Published online Nov 6, 2014. doi: 10.5527/wjn.v3.i4.277
Revised: July 16, 2014
Accepted: September 17, 2014
Published online: November 6, 2014
Processing time: 153 Days and 18.3 Hours
The nutcracker phenomenon [left renal vein (LRV) entrapment syndrome] refers to compression of the LRV most commonly between abdominal aorta and superior mesenteric artery. Term of nutcracker syndrome (NCS) is used for patients with clinical symptoms associated with nutcracker anatomy. LRV entrapment divided into 2 types: anterior and posterior. Posterior and right-sided NCSs are rare conditions. The symptoms vary from asymptomatic hematuria to severe pelvic congestion. Symptoms include hematuria, orthostatic proteinuria, flank pain, abdominal pain, varicocele, dyspareunia, dysmenorrhea, fatigue and orthostatic intolerance. Existence of the clinical features constitutes a basis for the diagnosis. Several imaging methods such as Doppler ultrasonography, computed tomography angiography, magnetic resonance angiography and retrograde venography are used to diagnose NCS. The management of NCS depends upon the clinical presentation and the severity of the LRV hypertension. The treatment options are ranged from surveillance to nephrectomy. Treatment decision should be based on the severity of symptoms and their expected reversibility with regard to patient’s age and the stage of the syndrome.
Core tip: The nutcracker phenomenon [left renal vein (LRV) entrapment syndrome] refers to compression of the LRV most commonly between abdominal aorta and superior mesenteric artery. Term of nutcracker syndrome (NCS) is used for patients with clinical symptoms associated with nutcracker anatomy. The symptoms vary from asymptomatic hematuria to severe pelvic congestion. The management of NCS depends upon the clinical presentation and the severity of the LRV hypertension.
- Citation: Gulleroglu K, Gulleroglu B, Baskin E. Nutcracker syndrome. World J Nephrol 2014; 3(4): 277-281
- URL: https://www.wjgnet.com/2220-6124/full/v3/i4/277.htm
- DOI: https://dx.doi.org/10.5527/wjn.v3.i4.277
The nutcracker phenomenon [left renal vein (LRV) entrapment syndrome] refers to compression of the LRV most commonly between abdominal aorta and superior mesenteric artery. This phenomenon is characterized by impeded outflow from the LRV into the inferior vena cava (IVC) due to extrinsic compression.
The terms nutcracker phenomenon and nutcracker syndrome (NCS) are sometimes used as synonym in the literature. Nutcracker phenomenon descript anatomic findings suggestive of nutcracker are present without clinical symptoms. Term of NCS is used for patients with clinical symptoms associated with nutcracker anatomy.
Diagnosis of NCS could be difficult for some reasons. It was thought to be a rare condition. Also in the absence of clinical features it was necessitate a high suspicion. A noninvasive imaging must be followed by an invasive imaging for confirmation of the diagnosis.
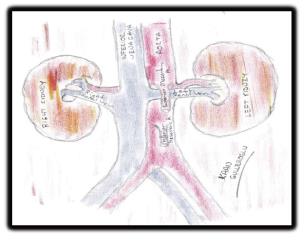
LRV entrapment divided into 2 types: anterior and posterior. Anterior NCS is the compression of a normally situated LRV by the abdominal aorta and the superior mesenteric artery (Figure 1). Posterior NCS is rare. It is presented with retroaortic LRV compressed usually between abdominal aorta and vertebral column. Other uncommon causes such as pancreatic neoplasm, paraaortic lymphadenopathy, retroperitoneal tumor, abdominal aortic aneurysm, overarching testicular artery, LRV duplication, and ectopic ventral right renal artery and strangulating fibrolymphatic tissue may play a role on the etiology of posterior NCS. Left renal ptosis, lordosis and decreased retroperitoneal and mesenteric fat tissue may cause to NCS[1-3].
Right-sided NCS is a more rare condition. Pregnancy is defining as a factor contributing to right-sided NCS by compression of large veins[1]. Left-sided IVC, hemiazygos continuation and persistent left superior vena cava combination is another rare cause of right NCS[4].
All of the anatomic mechanisms involved in renal vein compression are resulting with outflow obstruction leads to LRV hypertension with a measurable renocaval pressure gradient. The normal pressure gradient between the distal renal vein and IVC is < 1 mmHg. A renocaval pullback pressure gradient of ≥ 2 mmHg is highly suggestive of a nutcracker phenomenon[5]. LRV hypertension is the underlying mechanism which may result in formation of varices and collaterals. Venous sinuses in the neighboring of renal calyces were taken in form by these varices and collaterals. Hematuria and proteinuria are the results of these venous sinuses[6].
Prevalence of NCP is unknown. NCP may be higher in female. Affected persons are ranging from children and adolescents to middle-aged and older people with seventh decade of life[7]. Most symptomatic patients are in their second and third decade of life and a second peak of NCS occurs in middle-aged women[8]. Coincidental cases in siblings have been reported, although NCP is not a hereditary phenomenon[9]. The rapid increase in body height and the maturation of the vertebral bodies during puberty is resulting with decrease in the angle between the superior mesenteric artery and aorta. A low body mass index has been shown to correlate positively with NCS[10].
Clinical features of patients with NCS are various. The symptoms vary from asymptomatic hematuria to severe pelvic congestion. Some patients have severe and persistent symptoms. Symptoms are aggravated by physical activity[7]. Symptoms include hematuria, orthostatic proteinuria, flank pain, abdominal pain, varicocele, dyspareunia, dysmenorrhea, fatigue and orthostatic intolerance[11-13]. The symptoms of autonomic dysfunction such as hypotension, syncope, and tachycardia could be seen but they are rare[14]. Henoch-Schönlein purpura, IgA, nephropathy, membranous nephropathy, and idiopathic hypercalciuria with nephrolithiasis associated with NCS have been reported[12,15].
NCS can differentiate clinically into 2 subtypes as follows: typical presentation (or renal presentation) and atypical presentation (or urologic presentation). Typical clinical presentation include hematuria (micro- to macrohematuria), orthostatic proteinuria with or without flank pain. Abdominal pain, varicocele, dyspareunia, dysmenorrhea, fatigue and orthostatic intolerance are the components of the atypical presentation (Table 1).
| Renal presentation | Urologic presentation | |
| Hematuria | + | - |
| Orthostatic proteinuria | + | - |
| Flank pain | + | - |
| Abdominal pain | - | + |
| Varicocele | - | + |
| Dyspareunia | - | + |
| Dysmenorrhea | - | + |
| Fatigue | - | + |
| Orthostatic intolerance | - | + |
The most common symptom is hematuria. It is due to elevated LRV pressure resulting in the rupture of thin-walled septum between the varices and the collecting system in the renal fornix. Hematuria varies from micro- to macrohematuria. LRV is correspondent in this variation[14]. Isolated hematuria was reported 33.3% in children with NCS. Microhematuria is 4 times more common than macrohematuria[16].
Orthostatic proteinuria is another common symptom in NCS. The degree of proteinuria is variable. The incidence of orthostatic proteinuria is high during puberty. The mechanism of orthostatic proteinuria was not well understood yet. Changes of renal hemodynamic and the elevated levels of norepinephrine and angiotensin II were thought as the causes[17].
Pain is a result of the inflammatory cascade triggered by venous hypertension. Flank pain and abdominal pain are the consequences of that inflammatory process[1]. Left flank pain can be due also to urethral colic related to blood clots passing down to left ureter[7].
Varicocele affects 5.5%-9.5% of men and usually occurs on the left side. Development of varicocele is related with high LRV pressure and collateral circulation. Collateral veins could be demonstrated on pelvic and abdominal Doppler ultrasonography or venography[11].
Variations of normal anatomy must be considered before the diagnosis. Asymptomatic dilatation of LRV is frequently seen on ultrasonography or computed tomography, has been accepted as a finding of a normal variant[18]. NCS can exist without distended LRV. Normal flow also can exist in distended LRV[11]. Therefore, the first diagnostic need must be clinical examination. Existence of the clinical features constitutes a basis for the diagnosis. The presence of macroscopic or microscopic hematuria and proteinuria must evaluate. Urine analysis, urine phase contrast microscopy, urine culture and imaging of kidneys should be performed. Several imaging methods are used to diagnose NCS. Doppler ultrasonography, computed tomography angiography (CTA), magnetic resonance angiography (MRA) and retrograde venography are utilized.
Doppler ultrasonography can be used as the first diagnostic test in patients with suspected NCS. Length of the LRV is 6 to 10 cm and the average normal LRV diameter is 4 to 5 mm[7]. The normal pressure gradient between LRV and IVC is 1 mmHg or lower An elevated gradient > 3 mmHg between the LRV and the IVC can be used as a criteria of diagnosis for NCS[5]. Diameter of normal left gonadal vein is approximately 3 mm[19]. The normal superior mesenteric artery (SMA) originates behind the neck of the pancreas at the level of the first lumbar vertebra, and usually creates an acute angle at its origin from the aorta. Mean SMA angle is 51 ± 25º and mean SMA-aorta distance is 16 ± 6 mm in normal adults. Mean SMA angles in children are 45.8 ± 18.2º for boys and 45.3 ± 21.6º for girls. Mean SMA-aorta distances in children are 11.5 ± 5.3 mm for boys and 11.5 ± 4.5 mm for girls[20]. The standards of ultrasound diagnosis of NCS are descript by Zhang et al[21]: (1) the flow velocity of stenosis of the LRV in the supine position accelerates remarkably, and the acceleration, which is more than 100 cm/s, is more obvious after the patient has stood for 15 min; (2) the inner diameter ratio between ratio between the renal hilum and stenosis of the LRV in the supine position is > 3 and is > 5 after the patient has stood for 15 min[21]. Doppler ultrasonography has a sensitivity of 78% and a specificity of 100%[22]. However, in children the use of these criteria is limited because the smallest LRV sampling area and the largest Doppler angle than in adults[23].
CTA and MRA provide visualization of the anatomy. These tests can demonstrate the precise LRV compression point and/or prestenotic dilatation of the LRV together with perirenal and/or gonadal vein varices[24]. “Beak sign” is the abrupt narrowing of the LRV with a triangular shape at the aortomesenteric portion. It might be most useful finding among the various CT parameters, because it showed sensitivity 91.7% and specificity 88.9%[25]. MRA finding are similar to CT findings and MRA has the advantages of being less invasive with less amount of radiation than retrograde venography.
Retrograde venography is the gold standard for the diagnosis of NCS. It is not only confirming anatomic change, but also show a pressure gradient across the area of entrapment. Reflux of contrast into adrenal and gonadal veins from periureteral and perirenal venous collaterals, and pooling of contrast into the renal vein can be demonstrated[22]. Retrograde venography is the most informative method although it is an invasive test. It is not commonly performed in patients who have not severe symptoms.
Another invasive test such as cystoscopy may be helpful to identify hematuria from left ureteral origin. Notching from varicosities of the renal pelvis and ureters may be seen[26]. Cystoscopy is an indirect diagnostic method for NCS diagnosis.
NCS is a type of spectral disease and varies in severity and symptoms, reflecting degrees of LRV compression, LRV hypertension and the compensatory stage related to the development of collaterals[11]. The management of NCS depends upon the clinical presentation and the severity of the LRV hypertension. The treatment options are ranged from surveillance to nephrectomy. Treatment decision should be based on the severity of symptoms and their expected reversibility with regard to patient’s age and the stage of the syndrome[27]. Mild and tolerable symptoms can be followed conservatively. However, recurrent gross hematuria with anemia, severe flank pain, renal functional impairment, and inefficacy or aggravation of conservative treatment of the persistent orthostatic proteinuria after 24 mo of follow-up might require surgical treatment[18].
Spontaneous resolution by physical development during childhood is possible[18]. Conservative approach with observation during minimum 2 years without medication is the best option for patients younger than 18 years old. Seventy-five percent of patients with hematuria have complete resolution during this time[7]. Angiotensin inhibitors could be effective in patients with especially severe and prolonged orthostatic proteinuria[1].
Surgical procedures are used for treatment in patients with severe symptoms. Nephropexy, intravascular and extravascular stent implantation, transposition of the LRV or SMA, gonadocaval bypass, renal autotransplantation and nephrectomy are surgical procedures.
Open surgical techniques for anterior NCS include LRV transposition, LRV transposition with patch venoplasty, patch venoplasty without LRV transposition, LRV transposition with saphenous vein cuff, gonadal vein transposition and saphenous vein bypass[28]. LRV transposition is the most frequent and most effective technique in which LRV is transposed distally to the IVC. The LRV is transected and re-anastomosed to the IVC in a more distal location and in a tension-free end-to-side fashion. LRV transposition with patch venoplasty is used in conditions as permanent distortion of the vein with prolonged compression of the LRV or overstretched LRV because of the prominent aorta. The great saphenous vein is used as a patch to augment the LRV-IVC confluence after transposition of the LRV. Patch venoplasty without LRV transposition technique is used when transposition is not favorable because of the short renal vein is short or it is not improve the external compression of the vein. In LRV transposition with saphenous vein cuff technique the saphenous vein is used to form a cuff extension to the LRV to create tension-free anastomosis. Decrease of pelvic congestion and decompression of LRV can be obtained by left gonadal vein transposition. Saphenous vein also can be used for the bypass of the decompressed segment of the LRV[28].
Anterior transposition of LRV is used for posterior variant of NCS. In this technique LRV is excised with a small rim of the caval wall, and transposed to IVC, in a proximal position, via anteaortic routing[29].
Surgical placement of an external stent to the LRV is another surgical approach to NCS [5]. Endovascular stenting is an alternative treatment option. It can be preferred to open surgery because of the long period of renal congestion, additional anastomoses and extensive dissection requirement of the open surgery. Thrombosis, stent migration, fracture and restenosis are the complications of the endovascular stenting but they are rare[30].
NCS is a type of spectral disease and varies in severity and symptoms. Variations of normal anatomy must be considered before the diagnosis. Existence of the clinical features constitutes a basis for the diagnosis. The management of NCS depends upon the clinical presentation and the severity of the LRV hypertension.
P- Reviewer: Bianchetti MG, Greenwell TJ S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
| 1. | He Y, Wu Z, Chen S, Tian L, Li D, Li M, Jin W, Zhang H. Nutcracker syndrome--how well do we know it? Urology. 2014;83:12-17. [PubMed] |
| 2. | Shah D, Qiu X, Shah A, Cao D. Posterior nutcracker syndrome with left renal vein duplication: An uncommon cause of hematuria. Int J Surg Case Rep. 2013;4:1142-1144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Basile A, Tsetis D, Calcara G, Figuera M, Coppolino F, Patti MT, Midiri M, Granata A. Nutcracker syndrome due to left renal vein compression by an aberrant right renal artery. Am J Kidney Dis. 2007;50:326-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Yildiz AE, Cayci FS, Genc S, Cakar N, Fitoz S. Right nutcracker syndrome associated with left-sided inferior vena cava, hemiazygos continuation and persistant left superior vena cava: a rare combination. Clin Imaging. 2014;38:340-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Venkatachalam S, Bumpus K, Kapadia SR, Gray B, Lyden S, Shishehbor MH. The nutcracker syndrome. Ann Vasc Surg. 2011;25:1154-1164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | PYTEL A. Renal fornical hemorrhages: their pathogenesis and treatment. J Urol. 1960;83:783-789. [PubMed] |
| 7. | Kurklinsky AK, Rooke TW. Nutcracker phenomenon and nutcracker syndrome. Mayo Clin Proc. 2010;85:552-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 345] [Cited by in RCA: 323] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 8. | Rudloff U, Holmes RJ, Prem JT, Faust GR, Moldwin R, Siegel D. Mesoaortic compression of the left renal vein (nutcracker syndrome): case reports and review of the literature. Ann Vasc Surg. 2006;20:120-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 94] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 9. | Matsukura H, Arai M, Miyawaki T. Nutcracker phenomenon in two siblings of a Japanese family. Pediatr Nephrol. 2005;20:237-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Ozkurt H, Cenker MM, Bas N, Erturk SM, Basak M. Measurement of the distance and angle between the aorta and superior mesenteric artery: normal values in different BMI categories. Surg Radiol Anat. 2007;29:595-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 83] [Article Influence: 4.6] [Reference Citation Analysis (1)] |
| 11. | Takebayashi S, Ueki T, Ikeda N, Fujikawa A. Diagnosis of the nutcracker syndrome with color Doppler sonography: correlation with flow patterns on retrograde left renal venography. AJR Am J Roentgenol. 1999;172:39-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 114] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Alaygut D, Bayram M, Soylu A, Cakmakcı H, Türkmen M, Kavukcu S. Clinical course of children with nutcracker syndrome. Urology. 2013;82:686-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Del Canto Peruyera P, Vaquero Lorenzo F, Vallina-Victorero Vazquez MJ, Alvarez Salgado A, Vicente Santiago M, Botas Velasco M, Alvarez Fernandez LJ. Recurrent hematuria caused by nutcracker syndrome. Ann Vasc Surg. 2014;28:1036.e15-1036.e19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Daily R, Matteo J, Loper T, Northup M. Nutcracker syndrome: symptoms of syncope and hypotension improved following endovascular stenting. Vascular. 2012;20:337-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Altugan FS, Ekim M, Fitöz S, Ozçakar ZB, Burgu B, Yalçınkaya F, Soygür T. Nutcracker syndrome with urolithiasis. J Pediatr Urol. 2010;6:519-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Shin JI, Park JM, Lee JS, Kim MJ. Effect of renal Doppler ultrasound on the detection of nutcracker syndrome in children with hematuria. Eur J Pediatr. 2007;166:399-404. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 75] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 17. | Mazzoni MB, Kottanatu L, Simonetti GD, Ragazzi M, Bianchetti MG, Fossali EF, Milani GP. Renal vein obstruction and orthostatic proteinuria: a review. Nephrol Dial Transplant. 2011;26:562-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 18. | Wang L, Yi L, Yang L, Liu Z, Rao J, Liu L, Yang J. Diagnosis and surgical treatment of nutcracker syndrome: a single-center experience. Urology. 2009;73:871-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 63] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 19. | Park SJ, Lim JW, Ko YT, Lee DH, Yoon Y, Oh JH, Lee HK, Huh CY. Diagnosis of pelvic congestion syndrome using transabdominal and transvaginal sonography. AJR Am J Roentgenol. 2004;182:683-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 141] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 20. | Arthurs OJ, Mehta U, Set PA. Nutcracker and SMA syndromes: What is the normal SMA angle in children? Eur J Radiol. 2012;81:e854-e861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Zhang H, Li M, Jin W, San P, Xu P, Pan S. The left renal entrapment syndrome: diagnosis and treatment. Ann Vasc Surg. 2007;21:198-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 93] [Article Influence: 5.2] [Reference Citation Analysis (1)] |
| 22. | Noorani A, Walsh SR, Cooper DG, Varty K. Entrapment syndromes. Eur J Vasc Endovasc Surg. 2009;37:213-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 23. | Park SJ, Lim JW, Cho BS, Yoon TY, Oh JH. Nutcracker syndrome in children with orthostatic proteinuria: diagnosis on the basis of Doppler sonography. J Ultrasound Med. 2002;21:39-45; quiz 46. [PubMed] |
| 24. | Bhanji A, Malcolm P, Karim M. Nutcracker syndrome and radiographic evaluation of loin pain and hematuria. Am J Kidney Dis. 2010;55:1142-1145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Kim KW, Cho JY, Kim SH, Yoon JH, Kim DS, Chung JW, Park JH. Diagnostic value of computed tomographic findings of nutcracker syndrome: correlation with renal venography and renocaval pressure gradients. Eur J Radiol. 2011;80:648-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 92] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 26. | Wendel RG, Crawford ED, Hehman KN. The “nutcracker“ phenomenon: an unusual cause for renal varicosities with hematuria. J Urol. 1980;123:761-763. [PubMed] |
| 27. | Shin JI, Baek SY, Lee JS, Kim MJ. Follow-up and treatment of nutcracker syndrome. Ann Vasc Surg. 2007;21:402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Said SM, Gloviczki P, Kalra M, Oderich GS, Duncan AA, D Fleming M, Bower TC. Renal nutcracker syndrome: surgical options. Semin Vasc Surg. 2013;26:35-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 29. | Marone EM, Psacharopulo D, Kahlberg A, Coppi G, Chiesa R. Surgical treatment of posterior nutcracker syndrome. J Vasc Surg. 2011;54:844-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 30. | Chen S, Zhang H, Shi H, Tian L, Jin W, Li M. Endovascular stenting for treatment of Nutcracker syndrome: report of 61 cases with long-term followup. J Urol. 2011;186:570-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 85] [Article Influence: 6.1] [Reference Citation Analysis (0)] |