Revised: April 24, 2014
Accepted: May 14, 2014
Published online: August 6, 2014
Processing time: 319 Days and 15.8 Hours
AIM: To investigate a potential protective role of the kinin B2 receptor in a glycerol-induced rhabdomyolysis mouse model.
METHODS: We separated 28 C57Bl/6 male mice into 4 groups: untreated WT animals, untreated B2 knockout mice, glycerol-treated WT and glycerol-treated B2 knockout mice. Glycerol-treated animals received one intramuscular injections of glycerol solution (50% v/v, 7 mL/kg). After 48 h, urine and blood samples were collected to measure creatinine and urea levels. Additionally, kidney samples were extracted for histological evaluation, and the mRNA expression levels of kinin B1 and B2 receptors and inflammatory mediators were measured by real-time polymerase chain reaction.
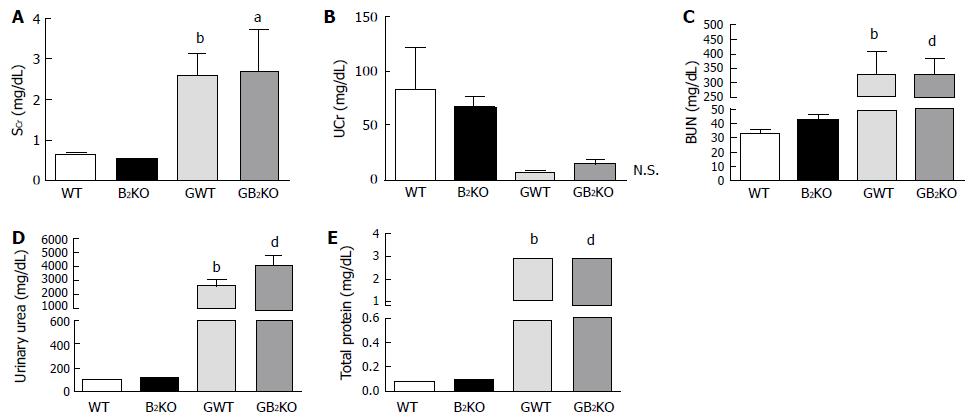
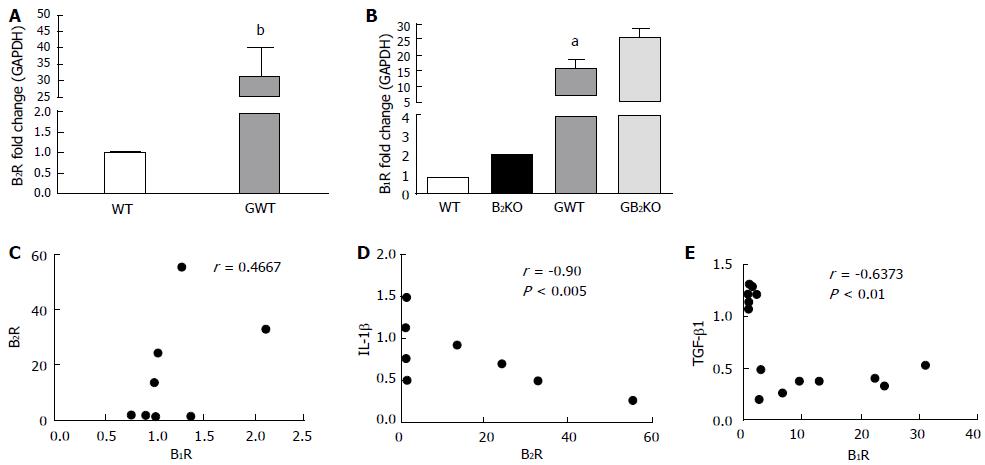
RESULTS: Serum creatinine and urea levels showed differences between untreated wild-type and glycerol-treated wild-type mice (0.66 ± 0.04 vs 2.61 ± 0.53 mg/dL, P < 0.01; and 33.51 ± 2.08 vs 330.2 ± 77.7 mg/dL, P < 0.005), and between untreated B2 knockout mice and glycerol-treated knockout mice (0.56 ± 0.03 vs 2.23 ± 0.87 mg/dL, P < 0.05; and 42.49 ± 3.2 vs 327.2 ± 58.4 mg/dL, P < 0.01), but there was no difference between the glycerol-treated wild-type and glycerol-treated knockout mice. Glycerol was able to induce a striking increase in kinin B2 receptor expression (> 30 times, 31.34 ± 8.9) in kidney. Animals injected with glycerol had a higher degree of tubular injury than untreated animals. Wild-type and knockout mice treated with glycerol intramuscularly present kidney injury, with impairment in renal function. However, B2 knockout mice treated with glycerol did not show a different phenotype regarding kidney injury markers, when compared to the wild-type glycerol-treated group.
CONCLUSION: We conclude that the kinin B2 receptor does not have a protective role in renal injury.
Core tip: In this work we are showing that glycerol-treated animals experienced impairment in renal function. Furthermore, we worked with kinin B2 receptor knockout mice and our results suggest that kinin B2 receptor does not exert renoprotective effects in this rhabdomyolysis model. In addition, we are presenting results of kidney expressions and we investigated several candidates that can participate in the kidney injury induced by glycerol.
- Citation: Gattai PP, Mafra FFP, Wasinski F, Almeida SS, Cenedeze MA, Malheiros DMAC, Bacurau RFP, Barros CC, Câmara NOS, Araujo RC. Kinin B2 receptor does not exert renoprotective effects on mice with glycerol-induced rhabdomyolysis. World J Nephrol 2014; 3(3): 85-91
- URL: https://www.wjgnet.com/2220-6124/full/v3/i3/85.htm
- DOI: https://dx.doi.org/10.5527/wjn.v3.i3.85
Acute kidney injury (AKI) is a common life-threatening disease that places a heavy burden on the health system[1]. It was reported that the mortality rate for this disease ranges from 10% to 80%. Other studies suggest that AKI may be a step in the progression toward chronic kidney disease[2], in humans and animals[3].
The main factors that predispose patients to AKI include hemodynamic instability, hypovolemia, hypoxia, ischemia and reperfusion (I/R), and burns, among others[4]. There are several models used to study this disease; one of them is the glycerol-induced rhabdomyolysis model in which AKI occurs after muscle injury. In this nephrotoxic experimental model, the waste products from metabolism, such as enzymes and other molecules (e.g., uric acid and myoglobin), cause kidney injury to the proximal and distal tubules[4]. Such injuries cause an abrupt (in a matter of hours or days) decline in renal function.
In renal inflammatory conditions such as AKI, the kallikrein-kinin system (KKS) plays an important role in glucose homeostasis[5,6]. This system is also involved in kidney inflammatory and vasodilation processes[7], which are directly involved in the inflammatory response mechanism of AKI. The AKI inflammatory response involves induction of local vascular ischemia, hypoxia and tubular injury[4]. KKS exerts its actions by activating two receptors: B1 (B1R) and B2 (B2R)[8]. The activation of B1R is inducible and occurs under pathological conditions such as in ischemia[9], while B2R is constitutively active under normal physiological circumstances[8]. Furthermore, some authors[10] have shown that there are fewer B2R in rat nephrons affected by renal disease. It is well established that kinins are rapidly generated after tissue injury and that they have a central role in the development and maintenance of inflammatory processes, whether they are acute or chronic[1].
There is a renal KKS[11] that can respond in a more specific way to AKI. Another system that could be involved in the mechanism of AKI, as observed in the glycerol-induced rhabdomyolysis model, is the renin-angiotensin system (RAS). A drop in blood pressure, typically observed during a hypovolemic state, will activate this system and induce renal perfusion[12]. It is important to note that, the renal KKS can activate RAS[13]. In a recent study from our laboratory[14], we showed that there is a relationship between the genetic polymorphisms of ACE and B2R, where the former can modulate the kinins in transplanted kidney patients. In other animal models of renal injury, it has been shown that B2 has a possible protective role[15], while others have shown that it has a deleterious role[16].
It is described in the literature that the B2R are in all portions of the nephron, except in podocytes of human kidney[17]. Moreover, it is described that the NO levels fall in rhabdomyolysis[4], and that the B2R activation is related with NO production[18]. Thus, the purpose of this study is to investigate the role of B2R in the kidney in an animal model of glycerol-induced rhabdomyolysis.
This study began only with approval of the ethics committee of the Federal University of Sao Paulo (UNIFESP, nº 0300/11), and experiments were performed in accordance with the guidelines established by the Brazilian College for Animal Experimentation. The animals were provided by the Center for Development of Experimental Medicine and Biology (CEDEME) at UNIFESP. Twenty-eight male 3-month-old C57Bl/6 mice were used. Animals were randomly divided into 4 groups: WT (n = 5), glycerol WT (GWT, n = 9), B2KO (n = 6), and glycerol B2KO (GB2KO, n = 8). All animals were placed in individual cages (Alesco, Brazil) in an environment with controlled temperature (21 °C), a light/dark cycle of 12 h for one week and water and standard chow ad libitum.
The WT and B2KO groups were control groups and received no treatment. The animals in the treated groups were deprived of water for 18 h to better evidence of AKI. Animals of both treatment groups (GWT and GB2KO) were then slightly sedated with an intraperitoneal injection of ketamine-xylazine solution (150 µL, Vetnil, Brazil; at 10 μL/g, Vetbrands Brazil, Brazil), and received an i.m. injection of glycerol solution (50% v/v, Merk, Brazil, 7 mL/kg), with half a dose in each gastrocnemius muscle. Then, animals were placed back in their cages in a heated environment until recovery.
The urine samples were placed in 2 mL tubes and stored at -20 °C until analysis. Then, 48 h after the injections, the animals were anesthetized with i.p. ketamine-xylazine solution (300 μL at 10 μL/g), and blood samples were collected by intracardiac puncture into non-heparinized 1.5 mL tubes. These samples were incubated for approximately 20 min at room temperature and were then centrifuged at 4 °C at 4000 rpm for 10 min. The serum was collected and stored in a 1.5 mL tube at -20 °C until analysis. After blood sample collection, the animals were sacrificed by cervical dislocation, and each kidney was removed, weighed and transversally cut. One piece was placed in one 2 mL tube and immediately immersed in liquid nitrogen and then stored at -80 °C until analysis, while the other half was placed in a 2 mL tube with 10% buffered formaldehyde solution for 24 h, then placed into a new tube with a 70% ethanol solution and stored until sectioning.
For renal function analysis, we measured serum creatinine (SCr) levels and urine creatinine levels (UCr) according to the method described by Jaffé with slight modifications[19]. Briefly, we deproteinized the samples by adding 100 μL of each serum sample to a 1.5 mL tube containing 200 μL of 1.84 % H2SO4 and 300 μL of sodium tungstate and thoroughly mixed the resulting solution. The tubes were maintained at room temperature for 15 min and then centrifuged for 10 min at 4000 rpm at room temperature. The supernatant was then collected and placed in another 1.5 mL tube. Then, 5.28 mL of picric acid was mixed with 1.32 mL of a 10% NaOH solution in a 14 mL falcon tube. Next, 100 μL of picric acid (Labtest Diagnostica SA, Brazil) was added to 63 wells of a 96-well flat-bottomed ELISA microplate (Cral plast, Brazil), followed by pipetting and mixing of 200 μL of Milliq H2O (Millipore, United States) in triplicate for blank samples, 200 μL of standard protein at 5 mg/mL in triplicate, and 200 μL of each deproteinized sample in duplicate. The plate was incubated for 20 min and then read in an EPOCH spectrophotometer (Biotek Instruments Inc., United States) at 450 nm. To measure UCr levels, we used the same method, but we did not deproteinize the samples. Instead, we diluted the samples (1:125) and multiplied the results by 25. The blood urea nitrogen (BUN) level were measured by colorimetric reaction kit (Labtest diagnostica, Brazil) in spectrophotometer at 600 nm, following the manufacturer’s instructions.
Urine was collected by direct punction in bladder, for measure of creatinine and urea levels. The urine was collected in 1.5 mL tubes.
We also quantified the total urine protein (mg/dL) by colorimetric assay at 660 nm using the Pierce Protein Assay Kit (Thermo Scientific, United States).
Total RNA was extracted using the TRIzol Reagent method (Invitrogen, United States) from tissues and stored at -80 °C. The samples were run on 1% agarose gels to evaluate the integrity of the samples, and the samples were then quantified using a nanoDrop (NanoDrop Technologies, Inc., United States). Single-stranded cDNA was synthesized for each sample, using MML-V reverse transcriptase (Promega, United States). The qRT-PCR was carried out using Taqman (Applied Byosystem, United States) probes for GAPDH, B1R and B2R gene expression, and SYBR Green Real-time polymerase chain reaction (PCR) (Applied Byosystem, United States) probes for β-actin (sense - 5’ CTG GCC TCA CTG TCC ACC TT 3’ , antisense - 5’ CGG ACT CAT CGT ACT CCT GCT T 3’), TGF-β1 (sense - 5’ TTA GGA AGG ACC TGG GTT GG 3’ , antisense - 5’ AAG TTG GCA TGG TAG CCC TT 3’) and IL-1β (sense - 5’ AGG AGA ACC AAG CAA CGA CA 3’ , antisense - 5’ CGT TTT TCC ATC TTC TTC TTT 3’) gene expression. The plates were placed in a 7500 real-time PCR system (Applied Biosystems, United States) for reading. The fold change was calculated by taking the 2-∆CT of each sample and dividing it by the wild type (WT) group average.
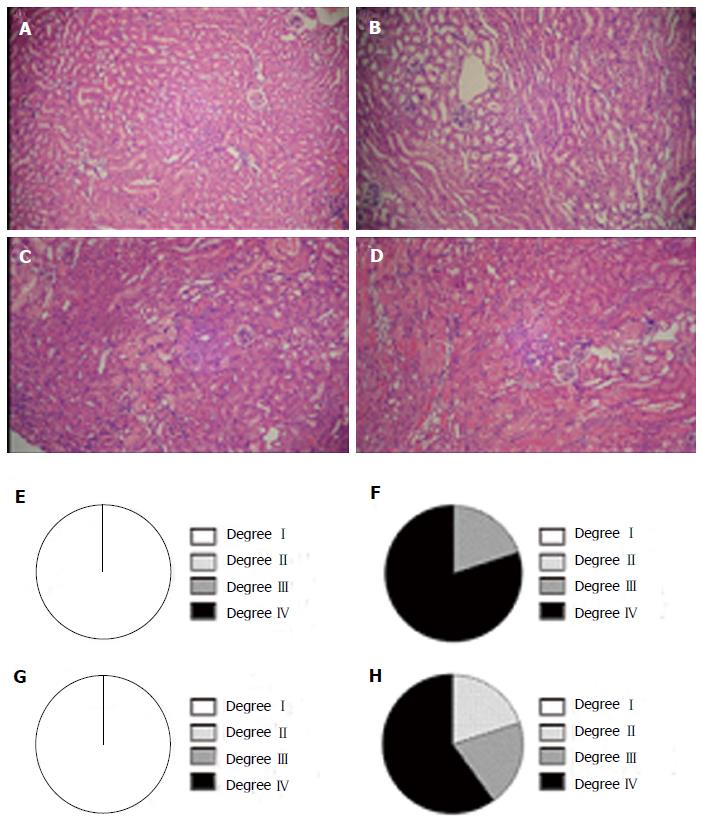
Slices 5 μm thick were cut from the samples stored in 70% ethanol solution and stained with HE. The samples were analyzed using an optical microscope at 200 × magnification. The criteria used to analyze the tubular injury in the samples included epithelium desquamation, cellular debris in the lumen, flattening of epithelium, the presence of cylinders and dilation of the lumen. Based on these criteria, an expert classified and scored the injuries: grade I (< 10%), grade II (10%-25%), grade III (25-50%), and grade IV (> 50%).
The values are expressed as the mean ± SE. Statistical analyses were carried out by one-way ANOVA (analysis of variance) followed by Tukey’s post-hoc test, and associations were made by the Spearman correlation test. P values < 0.05 were considered statistically significant. The statistical software used for graphs and analysis was GraphPad Prism 5.
The SCr levels were different between the control wild-type and glycerol, and knockout control group and glycerol, with glycerol groups greater about 4 times than control groups (Figure 1A). There were no significant differences in the Ucr levels, despite the wild-type showed about 11 times higher levels than glycerol wild-type group (Figure 1B). The BUN levels were different about 10 times between the control wild-type and glycerol, and about 8 times between control knockout mice and glycerol (Figure 1C). Urinary urea content differed between the control and glycerol groups, about 24 times for wild-type groups and about 33 times for knockout groups (Figure 1D). The levels of total urine proteins were different between the wild-type and glycerol group (around 42 times), while the difference between knockout and glycerol group was approximately 36 times. There were no difference between wild-type glycerol and knockout glycerol group (Figure 1E).
The fold changes in B1R, B2R, β-actin, IL-1β and TGF-β1 renal expression are shown in Figure 2. Also shown are the associations between these expression levels. The fold change of the B2R was different between the control and glycerol groups about 30 times (Figure 2A). The B1R fold change was different between the control and glycerol groups about 14 times, and between glycerol groups almost 2 times (Figure 2B). The associations were not different between the B1R and B2R (Figure 2C), but showed difference between B2R and IL-1β, where greater expression of B2R results in lower expression of IL-1β (Figure 2D), and between B1R and TGF-β1 groups, with greater expression of B1R when the expression of TGF- β1 is lower (Figure 2E).
The histological evaluation and histomorphometry shown in Figure 3 demonstrate that both sets of animals (WT and B2KO) had a high degree of tubular injury when injected with glycerol (Figure 3F and H), but WT had a higher degree IV compared with B2KO.
It is described that the NO levels fall in rhabdomyolysis[4], and that the B2R activation is related with NO production[18] we considered investigate the role of kinin B2 receptor in glycerol-induced rhabdomyolysis model.
Our findings demonstrate that the renal expression of B2R in animals that received glycerol is 30 times greater than that of the controls. Another study showed a 5-fold increase of B2R expression[15]. These results suggest that B2R may be involved in the kidney inflammatory process. Interestingly, the peak renal expression of B2R coincided with a significant reduction in renal function, which could suggest that the renal upregulation of these receptors occurs in response to renal injury.
Renal function was evaluated by measuring serum creatinine and BUN levels. In mice, particularly male C57Bl/6 mice, the normal serum creatinine level (SCr) is approximately 0.8 ± 0.1 mg/dL[20], which is similar to the values found in the control groups (Table 1). In a recent study[21], the authors showed using the glycerol model in rats, that the peak of renal function impairment occurs between 48 and 72 h, as evidenced by SCr levels. In our study, we investigated the peak of injury.
Kidney injury in the glycerol model is due to the release of nephrotoxic molecules and proteins (e.g., myoglobin) into the bloodstream, causing damage upon reaching the kidney[4]. The literature describes, using rat and cell culture models[22-27], the deleterious role of this protein, specifically the heme prosthetic group, in the tubular endothelium. This role is associated with the production of reactive oxygen species (ROS) and free radicals in the mitochondria, which initiate lipid peroxidation reactions.
It has been shown that human skeletal muscle can survive for up to 3 or 4 h during circulatory ischemia[28]. In other studies[24], the authors showed that in the rat glycerol-induced rhabdomyolysis model, the renal mitochondria were already markedly degenerated 3 h after the glycerol application. Twenty-four hours after treatment, there were clear signs of tubular necrosis (proximal and distal). The authors attributed this to the formation of intra-tubular aggregates. This conclusion suggests that disruption of skeletal muscle can occur approximately 3 h after the glycerol administration.
Recent studies[28-31] show that deletion of B1R and B2R exacerbates the renal phenotype in diabetic mouse models, suggesting that both receptors have a protective effect on diabetic nephropathy by suppressing oxidative stress via NO and prostaglandins. However, because the absence of one of the receptors causes increased expression of the other, it is difficult to determine the precise function of each receptor[28]. In other models, such as the I/R model[15] the receptors’ role was also studied. Blocking B1R showed an antifibrotic effect, which therefore has a protective effect. Some authors[16] have demonstrated that renal injury by ischemia and reperfusion is significantly increased by B2R activation and that this activation is related to increased production of ROS, suggesting that B2R activation is deleterious.
Kinin receptors in renal tissue were studied in the I/R model, where it was shown that both receptors have a protective role in this type of injury[30]. However, a different study[15] found that during I/R in mice, the double knockout showed an extremely high SCr along with a proinflammatory profile. The renal B2R expression alternated, beginning with low expression after 4 h, high expression after 24 h, and 48 h after the reperfusion onset, its expression level was similar to that observed at 4 h and then increased to values similar to those observed at 24 h post-reperfusion.
An important difference between the previous two studies[15,24] and ours is that in the other studies, ischemia and reperfusion were induced exclusively in the kidneys, whereas in our work, nephrotoxic kidney injury occurs after induction of primary skeletal muscle injury. Furthermore, in the model we use, there is no time for reperfusion to occur because the peak of injury would be 48 h later, allowing the kidneys to therefore remain in an ischemic state.
Regarding the release of proinflammatory cytokines (e.g., IL-1β) and growth factors with a known profibrotic effect (TGF-β1), some authors[21] have shown that in the rat glycerol model, the mRNA expression levels of IL-1β peak 48 h after treatment, while in our work, the same expression levels were observed in GB2KO animals, whereas GWT animals showed expression levels similar to those found 24 h post-treatment by these authors. In our study, we found a strong negative association between the expression of B2R and IL-1β, which may indicate that B2R does not induce inflammation in the kidneys.
Previous studies show[21] that renal TGF-β1 expression 48 h after im glycerol injection in mice is 1.5 times greater than our results indicate. It is important to note that the lineage of the animals used was different and that the endogenous gene studied was also different. Furthermore, in our work, we did not find any association between renal expression of B2R and TGF-β1 (data not shown). Meanwhile, B1R and TGF- β1 had a strong negative association.
Another important issue regarding analysis of TGF-β1 expression is the methodological difference between the studies. Although both studies use rodents, rats and mice have differences in several genes, including TGF-β1; the rat version is on chromosome 1, while the murine version is located on chromosome 7.
In conclusion, our results suggest that B2R does not have a renoprotective role in mice with glycerol-induced rhabdomyolysis.
Acute kidney injury (AKI) is a common life-threatening disease that places a heavy burden on the health system and may be a step in the progression toward chronic kidney disease. It was reported that the mortality rate for this disease ranges from 10% to 80%, depending on the population studied. According to some authors, prevention is the key to avoiding the morbidity and mortality associated with AKI.
Kinins is related with several models of inflammatory process in different organs as well in kidney. However, there is a lack of acknowledgments about kinins and rhabdomyolysis. The kinins are related with pathologies as well in physiology process. However, the absence of B2 receptor can induces the expression of the kinin B1 receptor and it difficult the determination of the precise function of each receptor. In this study, the authors demonstrated that the overexpression of kinin B2 receptor could be involved with kidney injury once that the peak renal expression of kinin B2 receptor coincided with a significant reduction in renal function.
This is the first study reporting that kinin B2 receptor is over-expressed in kidney in rhabdomyolysis model. Furthermore, these results suggest that the over-expression may be one of the causes of kidney injury in this animal model.
Kinin B2 receptor antagonist could be tested in future to avoid kidney injury in rhabdomyolysis process.
Rhabdomyolysis is a skeletal muscle disease where the muscle tends to break, that commonly result in acute kidney injury. Bradykinin is a nonapeptide messenger that is enzymatically produced from kallidin and that act via activation of two membrane receptors: kinin B1 receptor and kinin B2 receptor. Kinin B1 receptor is a bradykinin receptor that is induced in response to inflammation, it may play a role in chronic inflammation. Kinin B2 receptor is a bradykinin receptor that is constitutively expressed and may play a role in the acute phase of inflammation.
Gattai et al reported that the kinin B2 receptor knockout. The authors provided detailed data on this and the manuscript is well written.
P- Reviewer: Fujigaki Y, Watanabe T S- Editor: Song XX L- Editor: A E- Editor: Wu HL
| 1. | Costa-Neto CM, Dillenburg-Pilla P, Heinrich TA, Parreiras-e-Silva LT, Pereira MG, Reis RI, Souza PP. Participation of kallikrein-kinin system in different pathologies. Int Immunopharmacol. 2008;8:135-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 63] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Heung M, Chawla LS. Predicting progression to chronic kidney disease after recovery from acute kidney injury. Curr Opin Nephrol Hypertens. 2012;21:628-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 3. | Sanoff S, Okusa MD. Impact of acute kidney injury on chronic kidney disease and its progression. Contrib Nephrol. 2011;171:213-217. [PubMed] |
| 4. | Bosch X, Poch E, Grau JM. Rhabdomyolysis and acute kidney injury. N Engl J Med. 2009;361:62-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 857] [Cited by in RCA: 897] [Article Influence: 56.1] [Reference Citation Analysis (0)] |
| 5. | Araújo RC, Mori MA, Merino VF, Bascands JL, Schanstra JP, Zollner RL, Villela CA, Nakaie CR, Paiva AC, Pesquero JL. Role of the kinin B1 receptor in insulin homeostasis and pancreatic islet function. Biol Chem. 2006;387:431-436. [PubMed] |
| 6. | Barros CC, Haro A, Russo FJ, Schadock I, Almeida SS, Reis FC, Moraes MR, Haidar A, Hirata AE, Mori M. Bradykinin inhibits hepatic gluconeogenesis in obese mice. Lab Invest. 2012;92:1419-1427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Bhoola KD, Figueroa CD, Worthy K. Bioregulation of kinins: kallikreins, kininogens, and kininases. Pharmacol Rev. 1992;44:1-80. [PubMed] |
| 8. | Regoli D, Barabé J. Pharmacology of bradykinin and related kinins. Pharmacol Rev. 1980;32:1-46. [PubMed] |
| 9. | Marceau F, Hess JF, Bachvarov DR. The B1 receptors for kinins. Pharmacol Rev. 1998;50:357-386. [PubMed] |
| 10. | Naicker S, Naidoo S, Ramsaroop R, Moodley D, Bhoola K. Tissue kallikrein and kinins in renal disease. Immunopharmacology. 1999;44:183-192. [PubMed] |
| 11. | Klein J, Buffin-Meyer B, Schanstra JP. The role of the renal kallikrein-kinin system in physiology and pathology. Kinins. Berlin: DeGruyter 2011; 103-110. |
| 12. | Canteras NS. Neural basis of motivated behaviors and emotions. Physiology. Rio de Janeiro: Guanabara Koogan 2011; 355. |
| 13. | Scicli AG, Carretero OA. Renal kallikrein-kinin system. Kidney Int. 1986;29:120-130. [PubMed] |
| 14. | Amorim CE, Nogueira E, Almeida SS, Gomes PP, Bacurau RF, Ozaki KS, Cenedeze MA, Silva Filho AP, Câmara NO, Araujo RC. Clinical impact of an angiotensin I-converting enzyme insertion/deletion and kinin B2 receptor +9/-9 polymorphisms in the prognosis of renal transplantation. Biol Chem. 2013;394:369-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Wang PH, Campanholle G, Cenedeze MA, Feitoza CQ, Gonçalves GM, Landgraf RG, Jancar S, Pesquero JB, Pacheco-Silva A, Câmara NO. Bradykinin [corrected] B1 receptor antagonism is beneficial in renal ischemia-reperfusion injury. PLoS One. 2008;3:e3050. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Chiang WC, Chien CT, Lin WW, Lin SL, Chen YM, Lai CF, Wu KD, Chao J, Tsai TJ. Early activation of bradykinin B2 receptor aggravates reactive oxygen species generation and renal damage in ischemia/reperfusion injury. Free Radic Biol Med. 2006;41:1304-1314. [PubMed] |
| 17. | Song Q, Wang DZ, Harley RA, Chao L, Chao J. Cellular localization of low-molecular-weight kininogen and bradykinin B2 receptor mRNAs in human kidney. Am J Physiol. 1996;270:F919-F926. [PubMed] |
| 18. | Kon V, Hunley TE. Kinins and Endothelin. Seldin and Giebisch’s The Kidney: Physiology and Pathophysiology. Manhattan: Elsevier/Academic Press 2007; 385-396. |
| 19. | Semedo P, Correa-Costa M, Antonio Cenedeze M, Maria Avancini Costa Malheiros D, Antonia dos Reis M, Shimizu MH, Seguro AC, Pacheco-Silva A, Saraiva Camara NO. Mesenchymal stem cells attenuate renal fibrosis through immune modulation and remodeling properties in a rat remnant kidney model. Stem Cells. 2009;27:3063-3073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 194] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 20. | Schnell MA, Hardy C, Hawley M, Propert KJ, Wilson JM. Effect of blood collection technique in mice on clinical pathology parameters. Hum Gene Ther. 2002;13:155-161. [PubMed] |
| 21. | Korrapati MC, Shaner BE, Schnellmann RG. Recovery from glycerol-induced acute kidney injury is accelerated by suramin. J Pharmacol Exp Ther. 2012;341:126-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 59] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 22. | Balla G, Vercellotti GM, Muller-Eberhard U, Eaton J, Jacob HS. Exposure of endothelial cells to free heme potentiates damage mediated by granulocytes and toxic oxygen species. Lab Invest. 1991;64:648-655. [PubMed] |
| 23. | Beetham R. Biochemical investigation of suspected rhabdomyolysis. Ann Clin Biochem. 2000;37:581-587. [PubMed] |
| 24. | Nath KA, Grande JP, Croatt AJ, Likely S, Hebbel RP, Enright H. Intracellular targets in heme protein-induced renal injury. Kidney Int. 1998;53:100-111. [PubMed] |
| 25. | Plotnikov EY, Chupyrkina AA, Pevzner IB, Isaev NK, Zorov DB. Myoglobin causes oxidative stress, increase of NO production and dysfunction of kidney’s mitochondria. Biochim Biophys Acta. 2009;1792:796-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 86] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 26. | Shah SV, Walker PD. Evidence suggesting a role for hydroxyl radical in glycerol-induced acute renal failure. Am J Physiol. 1988;255:F438-F443. [PubMed] |
| 27. | Zager RA, Burkhart K. Myoglobin toxicity in proximal human kidney cells: roles of Fe, Ca2+, H2O2, and terminal mitochondrial electron transport. Kidney Int. 1997;51:728-738. [PubMed] |
| 28. | Tomita H, Sanford RB, Smithies O, Kakoki M. The kallikrein-kinin system in diabetic nephropathy. Kidney Int. 2012;81:733-744. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 29. | Kakoki M, Takahashi N, Jennette JC, Smithies O. Diabetic nephropathy is markedly enhanced in mice lacking the bradykinin B2 receptor. Proc Natl Acad Sci USA. 2004;101:13302-13305. [PubMed] |
| 30. | Kakoki M, McGarrah RW, Kim HS, Smithies O. Bradykinin B1 and B2 receptors both have protective roles in renal ischemia/reperfusion injury. Proc Natl Acad Sci USA. 2007;104:7576-7581. [PubMed] |
| 31. | Kakoki M, Sullivan KA, Backus C, Hayes JM, Oh SS, Hua K, Gasim AM, Tomita H, Grant R, Nossov SB. Lack of both bradykinin B1 and B2 receptors enhances nephropathy, neuropathy, and bone mineral loss in Akita diabetic mice. Proc Natl Acad Sci USA. 2010;107:10190-10195. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 97] [Cited by in RCA: 94] [Article Influence: 6.3] [Reference Citation Analysis (0)] |