0)] |
| 41. | Mavridis T, Deligianni CI, Karagiorgis G, Daponte A, Breza M, Mitsikostas DD. Monoclonal Antibodies Targeting CGRP: From Clinical Studies to Real-World Evidence-What Do We Know So Far? Pharmaceuticals (Basel). 2021;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 42. | Sevivas H, Fresco P. Treatment of resistant chronic migraine with anti-CGRP monoclonal antibodies: a systematic review. Eur J Med Res. 2022;27:86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 43. | Zhu C, Guan J, Xiao H, Luo W, Tong R. Erenumab safety and efficacy in migraine: A systematic review and meta-analysis of randomized clinical trials. Medicine (Baltimore). 2019;98:e18483. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |