Published online May 25, 2023. doi: 10.5527/wjn.v12.i3.56
Peer-review started: December 25, 2022
First decision: February 8, 2023
Revised: February 22, 2023
Accepted: March 22, 2023
Article in press: March 22, 2023
Published online: May 25, 2023
Processing time: 145 Days and 1.6 Hours
There are two known types of exercise-induced acute renal failure. One is the long-known myoglobinuria-induced acute renal failure due to severe rhabdomyolysis, and the other is the recently recognized non-myoglobinuria-induced acute renal failure with mild rhabdomyolysis. Exercise-induced acute renal failure was first reported in 1982. Non-myoglobinuria-induced acute renal failure is associated with severe low back pain and patchy renal vasoconstriction, and it is termed post-exercise acute renal failure because it usually occurs hours after exercise. It is also called acute renal failure with severe loin pain and patchy renal ischemia after anaerobic exercise (ALPE).
To makes a significant contribution to medical literature as it presents a study that investigated a not-widely-known type of exercise-induced acute renal failure known as ALPE.
We performed a database search selecting papers published in the English or Japanese language. A database search was lastly accessed on September 1, 2022. The results of this study were compared with those reported in other case series.
The study evaluated renal hypouricemia as a key risk factor of ALPE. The development of ALPE is due to the sum of risk factors such as exercise, hypou
In conclusion, hypouricemia plays a key role in the development of ALPE and is often associated with anaerobic exercise. The development of ALPE is a result of the cumulative effects of risk factors such as exercise, hypouricemia, NSAIDs, vasopressors, and dehydration.
Core Tip: Exercise is important for health maintenance and promotion. However, exercise-induced acute renal failure is a disease that athletes and doctors should be aware of. This paper makes a significant contribution to medical literature as it presents a study that investigated a not-widely-known type of exercise-induced acute renal failure known as Acute renal failure with severe Loin pain and Patchy renal ischemia after anaerobic Exercise (ALPE). Further, the study evaluated renal hypouricemia as a key risk factor of ALPE. The information in this paper can help clinicians make more accurate diagnosis, given that a significant proportion of patients with ALPE are undiagnosed. Further, this paper can increase awareness among athletes to help them prevent ALPE and reach their exercise goals.
- Citation: Tamura H. Acute renal failure with severe loin pain and patchy renal ischemia after anaerobic exercise. World J Nephrol 2023; 12(3): 56-65
- URL: https://www.wjgnet.com/2220-6124/full/v12/i3/56.htm
- DOI: https://dx.doi.org/10.5527/wjn.v12.i3.56
There are two known types of exercise-induced acute renal failure (ARF). One is the long-known myoglobinuria-induced ARF due to severe rhabdomyolysis, and the other is the recently recognized non-myoglobinuria-induced ARF with mild rhabdomyolysis. The distinguishing features of the two types of exercise-induced ARF are summarized in Table 1.
| ALPE | Myoglobinuria acute renal failure | |
| Amount of exercise | + | +++ |
| Type of exercise | Anaerobic exercise | Aerobic exercise |
| Urine volume | Non-oliguria | Oliguria |
| Reddish brown urine | - | +++ |
| Loin pain | +++ | -~+ |
| Nausea, vomiting/slight fever | ++ | +- |
| Dehydration | + | +++ |
| Serum CK/serum myoglobin | normal or mildly elevated | ↑↑↑ |
Exercise-induced ARF was first reported by Ishikawa in 1982. Non-myoglobinuria-induced ARF is associated with severe low back pain and patchy renal vasoconstriction, and it is termed post-exercise ARF because it usually occurs hours after exercise. It is also known as ARF with severe loin pain and patchy renal ischemia after anaerobic exercise (ALPE)[1].
Recently, many reports of post-exercise ARF, especially in patients with renal hypouricemia, have attracted attention. Thus, in this study, we report on the types of ALPE.
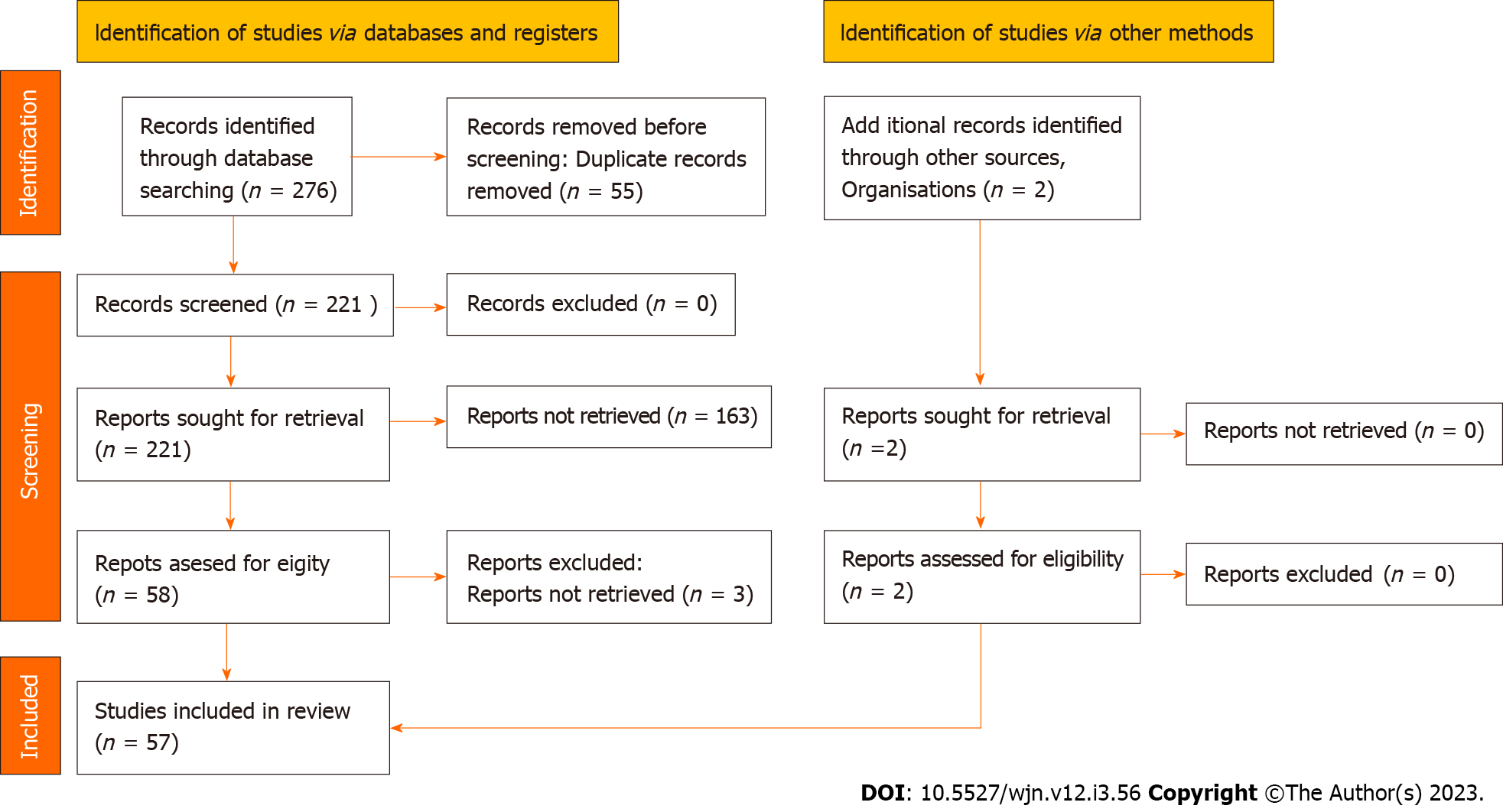
We searched PubMed for studies on ALPE and summarized 57 reported cases of ALPE, including self-examination cases[2-29] (Figure 1). The following patient characteristics were investigated: Sex, age at ARF episode, past history, first symptom of the ARF episode, type of exercise leading to ARF, date of ARF episode, first examination data of the ARF episode, baseline levels of uric acid, and treatment of ARF.
The results of this study were compared with those reported in other case series[30,31].
We compared the characteristics of patients with ALPE and renal hypouricemia with those of patients with ALPE without renal hypouricemia.
The characteristics of patients with ALPE with and without renal hypouricemia were compared with those reported in other case series[32].
We summarized 57 reported cases of ALPE, including self-examination cases (Table 2). ALPE most commonly occurs post-exercise (82.5%) and in men (91.2%). In addition to back pain (63.2%) at the first hospital visit, many patients with ALPE present with abdominal pain (56%), vomiting (63.2%), mild fever (33.3%), and high C-reactive protein (CRP) levels (72.2%).
| Age (yr) | 22.09 ± 9.55 (13-65) |
| Sex | Male 52 (91.2%), female 5 (8.8%) |
| Exercise | 47/57 (82.5) |
| Fever | 19/57 (33.3) |
| Nausea/vomiting | 36/57 (63.2) |
| Loin pain | 36/57 (63.2) |
| Abdominal pain | 32/57 (56.1) |
| High blood pressure on admission | 10/30 (33.3) |
| High CRP on admission | 13/18 (72.2) |
| Serum creatinine on admission (mg/dL) | 4.81 ± 2.25 (1.08-12.1), n = 56 |
| Serum myoglobin on admission (ng/mL) | 86.46 ± 66.80 (10-260), n = 21 |
| Serum CK on admission (IU/L) | 272.76 ± 301.97 (38-1182), n = 47 |
| Kidney CT patchy findings | 32/40 (80) |
| Hemodialysis | 10/54 (18.5) |
| Hydration | 37/54 (68.5) |
| Hydration+drugs | 6/54 (11.1) [furosemide (2), dopamine (2), nicardipine (1), Vitamin C, E (1)] |
| Rest | 1/54 (1.9) |
| Renal hypouricemia | 31/57 (54.4) |
| Recurrence of ALPE | 14/54 (25.9) |
| Days of renal failure improvement | 17.4 ± 10.4 (d), n = 35 |
| Premedication | 5/26 (19) [vasopressor (2), NSAIDs (1), Antibiotic agent (1), epileptic drugs (1)] |
Wedge-shaped scars were noted on contrast-enhanced computed tomography (CT) in 80% of the cases. The mean serum creatinine, creatine phosphokinase, and myoglobin levels at initial presentation were 4.81 mg/dL, 272 IU/L, and 86 ng/mL, respectively. Moreover, most of the patients (68.5%) only received hydration therapy, 18.5% of the patients underwent hemodialysis (HD), and only a few patients were treated with oral medications. The mean recovery period was approximately 17 d, 25.9% of the patients had ALPE recurrence, and 54.4% of the patients presented with hypouricemia.
The results of this study were comparable with those of the other case series (Table 3).
| This cases | Ohta et al[31], 2004 | Ishikawa et al[30], 2002 | |
| Age (yr) | 22.1 ± 9.6 (13-65) | 19.3 ± 8.1 (11-46) | 22.0 ± 7.6 (10-54) |
| Sex (male) | 52/57 (91.2) | 48/54 (88.9) | 112/118 (94.9) |
| Fever | 19/57 (33.3) | 7/60 (11.7) | 38/47 (80.9) |
| Nausea/vomiting | 36/57 (63.2) | 51/60 (85) | 84/88 (95.5) |
| Loin pain | 36/57 (63.2) | 35/60 (58.3) | NA |
| Abdominal pain | 32/57 (56.1) | 22/60 (36.7) | NA |
| Serum creatinine on admission (mg/dL) | 4.81 ± 2.52 (N = 56) | NA | 4.70 ± 2.90 (N = 77) |
| Kidney CT patchy findings | 32/40 (80) | NA | 49/96 (92) |
| Hemodialysis | 10/54 (18.5) | NA | 20/118 (16.9) |
| Exercise | 47/57 (82.5) | 61/61 (100) | 118/118 (100) |
| Renal hypouricemia | 31/57 (54.4) | 48/48 (100) | 49/96 (51) |
| Recurrence of ALPE | 14/54 (25.9) | 13/54 (24.1) | 20/118 (16.9) |
| Days of renal failure improvement | 17.4 ± 10.4 (N = 35) | NA | 13.1 ± 8.3 (N = 87) |
Table 4 shows the comparison of the characteristics of patients with ALPE with and without renal hypouricemia. The mean duration of acute kidney injury with hypouricemia was 17.9 d, whereas that of acute kidney injury without hypouricemia was 16.1 d. Overall, 24% of patients underwent HD, 12% of whom did not have hypouricemia. ALPE recurrence with hypouricemia was observed in 39% of patients and that without hypouricemia in 12% of the patients.
| Renal hypouricemia | No renal hypouricemia | |
| Number of patients | 31 | 26 |
| Age (yr) | 21.6 ± 10.7 (11-65) | 22.7 ± 8.0 (13-49) |
| Sex (male) | 28/31 (90) | 24/26 (92) |
| fever | 7/31 (23) | 12/26 (46) |
| Nausea/vomiting | 22/31 (71) | 14/26 (54) |
| Loin pain | 21/31 (68) | 15/26 (58) |
| Abdominal pain | 14/31 (45) | 18/26 (69) |
| High blood pressure on admission | 6/21 (28.6) | 4/9 (44.4) |
| High CRP on admission | 9/14 (64.3) | 4/4 (100) |
| Serum creatinine on admission (mg/dL) | 4.53 ± 2.04 (N = 30) | 5.24 ± 2.81 (N = 26) |
| Serum CK on admission (IU/L) | 261 ± 304 (N = 26) | 269 ± 225 (N = 21) |
| Kidney CT patchy findings | 9/15 (60) | 23/25 (92) |
| Hemodialysis | 7/29 (24) | 2/25 (8) |
| Exercise | 29/31 (94) | 19/26 (73) |
| Recurrence of ALPE | 11/28 (39) | 3/26 (12) |
| Days of renal failure improvement | 17.9 ± 8.3 (N = 26) | 16.1 ± 15.3 (N = 10) |
| premedication | 2/20 (10) | 3/6 (50) |
The findings of this study were consistent with those of previous studies (Table 5).
| Renal hypouricemia, this cases | Renal hypouricemia, Ishikawa[32], 2014 | No renal hypouricemia, this cases | No renal hypouricemia, Ishikawa[32], 2014 | |
| Number of patients | 31 | 148 | 26 | 94 |
| Age (yr) median | 18 (11-65) | 18 (15-25) | 21 (13-49) | 19 (16-26) |
| Sex (male) | 28/31 (90) | 136/148 (92) | 24/26 (92) | 82/92 (89) |
| Fever | 7/31 (23) | 35/43 (81) | 12/26 (46) | 35/49 (71) |
| Nausea/vomiting | 22/31 (71) | 106/107 (99) | 14/26 (54) | 63/66 (95) |
| Serum CK on admission (IU/L) | 155 (44-1182), N = 26 | 212 (100-447), N = 81 | 225 (38-686), N = 21 | 317 (124-696), N = 70 |
| Serum creatinine on admission (mg/dL) | 4.2 (1.1-8.9), N = 30 | 4.3 (2.6-6.7), N = 122 | 4.7 (1.4-7.6), N = 26 | 3.2 (2-5.1), N = 75 |
| Kidney CT patchy findings | 9/15 (60) | 31/32 (97) | 23/25 (92) | 56/58 (97) |
| Hemodialysis | 7/29 (24) | 46/148 (31) | 2/25 (8) | 16/94 (17) |
| Recurrence of ALPE | 11/28 (39) | 38/148 (26) | 3/26 (12) | 7/94 (7) |
| Days of renal failure improvement (d) | 17 (6-30), N = 26 | 14 (10-19), N = 85 | 15 (5-22), N = 10 | 10 (7-16), N = 66 |
The clinical features of ALPE are as follows[33]: ARF (A), severe back (loin) pain (L), and patchy renal ischemia of acute onset (P) after anaerobic exercise (E). Most patients with ALPE (approximately 90%) are men, and the age of onset is as low as 15-17 years. Most cases have been reported so far in Japan, and the relationship between ALPE and renal hypouricemia has attracted attention. Some patients administered antipyretic analgesics before exercise and had a slight cold. The risk factors for ALPE are summarized below.
Exercise: The types of exercises include anaerobic and repeated anaerobic exercises, such as track and field (sprinting), soccer, muscle training, swimming, cycling, baseball, and weightlifting. ALPE most commonly occurs after sprinting 200 m multiple times at sports festivals[34].
Loin pain: Loin pain refers to severe pain that seems to originate from the kidney, rather than from the muscles of the extremity used during exercise. It occurs 1–48 h (typically 3-12 h) after exercise. The pain is bilateral and mostly described as back pain, but it is occasionally described as abdominal, low back, or flank pain.
High pain severity does not allow patients with loin pain to drive a car. In addition, the patients complain of nausea, vomiting, and abdominal pain. They present to the hospital with mild fever and slightly high CRP levels.
Renal hypouricemia: Patients with ALPE and renal hypouricemia typically have more frequent relapses, more severe ARF, and longer recovery periods than those with ALPE and no renal hypouricemia. Since the identification of the gene for renal hypouricemia in Japan[35], post-exercise ARF has been gaining popularity as a complication of renal hypouricemia.
Clinically misdiagnosed diseases: ALPE may include clinically misdiagnosed diseases, such as urinary tract stones, acute gastroenteritis, acute pancreatitis, acute glomerulonephritis, acute pyelonephritis, and lumbago.
Diagnostic method: Having sufficient knowledge of ALPE is the first step in its diagnosis. A considerable number of ALPE cases may remain undiagnosed and are overlooked. It is important to obtain a medical history of exercise, especially anaerobic exercise, for accurate diagnosis of ALPE.
(1) History of repeated anaerobic exercise or exercise set that includes anaerobic exercise; (2) Back pain experienced 1-48 h (typically 3–12 h) after exercise; (3) Normal or slightly elevated serum creatine kinase (CK) levels (serum CK levels that are ≤ 9 times the reference value and serum myoglobin levels that are ≤ 7 times the reference value); and (4) Wedge-shaped residual contrast medium observed on delayed CT (1–2 d after the administration of the contrast medium) when the serum creatinine level is 1.2-3.5 mg/dL. ARF with criteria (1) to (3) is required for the diagnosis of ALPE; however, criterion (4) is not required for clinical diagnosis[33]. In rare cases, patients do not complain of back pain or remember exercising. These cases are considered atypical.
In atypical cases of ALPE, urinalysis does not show reddish-brown urine, patients usually have nonoliguric ARF, and oliguria is rare. The level of fractional excretion of sodium fluctuates between < 1% and > 1%. Furthermore, proteinuria and hematuria may be positive or negative, and the result of urinalysis is not definitive. Dehydration is rare, and the blood pressure level at the time of admission is usually normal.
Treatment: A considerable number of patients with low back pain several days after a sports festival may be overlooked without a diagnosis of ALPE who ultimately heal spontaneously. If a patient with ALPE presents to an emergency department with pain, nonsteroidal anti-inflammatory drugs (NSAIDs) should not be administered without consideration. This is because NSAIDs may exacerbate ARF, leading to oliguria and the need for dialysis therapy. If analgesia is considered necessary, centrally administered analgesics should be used instead of NSAIDs. The treatment is initially conservative. Hydration should be normal, and body weight should be maintained at the presymptomatic value. Regarding fluid balance, body weight should be controlled to the standard value with fluid replacement in cases of dehydration, and diuretics should be administered in cases of excess body fluid. Dialysis therapy is rarely used for treating oliguria, uremia, hyperkalemia, and heart failure.
Prevention: The management of patients with renal hypouricemia (particularly those with serum uric acid levels of ≤ 1 mg/dL) is an issue at school club activities and sports festivals. As ALPE recurs easily, patients with a history of ALPE should be advised to be wary of dehydration and of types of exercise likely to induce ALPE. These patients should also be advised to take preventive steps such as avoiding exercises that induce ALPE. However, there is yet no established definitive prevention method against ALPE recurrence. There is insufficient evidence to prove that drugs suppressing the generation of reactive oxygen species, such as allopurinol and vitamins A, C, and E, prevent ALPE[1].
The pathophysiological mechanism of ALPE is unknown, but renal circulatory impairment due to reactive oxygen species (ROS) is believed to be the main cause of ALPE[36].
Strenuous exercise, such as anaerobic exercise, generates large amounts of ROS, which are rapidly cleared by uric acid, a potent ROS scavenger, and other scavengers in healthy populations[37]. Consequently, patients with renal hypouricemia have insufficient scavengers, leading to inadequate ROS clearance, resulting in the activation of vasoconstrictors, vasoconstriction, and renal ischemia[31].
As renal vasoconstriction is known to cause further vasoconstriction and oxidative stress via the activation of the renin–angiotensin system as well as increased blood pressure level[38], patients with ALPE may be in a vicious cycle of oxidative stress and vasoconstriction. Oxidative stress causes stronger vasoconstriction, which in turn causes more oxidative stress, leading to acute ischemia and severe renal damage. The ischemia is localized to the kidney, but on rare occasions, it spreads to other organs. In extremely rare cases, it is accompanied by a spasm of the cerebral vessels, resulting in reversible occipital lobe leukoencephalopathy[39].
Genetic abnormalities in patients with renal hypouricemia who develop ALPE include mutations in the uric acid transporter URAT1, homozygotes for W258X, and compound heterozygotes including URAT1 and W258X. Homozygotes for R90H have also been reported[40].
Based on these findings, hypouricemia, rather than genetic mutation, is considered a risk factor for ALPE. In fact, patients with renal hypouricemia are approximately 50 times more likely to develop ALPE than those with nonrenal hypouricemia[32].
The case of a patient with ALPE without exercise who had no episodes of strenuous exercise was recently reported by Lee et al[29] However, enhanced CT revealed characteristic patchy renal signs.
To the best of our knowledge, 10 patients with ALPE without an episode of strenuous exercise have been reported so far, 8 of whom had an infection or took a vasopressor or analgesic before the onset of ALPE. Moreover, infection and vasopressor and analgesic use are considered as risk factors for ALPE (Table 6)[3,12,28,31].
| Patient No. | Age (yr) | Sex | Renal hypouricemia | Suspected trigger |
| 1 | 14 | Male | Yes | Gastroenteritis |
| 2 | 30 | Male | Yes | NA |
| 3 | 33 | Male | NR | URI and heavy alcoholconsumption |
| 4 | 23 | Female | NR | URI |
| 5 | 25 | Male | No | URI |
| 6 | 32 | Male | No | NSAIDs |
| 7 | 30 | Male | NR | NA |
| 8 | 49 | Male | Yes | Coincidence of myalgia |
| 9 | 15 | Male | Yes | Vasopressor |
| 10 | 65 | Male | Yes | Ureteral stone and NSAIDs |
The abovementioned reports suggest that ALPE can develop without strenuous exercise or other risk factors.
Aomura et al[3] reported ALPE in a patient who took vasopressors for orthostatic dysregulation for 15 days before the onset of ALPE.
It is possible that vasopressors induced or exacerbated ALPE by increasing ROS levels, worsening vasoconstriction, and forming a vicious cycle of decreased renal hemodynamics.
Karasawa et al[17] reported the case of a patient who was administered the vasoconstrictor midodrine before the onset of ALPE.
Radaković et al[41] demonstrated that vasodilation with low-dose dopamine improved the renal arteriolar resistance index in two cases of ALPE, suggesting a relationship between vasopressors and ALPE in clinical settings.
No study has directly addressed the relationship between vasopressors and ALPE; however, previous studies have shown the importance of catecholamine level homeostasis in the pathogenesis of ALPE. Vasopressors may be associated with the development of ALPE in patients with hypouricemia and may be a risk factor for ALPE.
In conclusion, hypouricemia plays a key role in the development of ALPE and is often associated with anaerobic exercise. The development of ALPE is a result of the cumulative effects of risk factors such as exercise, hypouricemia, NSAIDs, vasopressors, and dehydration.
Recently, many reports of post-exercise acute renal failure, especially in patients with renal hypouricemia, have attracted attention. The pathophysiological mechanism of acute renal failure with severe loin pain and patchy renal ischemia after anaerobic exercise (ALPE) is unknown, but renal circulatory impairment due to reactive oxygen species is believed to be the main cause of ALPE. Hypouricemia plays a key role in the development of ALPE and is often associated with anaerobic exercise.
Exercise is important for health maintenance and promotion. However, exercise-induced acute renal failure is a disease that athletes and doctors should be aware of.
This paper makes a significant contribution to medical literature as it presents a study that investigated a not-widely-known type of exercise-induced acute renal failure known as ALPE.
We performed a database search selecting papers published in the English or Japanese language. A database search was lastly accessed on 1 September 2022. The results of this study were compared with those reported in other case series.
The study evaluated renal hypouricemia as a key risk factor of ALPE. The development of ALPE is due to the sum of risk factors such as exercise, hypouricemia, nonsteroidal anti-inflammatory drugs, vasopressors, and dehydration.
Hypouricemia plays a key role in the development of ALPE and is often associated with anaerobic exercise. The development of ALPE is a result of the cumulative effects of risk factors such as exercise, hypouricemia, NSAIDs, vasopressors, and dehydration.
The information in this paper can help clinicians make more accurate diagnosis, given that a significant proportion of patients with ALPE are undiagnosed. Further, this paper can increase awareness among athletes to help them prevent ALPE and reach their exercise goals.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Pediatrics
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gadelkareem RA, Egypt; Jain R, India S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Ishikawa I. Acute renal failure with severe loin pain and patchy renal vasoconstriction. Eliahou HE, ed. Acute Renal Failure, John Libbey & Company, London. 1982; 224-229. |
| 2. | Gundlapalli S, Gaur Y, Rao MV, Bande SR, Sandhya P. Renal Hypouricemia with Exercise Induced Acute Kidney Injury-A Case Report. Indian J Nephrol. 2021;31:307-310. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Aomura D, Sonoda K, Harada M, Hashimoto K, Kamijo Y. A Case of Acute Kidney Injury in a Patient with Renal Hypouricemia without Intense Exercise. Case Rep Nephrol Dial. 2020;10:26-34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Shimizu Y, Wakabayashi K, Totsuka A, Hayashi Y, Nitta S, Hara K, Akira M, Tomino Y, Suzuki Y. Exercise-Induced Acute Kidney Injury in a Police Officer with Hereditary Renal Hypouricemia. Case Rep Nephrol Dial. 2019;9:92-101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Furuto Y, Kawamura M, Namikawa A, Takahashi H, Shibuya Y, Mori T, Sohara E. Non-urate transporter 1, non-glucose transporter member 9-related renal hypouricemia and acute renal failure accompanied by hyperbilirubinemia after anaerobic exercise: a case report. BMC Nephrol. 2019;20:433. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Maekawa M, Imaizumi T, Yamakawa T, Ito Y. Acute Renal Failure with Severe Loin Pain and Patchy Renal Vasoconstriction in a Patient without Hypouricemia, Provoked by Epileptic Seizure. Intern Med. 2017;56:2001-2005. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Shimizu Y, Takaori K, Maeda S. Exercise-induced acute renal failure in a trainee cyclist without hypouricemia: Successful athletic career post-treatment. J Gen Fam Med. 2017;18:432-435. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Shen H, Feng C, Jin X, Mao J, Fu H, Gu W, Liu A, Shu Q, Du L. Recurrent exercise-induced acute kidney injury by idiopathic renal hypouricemia with a novel mutation in the SLC2A9 gene and literature review. BMC Pediatr. 2014;14:73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Chakraborty S, Sural S. A young patient of hereditary renal hypouricaemia presenting with exercise-induced rhabdomyolysis and acute kidney injury. Ann Clin Biochem. 2013;50:271-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Saito O, Sugase T, Saito T, Akimoto T, Inoue M, Ando Y, Muto S, Kusano E. Two cases of renal hypouricemia in which dopamine infusion produced a good recovery from exercise-induced acute kidney injury. Clin Nephrol. 2011;76:83-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Yan MT, Cheng CJ, Chen JS, Lin SH. The case: a young man with acute kidney injury after exercise. The diagnosis: exercise induced acute kidney injury in hereditary renal hypouricemia. Kidney Int. 2010;77:935-936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Sugimoto T, Ide R, Uzu T, Kashiwagi A. Recurring exercise-induced acute renal failure with usual daily work. Nephrology (Carlton). 2007;12:110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Ishikawa I, Sakurai Y, Masuzaki S, Sugishita N, Shinoda A, Shikura N. Exercise-induced acute renal failure in 3 patients with renal hypouricemia. Nihon Jinzo Gakkai Shi. 1990;32:923-928. [DOI] [Full Text] |
| 14. | Erley CM, Hirschberg RR, Hoefer W, Schaefer K. Acute renal failure due to uric acid nephropathy in a patient with renal hypouricemia. Klin Wochenschr. 1989;67:308-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 47] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Harumasa Y, Masayoshi M, Toshinaga Y. A case of posterior reversible encephalopathy syndrome caused by acute renal failure with severe loin pain and patchy renal ischemia after anaerobic exercise. J Jpn Soc Intensive Care Med. 2013;20:405-409. [DOI] [Full Text] |
| 16. | Tamura Y, Kudo E, Shima T, Ueda S, Yano H, Arai S, Kato H, Fujimori S, Uchida S, Hosoyamada H, Kaneko K, Ichida K. A case of acute renal failure with renal hypouricemia after Exercise. Gout and Nucleic Acid Metabolism. 2013;37:48-49. [DOI] [Full Text] |
| 17. | Karasawa T, Ikezumi Y, Suzuki T, Hasegawa H, Uchiyama M. Oxidative Imbalance in Acute Renal Failure after Exercise without Renal Hypouricemia. JJN. 2010;23:12-17. [DOI] [Full Text] |
| 18. | Araki H, Takaya K. A case of acute renal failure with severe loin pain and patchy renal ischemia after anaerobic exercise in a patient with hypouricemia and mutation in the gene encoding uric acid transporter 1. Journal of Japanese Society for Dialysis Therapy. 2020;43:1005-1010. [DOI] [Full Text] |
| 19. | Takewa R, Taniguti N, Tanaka S. Mechanisms of exercise-induced acute renal failure in idiopathic renal hypouricemia: a case report and a review of the literature. JJN. 2009;22:57-61. [DOI] [Full Text] |
| 20. | Ichida K. Hypouricemia with recurrent acute renal failure. Hyperuricemia and Gout. 2008;16: 68-71. |
| 21. | Sudo H, Tuji M, Unishi G. Exercise-induced acute renal failure in a boy with renal hypouricemia. Japanese Journal of Pediatric Nephrology 2000; 13: 33-37. [DOI] [Full Text] |
| 22. | Takeda Y, Fujimoto T, Uyama H, Shiiki H, Yamano S, Kanauchi M, Yabuta M, Dohi K. [Two cases of exercise-induced acute renal failure with idiopathic renal hypouricemia]. Nihon Jinzo Gakkai Shi. 2001;43:384-388. [PubMed] |
| 23. | Hisanaga S, Ueno N, Inagaki H, Tokura T, Uezono S, Yokota N, Fujimoto S, Eto T. [Exercise-induced acute renal failure associated with renal vasoconstriction]. Nihon Jinzo Gakkai Shi. 1999;41:406-412. [PubMed] |
| 24. | Oi K, Ichida H, Okabe H, Kato N, Nakamura H, Kubo H, Kawamura T, Hosoya T, Shiro K. [Case of renal hypouricemia causing exercise-induced acute renal failure]. Nihon Naika Gakkai Zasshi. 1998;87:732-734. [PubMed] [DOI] [Full Text] |
| 25. | Tazawa M, Morooka M, Takeichi S, Minowa S, Yasaki T. [Exercise-induced acute renal failure observed in a boy with idiopathic renal hypouricemia caused by postsecretary reabsorption defect of uric acid]. Nihon Jinzo Gakkai Shi. 1996;38:407-412. [PubMed] |
| 26. | Numabe A, Tsukada H, Sugimoto T, Ono H, Hirao S, Abe M, Yagi S. [A case of acute renal failure in a patient with idiopathic hypouricemia]. Nihon Jinzo Gakkai Shi. 1992;34:841-845. [PubMed] |
| 27. | Ishikawa I, Sakurai Y, Masuzaki S, Sugishita N, Shinoda A, Shikura N. Exercise-induced acute renal failure in 3 patients with renal hypouricemia. Nihon Jinzo Gakkai Shi. 1990;32:923-928. [PubMed] |
| 28. | Sakurauchi Y, Tsuyuki M, Okazaki Y, Sugiyama T, Yamamoto T. A case of acute renal failure in patient with idiopathic hypouricemia. Kidney and Dialysis. 1990; 29: 125-128. |
| 29. | Lee J, Lee SW, Lee JW, Chin HJ, Joo KW, Kim YS, Ahn C, Kim S, Cho JY, Han JS. Clinical characteristics of acute renal failure with severe loin pain and patchy renal vasoconstriction. Kidney Res Clin Pract. 2012;31:170-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Ishikawa I. Acute renal failure with severe loin pain and patchy renal ischemia after anaerobic exercise in patients with or without renal hypouricemia. Nephron. 2002;91:559-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 74] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 31. | Ohta T, Sakano T, Igarashi T, Itami N, Ogawa T; ARF Assocoated with Renal Hypouricemia Research Group. Exercise-induced acute renal failure associated with renal hypouricaemia: results of a questionnaire-based survey in Japan. Nephrol Dial Transplant. 2004;19:1447-1453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 77] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 32. | Ishikawa I. Post-exercise acute kidney injury. The Journal of the Japanese Society of Internal Medicine. 2014;103:1101-1107. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | Ishikawa I. Exercise-Induced Acute Renal Failure. The Journal of the Japanese Society of Internal Medicine. 2010;99:970-976. [DOI] [Full Text] |
| 34. | Ishikawa I. Exercise-Induced Acute Renal Failure-Acute Renal Failure with Severe Loin Pain and Patchy Renal Ischemia after Anaerobic Exercise, Springer Japan, Tokyo. 2007; 1-108. [DOI] [Full Text] |
| 35. | Enomoto A, Kimura H, Chairoungdua A, Shigeta Y, Jutabha P, Cha SH, Hosoyamada M, Takeda M, Sekine T, Igarashi T, Matsuo H, Kikuchi Y, Oda T, Ichida K, Hosoya T, Shimokata K, Niwa T, Kanai Y, Endou H. Molecular identification of a renal urate anion exchanger that regulates blood urate levels. Nature. 2002;417:447-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1027] [Cited by in RCA: 1069] [Article Influence: 46.5] [Reference Citation Analysis (0)] |
| 36. | Murakami T, Kawakami H, Fukuda M, Furukawa S. Patients with renal hypouricemia are prone to develop acute renal failure--why? Clin Nephrol. 1995;43:207-208. [PubMed] |
| 37. | Ames BN, Cathcart R, Schwiers E, Hochstein P. Uric acid provides an antioxidant defense in humans against oxidant- and radical-caused aging and cancer: a hypothesis. Proc Natl Acad Sci USA. 1981;78:6858-6862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1824] [Cited by in RCA: 1946] [Article Influence: 44.2] [Reference Citation Analysis (0)] |
| 38. | Araujo M, Wilcox CS. Oxidative stress in hypertension: role of the kidney. Antioxid Redox Signal. 2014;20:74-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 149] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 39. | Fujinaga S, Ito A, Nakagawa M, Watanabe T, Ohtomo Y, Shimizu T. Posterior reversible encephalopathy syndrome with exercise-induced acute kidney injury in renal hypouricemia type 1. Eur J Pediatr. 2013;172:1557-1560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 40. | Ishikawa I, Nakagawa M, Hayama S, Yoshida S, Date T. Acute renal failure with severe loin pain and patchy renal ischaemia after anaerobic exercise (ALPE) (exercise-induced acute renal failure) in a father and child with URAT1 mutations beyond the W258X mutation. Nephrol Dial Transplant. 2005;20:1015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 41. | Radaković M, Borozan S, Djelić N, Ivanović S, Miladinović DĆ, Ristanić M, Spremo-Potparević B, Stanimirović Z. Nitroso-Oxidative Stress, Acute Phase Response, and Cytogenetic Damage in Wistar Rats Treated with Adrenaline. Oxid Med Cell Longev. 2018;2018:1805354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |