Published online Jun 25, 2025. doi: 10.5527/wjn.v14.i2.103756
Revised: February 23, 2025
Accepted: March 5, 2025
Published online: June 25, 2025
Processing time: 131 Days and 13.1 Hours
The discussion on renal biopsies and biomarkers highlights the essential aspects of nephrology. Although novel diagnostic biomarkers are emerging, renal biopsy remains critical for accurate diagnosis and treatment owing to the lack of suffi
Core Tip: Puspitasari et al reported significant changes in biopsy indications and histological outcomes before and after the coronavirus disease 2019 (COVID-19) pandemic, reflecting the interconnectedness of clinical practices, public health challenges, and patient demographics. Nevertheless, the COVID-19 pandemic has revealed vulnerabilities in nephrology services, necessitating flexible management strategies for chronic conditions.
- Citation: Gonzalez FM, Valjalo R. Essential role of kidney biopsy in diagnosing glomerular diseases amidst evolving biomarkers. World J Nephrol 2025; 14(2): 103756
- URL: https://www.wjgnet.com/2220-6124/full/v14/i2/103756.htm
- DOI: https://dx.doi.org/10.5527/wjn.v14.i2.103756
Renal biopsy has remained an essential tool for diagnosing and characterizing glomerular diseases for decades owing to the lack of validated and available substitute diagnostic biomarkers with high sensitivity and specificity. The most promising biomarkers have not yet been implemented in routine clinical practice because of insufficient validation in large cohorts, or because limited access or high costs prevent global implementation[1]. Consequently, most of the proposed biomarkers have not been incorporated into the current Kidney Disease: Improving Global Outcomes (KDIGO) guidelines for managing glomerular diseases. Consequently, renal biopsy has maintained its relevance, and its clinical utility remains highly valuable, providing definitive histological data that can guide the diagnosis, management, and prognostication of kidney diseases. Moreover, renal histology can lead to changes in treatment decisions in approximately 40% of cases[2,3].
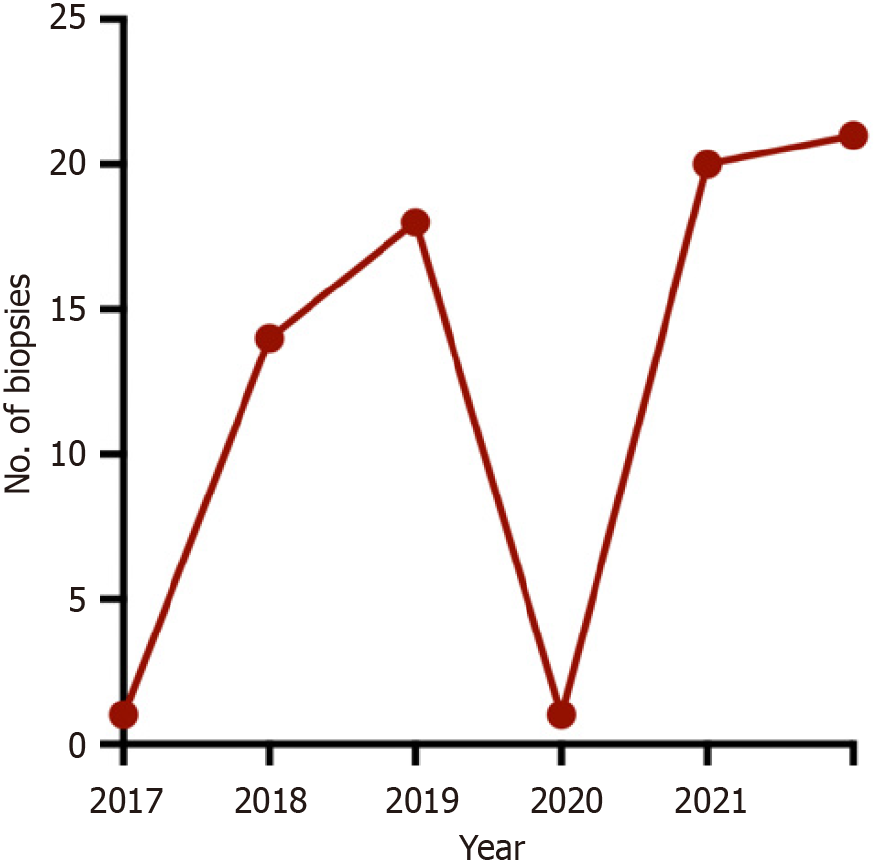
Most epidemiological studies on glomerular diseases involve large patient series that analyze the different histological patterns observed. These studies have shown heterogeneous results across regions, potentially influenced by demographic, genetic, environmental, and temporal factors, as well as other aspects such as variability in referral and biopsy policies between different countries and within regions[4,5]. In a recent issue of this journal, Puspitasari et al[6] described the frequency of renal biopsies performed and the histological patterns identified over six consecutive years, covering an initial period before the coronavirus disease 2019 (COVID-19) pandemic and a second period during and after the pandemic. Their results highlighted a dramatic reduction in the number of biopsies performed after the onset of the pandemic (2020), with lupus nephritis (LN) being the most frequently observed histological finding throughout the study period, accounting for one-third of the cases, followed by minimal change disease (MCD). After the onset of the COVID-19 pandemic, an increase in the proportion of biopsies showing LN and a significant reduction in biopsied MCD cases were observed compared with the pre-pandemic period. Although LN exhibited a frequency pattern similar to that reported in middle-income countries, where LN is the most common secondary glomerular disease in biopsies, a high proportion of MCD cases stood out[7]. As the authors noted, this high number of biopsies showing MCD might be explained by the over-representation of young individuals in the sample (40% being aged < 25 years), potentially at the expense of older individuals. There may also be some degree of overestimation of MCD diagnoses, differentiating MCD from focal segmental glomerulosclerosis can be challenging in early stages[8].
The significant changes observed in the frequencies of LN and MCD between the pre-and during/post-pandemic periods have not been consistently demonstrated in other studies[9]. These variations may reflect the influence of different biopsy criteria on renal biopsy data. During the periods of lockdown, social distancing, uncertainty, high care demand, and limited hospital bed availability, histological diagnostic efforts may have prioritized nephritic clinical phenotypes over nephrotic ones, which may have been treated empirically.
The correlation between the clinical and histopathological diagnoses in nephrology is critical, especially considering the nuances associated with nephritic and nephrotic syndromes. The predominance of nephritic syndrome in the clinical indications for biopsy in the study by Puspitasari et al[6], despite the higher prevalence of nephrotic syndromes reflected in the final diagnoses, raises important questions regarding clinical decision-making. Interestingly, a substantial pro
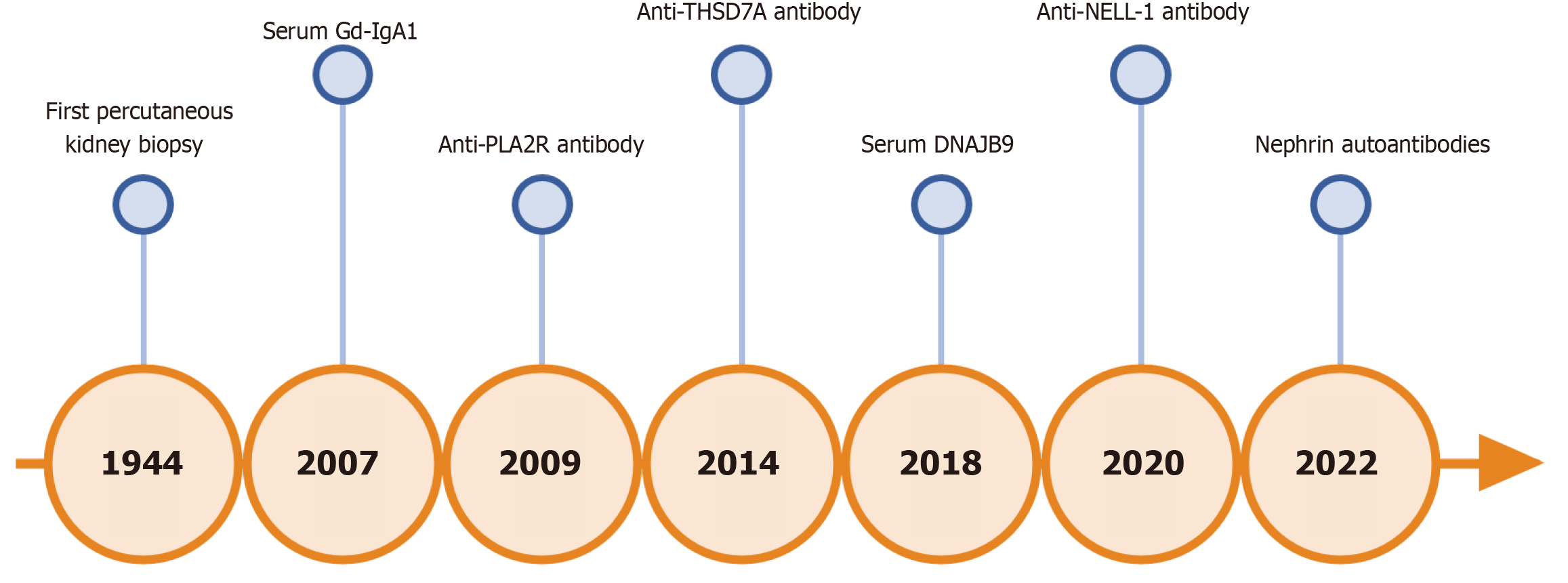
Over the past two decades, significant progress has been made in elucidating the mechanisms underlying the pathogenesis of various glomerular diseases, thereby enhancing the development of diagnostically useful biomarkers (Figure 1). The shift towards utilizing biomarkers, as outlined in the KDIGO guidelines, reflects an evolving approach for diagnosing and managing kidney diseases. This shift is becoming increasingly essential owing to the potential risks associated with invasive diagnostic strategies, such as biopsies, and the need for shorter diagnostic times. The discovery and recommendation to measure serum antibodies against the phospholipase A2 receptor (PLA2R) in cases of nephrotic syndrome suggests a move towards more targeted treatment interventions, potentially reducing the need for invasive biopsy procedures[10]. In addition to the anti-PLA2R antibodies used for diagnosing membranous nephropathy, the detection of autoantibodies against thrombospondin type 1 domain-containing 7A and neural epidermal growth factor-like 1 may prove useful[11,12]; these antibodies are present in 10% and 16% of the cases of anti-PLA2R-negative membranous nephropathy, respectively. The recent identification of anti-nephrin antibodies as potential biomarkers for podocyte diseases, particularly in diagnosing MCD, has made significant advances, although further validation and confirmation of these findings are necessary[13,14]. As the field of nephrology continues to evolve, it is likely that other serological markers (such as anti-double-stranded DNA antibodies for LN, anti-PLA2R antibodies for membranous nephropathy, and ANCAs for microscopic polyangiitis) will similarly influence clinical practice and renal biopsy decisions. Consequently, it is crucial to discover, research, and validate high-performance biomarkers to ensure that they are affordable for most centers worldwide.
Ultimately, the clinical diagnosis remains paramount in guiding the decision to perform a biopsy. Greater awareness and education regarding the different presentations of nephrotic and nephritic syndromes, along with the integration of emerging biomarkers into clinical practice, can lead to improved patient outcomes. Developing protocols that balance clinical evaluation with serological testing may streamline the diagnostic process, ensuring that patients receive timely and appropriate management of their renal condition.
The COVID-19 pandemic caused serious direct and indirect adverse health outcomes in nephrologic patients, who faced collateral reductions in access to care based on the pandemic's impact on healthcare facilities in each region. In some countries, significant reductions were observed in access to dialysis as well as in outpatient and inpatient nephrologic care. This resulted in a reduction in the number of dialysis stations, an increase in absenteeism rates, a higher patient-to-nurse ratio, and deterioration of patients' laboratory and dialysis adequacy parameters[15,16]. In addition, there was a global decline in the number of transplants and donations from living and deceased donors[17-19]. Notably, in Europe, the kidney transplantation rate decreased by 22.5%, affecting most countries[19]. This decline is particularly critical, as patients on the waiting list face greater risks of complications and mortality than those who receive transplants. Similar to the findings of Puspitasari et al, several reports have noted a marked reduction in the number of renal biopsies performed immediately after the onset of the pandemic, followed by an increase in the later period (Figure 2)[6,17,20,21]. The COVID-19 pandemic and subsequent lockdowns significantly impacted various aspects of care for nephrology patients. Ensuring sustained access to optimal care for patients requiring renal replacement and complex procedures in response to future large-scale events is crucial.
In conclusion, although the identification of appropriate biomarkers is valuable, the definitive diagnosis of glomerular diseases (with a few exceptions) ultimately relies on kidney biopsies. This procedure, coupled with a thorough histopathological analysis, provides critical insights that aid clinical nephrologists in comprehending the underlying pathology affecting patients. Such an understanding is essential for guiding evidence-based treatment strategies and enhancing the prediction of medium- and long-term patient prognosis. Furthermore, accurate diagnosis and treatment planning can help select specific and non-specific therapeutic interventions—including renin-angiotensin axis blockade, inhibition of type 2 sodium-glucose co-transporter, mineralocorticoid receptor antagonism, and glucagon-like peptide-1 agonism—ensuring that therapies are tailored to the specific needs of each patient for optimal outcomes.
Francisca González Cohens because of her valuable help in correcting and editing this English version.
| 1. | Catanese L, Rupprecht H, Huber TB, Lindenmeyer MT, Hengel FE, Amann K, Wendt R, Siwy J, Mischak H, Beige J. Non-Invasive Biomarkers for Diagnosis, Risk Prediction, and Therapy Guidance of Glomerular Kidney Diseases: A Comprehensive Review. Int J Mol Sci. 2024;25:3519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Asad RA, Valson AT, Kavitha V, Korula A, Eapen A, Rebekah G, Jacob S, Pathak H, Alexander S, Mohapatra A, David VG, Varughese S, Tamilarasi V, Basu G. Safety and utility of kidney biopsy in patients with estimated glomerular filtration rate < 30 ml/min/1.73 m(2). Nephrology (Carlton). 2021;26:659-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Richards NT, Darby S, Howie AJ, Adu D, Michael J. Knowledge of renal histology alters patient management in over 40% of cases. Nephrol Dial Transplant. 1994;9:1255-1259. [PubMed] |
| 4. | McGrogan A, Franssen CF, de Vries CS. The incidence of primary glomerulonephritis worldwide: a systematic review of the literature. Nephrol Dial Transplant. 2011;26:414-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 521] [Cited by in RCA: 465] [Article Influence: 33.2] [Reference Citation Analysis (0)] |
| 5. | O'Shaughnessy MM, Hogan SL, Thompson BD, Coppo R, Fogo AB, Jennette JC. Glomerular disease frequencies by race, sex and region: results from the International Kidney Biopsy Survey. Nephrol Dial Transplant. 2018;33:661-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 143] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 6. | Puspitasari M, Wardhani Y, Sattwika PD, Wijaya W. Patterns of kidney diseases diagnosed by kidney biopsy and the impact of the COVID-19 pandemic in Yogyakarta, Indonesia: A single-center study. World J Nephrol. 2024;13:100087. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Ekrikpo U, Obiagwu P, Chika-Onu U, Yadla M, Karam S, Tannor EK, Bello AK, Okpechi IG. Epidemiology and Outcomes of Glomerular Diseases in Low- and Middle-Income Countries. Semin Nephrol. 2022;42:151316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 8. | Sim JJ, Smoyer WE, Schachter AD. Minimal Change Disease and FSGS Are a Spectrum of a Single Disease within Immune-Mediated Nephrotic Syndrome. Kidney360. 2024;5:1197-1199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 9. | Valjalo R, Villalobos A, Ruiz A, Segura P, Avila E, Fulgeri C, Musalem P, Navarro F, Pais E, Cordero C, Mansilla R, Reynolds E, Contreras F, Hellman E, Año A, Hernández M. WCN24-2633 Impact of the COVID-19 pandemic on the frequency of glomerular disease in a population with low prevalence of APOL1 risk variants. Kidney Int Rep. 2024;9:S213-S215. [DOI] [Full Text] |
| 10. | Beck LH Jr, Bonegio RG, Lambeau G, Beck DM, Powell DW, Cummins TD, Klein JB, Salant DJ. M-type phospholipase A2 receptor as target antigen in idiopathic membranous nephropathy. N Engl J Med. 2009;361:11-21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1888] [Cited by in RCA: 1664] [Article Influence: 104.0] [Reference Citation Analysis (0)] |
| 11. | Tomas NM, Beck LH Jr, Meyer-Schwesinger C, Seitz-Polski B, Ma H, Zahner G, Dolla G, Hoxha E, Helmchen U, Dabert-Gay AS, Debayle D, Merchant M, Klein J, Salant DJ, Stahl RAK, Lambeau G. Thrombospondin type-1 domain-containing 7A in idiopathic membranous nephropathy. N Engl J Med. 2014;371:2277-2287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 592] [Cited by in RCA: 664] [Article Influence: 60.4] [Reference Citation Analysis (0)] |
| 12. | Sethi S, Debiec H, Madden B, Charlesworth MC, Morelle J, Gross L, Ravindran A, Buob D, Jadoul M, Fervenza FC, Ronco P. Neural epidermal growth factor-like 1 protein (NELL-1) associated membranous nephropathy. Kidney Int. 2020;97:163-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 230] [Article Influence: 38.3] [Reference Citation Analysis (0)] |
| 13. | Watts AJB, Keller KH, Lerner G, Rosales I, Collins AB, Sekulic M, Waikar SS, Chandraker A, Riella LV, Alexander MP, Troost JP, Chen J, Fermin D, Yee JL, Sampson MG, Beck LH Jr, Henderson JM, Greka A, Rennke HG, Weins A. Discovery of Autoantibodies Targeting Nephrin in Minimal Change Disease Supports a Novel Autoimmune Etiology. J Am Soc Nephrol. 2022;33:238-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 209] [Article Influence: 69.7] [Reference Citation Analysis (0)] |
| 14. | Hengel FE, Dehde S, Lassé M, Zahner G, Seifert L, Schnarre A, Kretz O, Demir F, Pinnschmidt HO, Grahammer F, Lucas R, Mehner LM, Zimmermann T, Billing AM, Oh J, Mitrotti A, Pontrelli P, Debiec H, Dossier C, Colucci M, Emma F, Smoyer WE, Weins A, Schaefer F, Alachkar N, Diemert A, Hogan J, Hoxha E, Wiech T, Rinschen MM, Ronco P, Vivarelli M, Gesualdo L, Tomas NM, Huber TB; International Society of Glomerular Disease. Autoantibodies Targeting Nephrin in Podocytopathies. N Engl J Med. 2024;391:422-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 94] [Article Influence: 94.0] [Reference Citation Analysis (0)] |
| 15. | Prasad N, Bhatt M, Agarwal SK, Kohli HS, Gopalakrishnan N, Fernando E, Sahay M, Rajapurkar M, Chowdhary AR, Rathi M, Jeloka T, Lobo V, Singh S, Bhalla AK, Khanna U, Bansal SB, Rai PK, Bhawane A, Anandh U, Singh AK, Shah B, Gupta A, Jha V. The Adverse Effect of COVID Pandemic on the Care of Patients With Kidney Diseases in India. Kidney Int Rep. 2020;5:1545-1550. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 16. | Naga YS, El Keraie A, Abd ElHafeez SS, Zyada RS. Impact of COVID-19 pandemic on care of maintenance hemodialysis patients: a multicenter study. Clin Exp Nephrol. 2024;28:1040-1050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 17. | Hussein NR, M Saleem ZS, Ibrahim N, Musa DH, Naqid IA. The impact of COVID-19 pandemic on the care of patients with kidney diseases in Duhok City, Kurdistan Region of Iraq. Diabetes Metab Syndr. 2020;14:1551-1553. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 18. | Zhang C, Kodali L, Mour G, Jadlowiec C, Mathur AK. The impact of COVID-19 on kidney transplant care. Front Med (Lausanne). 2022;9:1093126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 19. | Kramer A, Jager KJ, Chesnaye NC, Kerschbaum J, Hommel K, Comas Farnés J, Trujillo Alemán S, Santamaria R, Finne P, Hemmelder MH, Åsberg A, Nitsch D, Ambühl P, Sørensen SS, Sánchez-Alvarez JE, Segelmark M, Resic H, Ots-Rosenberg M, Radunovic D, Palsson R, Santiuste de Pablos C, Rodríguez Arévalo OL, Legeai C, Lausevic M, Bakkaloglu SA, Ortiz A, Stel VS. Changes in the epidemiology of kidney replacement therapy across Europe in 2020-the first year of the COVID-19 pandemic: an ERA Registry study. Nephrol Dial Transplant. 2024;39:1835-1845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Hakroush S, Tampe D, Korsten P, Tampe B. Impact of the COVID-19 Pandemic on Kidney Diseases Requiring Renal Biopsy: A Single Center Observational Study. Front Physiol. 2021;12:649336. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Chandra A, Rao N, Malhotra KP, Srivastava D. Impact of COVID 19 pandemic on patients requiring renal biopsy. Int Urol Nephrol. 2022;54:2617-2623. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |